Limits to Our Understanding Eric S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Applied Category Theory for Genomics – an Initiative
Applied Category Theory for Genomics { An Initiative Yanying Wu1,2 1Centre for Neural Circuits and Behaviour, University of Oxford, UK 2Department of Physiology, Anatomy and Genetics, University of Oxford, UK 06 Sept, 2020 Abstract The ultimate secret of all lives on earth is hidden in their genomes { a totality of DNA sequences. We currently know the whole genome sequence of many organisms, while our understanding of the genome architecture on a systematic level remains rudimentary. Applied category theory opens a promising way to integrate the humongous amount of heterogeneous informations in genomics, to advance our knowledge regarding genome organization, and to provide us with a deep and holistic view of our own genomes. In this work we explain why applied category theory carries such a hope, and we move on to show how it could actually do so, albeit in baby steps. The manuscript intends to be readable to both mathematicians and biologists, therefore no prior knowledge is required from either side. arXiv:2009.02822v1 [q-bio.GN] 6 Sep 2020 1 Introduction DNA, the genetic material of all living beings on this planet, holds the secret of life. The complete set of DNA sequences in an organism constitutes its genome { the blueprint and instruction manual of that organism, be it a human or fly [1]. Therefore, genomics, which studies