Making Clinical Governance Work for You
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Intended and Unintended Outcomes of New Governance Arrangements Within the NHS
SDO Project (08/1618/129) The intended and unintended outcomes of new governance arrangements within the NHS Report for the National Institute for Health Research Service Delivery and Organisation programme March 2010 Professor John Storey, The Open University Business School Dr Richard Holti, The Open University Business School Dr Nik Winchester, The Open University Business School Professor Rod Green, Department of Management, The University of Bath Professor Graeme Salaman, The Open University Business School Professor Paul Bate, University College, London ____________________________________ Project Lead: Professor John Storey, Open University Business School Walton Hall, Milton Keynes, MK7 6AA E-mail: [email protected] © Queen’s Printer and Controller of HMSO 2010 1 SDO Project (08/1618/129) Contents Acknowledgements ....................................................5 Executive Summary....................................................6 Background ..............................................................................6 Aims........................................................................................6 About this study ........................................................................7 Key findings..............................................................................7 Conclusions ..............................................................................9 PART 1: POSITIONING THE STUDY...........................11 1 Introduction and background...........................11 1.1 The governance and -
Risk Management Review
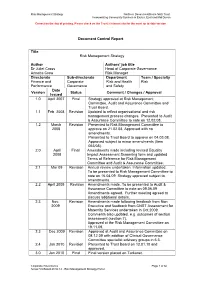
Risk Management Strategy Northern Devon Healthcare NHS Trust Incorporating Community Services in Exeter, East and Mid Devon Correct on the day of printing. Please check on the Trust’s internet site for the most up to date version Document Control Report Title Risk Management Strategy Author Authors’ job title Dr Juliet Cross Head of Corporate Governance Annette Crew Risk Manager Directorate Sub-directorate Department Team / Specialty Finance and Corporate Risk and Health Risk Performance Governance and Safety Date Version Status Comment / Changes / Approval Issued 1.0 April 2007 Final Strategy approved at Risk Management Committee, Audit and Assurance Committee and Trust Board. 1.1 Feb. 2008 Revision Updated to reflect organisational and risk management process changes. Presented to Audit & Assurance Committee to note on 12.02.08. 1.2 March Revision Presented to Risk Management Committee to 2008 approve on 21.02.08. Approved with no amendments. Presented to Trust Board to approve on 04.03.08. Approved subject to minor amendments (Item 053/08). 2.0 April Final Amendments made including revised Equality 2008 Impact Assessment Screening form and updated Terms of Reference for Risk Management Committee and Audit & Assurance Committee. 2.1 Mar 09 Revision Annual review undertaken. Information updated. To be presented to Risk Management Committee to note on 16.04.09. Strategy approved subject to amendments. 2.2 April 2009 Revision Amendments made. To be presented to Audit & Assurance Committee to note on 09.06.09 Amendments agreed. Further meeting agreed to discuss additional details. 2.3 Nov. Revision Amendments made following feedback from Non 2009 Executive and feedback from CNST Assessment for Maternity Services undertaken in Oct.2009. -

Clinical Governance: the Next Hype?
Maltese Medical Journal, 2000; 12(1,2): 31 31 All rights reserved Clinical Governance: the next hype? Marie-Klaire Farrugia * *Senior House Officer, Department of Orthopaedics and Trauma Correspondence: Dr M K Farrugia, E-mail: [email protected] Introduction Evidence Based Practice The recent wave of strategies geared at improving the Evidence Based Practice is about basing one's quality of the NHS and combating medicolegal actions practice on the best accepted evidence to date. This in the UK has resulted in the accumulation of a number requires a basic infrastructure which will provide this of hyped-up terms, the latest of which is Clinical continuously-updated information. It entails information Governance. Clinical Governance is to be the main technology which will enable access to specialist vehicle for continuously improving the quality of databases such as the Cochrane Collaboration (www. patient care and developing the capacity to maintain cochrane.co.uk) and facilitated access to updated high standards. libraries4. As from June 1999, the British Health Act has placed a duty on each primary care trust and each NHS trust to Audit make arrangements for the purpose of monitoring and improving the quality of healthcare provided to patients. Assessing whether one's practice is actually up to the A recent update of the NHS Plan (www.nhs.uk! required standard relies on audit. All clinicians in the nationalplan/nhsplan.htm), published in July 2000, UK are now expected to participate in audit programs, explains how this move is to be governed by the and there is greater emphasis on evidence-based National Institute for Clinical Excellence (NICE) practice and adherence to national frameworks and www.nice.org.uk - which will set standards and recommendations made by the NICE. -

Clinical Audit: a Simple Guide for NHS Boards & Partners
Clinical audit: A simple guide for NHS Boards & partners Authors: Dr. John Bullivant, Director, Good Governance Institute (GGI) Good Governance Andrew Corbett-Nolan, Institute Chair, Institute of Healthcare Management (IHM) Contents Executive summary Executive summary 3 Whilst this guide is specifically about clinical audit, much of what • Delivers a return on investment. is described here is relevant to the way in which NHS Boards can • Improvements are implemented and sustained. 1. Clinical audit: Ten simple rules for NHS Boards 5 monitor clinical quality as a whole within the context of clinical or integrated governance. A PCT has specific responsibilities in relation to clinical audit that 2. Foreword 7 should be managed through the Professional Executive Clinical audit has been endorsed by the Department of Health in Committee (PEC) or an equivalent committee. 3. Clinical audit as part of the modern healthcare system 9 successive strategic documents as a significant way in which the quality of clinical care can be measured and improved. Originally, Boards should use clinical audit to confirm that current practice 4. Definitions and types of clinical quality review 11 clinical audit was developed as a process by which clinicians compares favourably with evidence of good practice and to reviewed their own practice. However, clinical audit is now 5. The importance and relationship of clinical audit to clinical ensure that where this is not the case that changes are made recognised as an effective mechanism for improving the quality that improve the delivery of care. governance, NHS Boards and their partner organisations 15 of care patients receive as a whole. -

GOVERNING MEDICINE Theory and Practice EDITED by Andrew Gray & Stephen Harrison G “Gray and Harrison Have Assembled an Impressive Array of Authors to Analyse The
GOVERNING MEDICINE Theory and Practice EDITED BY Andrew Gray & Stephen Harrison G “Gray and Harrison have assembled an impressive array of authors to analyse the changing role of the medical profession. The contributions range from historical OVERNING analyses of the relationship between government and doctors, to detailed examination of the implementation of clinical governance in the NHS. All offer important insights into an issue that lies at the heart of contemporary debates in health policy.” CHRIS HAM, PROFESSOR OF HEALTH POLICY AND MANAGEMENT, UNIVERSITY OF BIRMINGHAM This book brings together a range of detailed explorations of the theory, practice and prospects of clinical governance by some of the most eminent practitioners and researchers in the United Kingdom. Since New Labour’s institution of clinical governance through its White Paper in 1997, there has been a good deal of M debate about the history, theory and practice of clinical governance and the governance of clinical care. EDICINE Divided into three parts, the book focuses on the core areas of: N Medicine, Autonomy and Governance N Evidence, Science and Medicine N Realizing Clinical Governance Starting with the differing definitions of the term clinical governance, the contributors discuss the relationship of medicine and governance, the challenges that evidence-based medicine makes upon clinical practice and move on to suggest possible futures for clinical governance. Written by a team of experienced academics and practitioners, this book is aimed at reflective health professionals, as well as students and academics in the fields of health policy, health services management, social policy and public policy. Gray & Harrison Cover design Hybert Design GOVERNING Andrew Gray is Emeritus Professor of Public Sector Management and Visiting Professorial Fellow at the Centre for Clinical Management at the University of Durham. -

Clinical Governance Principles for Pharmacy Services 2018
Clinical Governance Principles for Pharmacy Services 2018 PSA Australia’s peak body for pharmacists © Pharmaceutical Society of Australia 2018 This publication contains material that has been provided by the Pharmaceutical Society of Australia (PSA), and may contain material provided by the Commonwealth and third parties. Copyright in material provided by the Commonwealth or third parties belong to them. PSA owns the copyright in the publication as a whole and all material in the guide that has been developed by PSA. In relation to PSA owned material, no part may be reproduced by any process except in accordance with the provisions of the Copyright Act 1968 (Cth), or the written permission of PSA. Requests and inquiries regarding permission to use PSA material should be addressed to: Pharmaceutical Society of Australia, PO Box 42, Deakin West ACT 2600. Where you would like to use material that has been provided by the Commonwealth or third parties, contact them directly. The development of the Clinical Governance Principles for Pharmacy Services has been funded by the Australian Government Department of Health. This work has been informed by experts, consultation and stakeholder feedback. The Pharmaceutical Society of Australia (PSA) thanks all those involved in the development of this document and in particular, gratefully acknowledges the feedback and input received from the following organisations: • Australian Government Department of Health • Australian Commission on Safety and Quality in Health Care • The Society of Hospital Pharmacists -

Cultivating Accountability for Health Systems Strengthening
. Cultivating Accountability for health systems strengthening Series of Guides for Enhanced Governance of the Health Sector and Health Institutions in Low- and Middle-Income Countries JUNE 2014 Cultivating Accountability for Health Systems Strengthening 3 Table of Contents Acknowledgements . 4 Introduction . 5 Purpose and Audience for the Guides . 6 Governing Practice—Cultivating Accountability . 8 Your Personal Accountability . 10 Accountability of Your Organization to its Stakeholders . 11 Internal Accountability in Your Organization . 12 Accountability of Health Providers and Health Workers . 13 Managing Performance . 14 Sharing Information . 15 Developing Social Accountability . 17 Using Technology to Support Accountability . 20 Smart Oversight . 21 Appendix: Transparency and Accountability Tools . .. 22 Accreditation . 22 Community Scorecard . 22 Citizen Report Cards . 23 Participatory Budgeting . 23 Independent Budget Analysis . 24 Public Expenditure Tracking Survey . 24 Social Audit .. 24 Citizen’s Charter . 24 Public Hearings . 24 E-Governance . 25 Community Radio . 25 Community-Based Monitoring of Primary Healthcare Providers in Uganda . 26 References and Resources . 27 Transparency . 27 Accountability . 27 Want To Learn More? . 28 Funding was provided by the United States Agency for International Development (USAID) under Cooperative Agreement AID-OAA-A-11-00015. The contents are the responsibility of the Leadership, Management, and Governance Project and do not necessarily reflect the views of USAID or the United States Government. 4 Cultivating Accountability for Health Systems Strengthening Acknowledgements This work was funded by the United States Agency for International Development (USAID) through the Leadership, Management, and Governance (LMG) Project . The LMG Project team thanks the staff of the USAID Office of Population and Reproductive Health, in particular, the LMG Project Agreement Officer’s Representative and her team for their constant encouragement and support . -

Introduction to Clinical Governance – a Background Paper NO
INFORMATION SERIES NO. 1.1 Introduction to Clinical Governance – A Background Paper NO. 1.1 NO. ACKNOWLEDGEMENTS The Office of Safety and Quality in Health Care acknowledges and appreciates the input of all individuals and groups who have contributed to the development of this background paper. In particular, the Office of Safety and Quality in Health Care would like to recognise the valuable contribution of members of the Western Australian Council for Safety and Quality in Health Care for their guidance and support. The Office of Safety and Quality in Health Care will undertake further consultation with the metropolitan Area Health Services and Country Health Service Regions to ensure the implementation of the WA Clinical Governance policy at the local level. The Western Australian Council for Safety and Quality in Health Care will provide a leadership role in monitoring and evaluating the implementation of the Policy by hospitals and health services across the Western Australian health system to ensure the delivery of consumer-focused, safe, quality health care in Western Australia. Table of Contents 1 CLINICAL GOVERNANCE: BACKGROUND PAPER 2 WHERE HAS CLINICAL GOVERNANCE COME FROM? 3 DO WE REALLY NEED CLINICAL GOVERNANCE? 3 1. THE VIEW FROM INSIDE 3 2. WHAT DOES THE PUBLIC SEE? 4 HOW ARE INTERNATIONAL HEALTH SYSTEMS RESPONDING? 5 WHAT DOES CLINICAL GOVERNANCE INCLUDE? 6 1. CLINICAL AUDIT 6 2. CLINICAL RISK MANAGEMENT 7 3. PROFESSIONAL DEVELOPMENT AND MANAGEMENT 7 WHAT ARE THE BARRIERS? 8 CONCLUSION 9 Introduction to Clinical Governance 2 Clinical Governance: Background paper constantly strive to do their best for their patients, but in an imperfect and sometimes inadequate environment. -

Report on the Economics of Patient Safety in Primary and Ambulatory
THE ECONOMICS OF PATIENT SAFETY IN PRIMARY AND AMBULATORY CARE Flying blind The Economics of Patient Safety in Primary and Ambulatory Care Flying blind 1 │ This work is published under the responsibility of the Secretary-General of the OECD. The opinions expressed and arguments employed herein do not necessarily reflect the official views of OECD member countries. This document and any map included herein are without prejudice to the status of or sovereignty over any territory, to the delimitation of international frontiers and boundaries and to the name of any territory, city or area. The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law. The Economics of Patient Safety in Primary and Ambulatory Care © OECD 2018 2 │ Table of Contents Acknowledgements ................................................................................................................................ 3 Key messages .......................................................................................................................................... 4 1. Introduction ....................................................................................................................................... 6 1.1. This report makes the economic case for safety in the primary and ambulatory care sector ........ 8 1.2. Safety -

Clinical Governance
CLINICAL GOVERNANCE A STUDY OF IMPLEMENTATION; A STUDY OF CHANGE by LINDA ANN LATHAM A thesis submitted to The Faculty of Commerce and Social Science The University of Birmingham for the degree of DOCTOR OF PHILOSOPHY Health Services Management Centre University of Birmingham Birmingham B152TT February 2003 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. o ao (A) ABSTRACT The concept of clinical governance was first introduced to the National Health Service in the White Paper published in 1997 (Department of Health); it has been described as the 'linchpin' of the quality reforms and, as of April 1999, is one of the statutory duties placed on NHS Trust Boards. Clinical governance is defined as: 'A framework through which NHS organisations are accountable for continuously improving the quality if their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish.' (Department of Health, 1998; p33). The research project upon which this thesis is based took place over an 18 month period and has followed one NHS Trust as it implemented this new policy. -
System Governance Towards Improved Patient Safety
SYSTEM GOVERNANCE TOWARDS IMPROVED PATIENT SAFETY Key Functions, Approaches and Pathways to Implementation 1 SYSTEM GOVERNANCE TOWARDS IMPROVED PATIENT SAFETY KEY FUNCTIONS, APPROACHES AND PATHWAYS TO IMPLEMENTATION SYSTEM GOVERNANCE TOWARDS IMPROVED PATIENT SAFETY © OECD 2020 2 Copyright page This document and any map included herein are without prejudice to the status of or sovereignty over any territory, to the delimitation of international frontiers and boundaries and to the name of any territory, city or area. The statistical data for Israel are supplied by and under the responsibility of the relevant Israeli authorities. The use of such data by the OECD is without prejudice to the status of the Golan Heights, East Jerusalem and Israeli settlements in the West Bank under the terms of international law. © OECD 2020 SYSTEM GOVERNANCE TOWARDS IMPROVED PATIENT SAFETY © OECD 2020 3 Acknowledgements This report was produced by the OECD for the 5th Global Ministerial Summit on Patient Safety, which was scheduled to take place in Montreux, Switzerland on the 27th and 28th of February 2020. The work was enabled by a voluntary contribution from the Swiss Federal Office of Public Health. The authors of this report are Ane Auraaen, Kristin Saar and Niek Klazinga. The authors would like to thank the Swiss Federal Office of Public Health and Dr Anthony Staines for valuable support and collaboration during the planning of the Global Ministerial Summit on Patient Safety and drafting of the report. Many thanks also to Pr. Jeffrey Braithwaite, Dr. Ingo Häertel and Dr. Ernest Konadu Asiedu for their insightful feedback and guidance in this process Authors would like to acknowledge and warmly thank the survey respondents and the patient safety governance experts who participated to in-depth interviews during the drafting process of this report. -

The Quality of GP Diagnosis and Referral Catherine Foot Chris Naylor Candace Imison
Research paper The quality of GP diagnosis Authors Catherine Foot and referral Chris Naylor Candace Imison An Inquiry into the Quality of General Practice in England The quality of GP diagnosis and referral Catherine Foot Chris Naylor Candace Imison This paper was commissioned by The King’s Fund to inform the Inquiry panel. The views expressed are those of the authors and not of the panel. Contents Executive summary 3 1 Introduction 7 Context 7 Methods 9 2 The quality of diagnosis in general practice in England 11 What is the role of general practice in diagnosis? 11 High-quality diagnosis in general practice – what does it look like? 13 The current quality of diagnosis in general practice 15 Approaches towards quality improvement 22 Key messages 25 3 The quality of referral in general practice in England 27 What is a GP referral? 27 High-quality referral – what does it look like? 27 The quality of current GP referral practices 32 Approaches towards quality improvement in referral 45 Key messages 48 4 Discussion and conclusions 50 Key findings 50 Recommendations for approaches to improvement 51 Potential quality measures 52 Conclusion 54 Appendices Appendix A: Effective interventions 55 Appendix B: Case study 57 Appendix C: Search terms used in literature review 62 References 63 2 The King’s Fund 2010 Executive summary This report forms part of the wider inquiry into the quality of general practice in England commissioned by The King’s Fund, and focuses specifically on the quality of diagnosis and referral. The report: ■ describes what ‘good’ looks like for diagnosis and referral within primary care ■ describes what is known about the current quality of referral and diagnosis in general practice ■ identifies evidence-based means of improving the quality of GP diagnosis and referral ■ considers the potential for quality measures of diagnosis and referral within primary care.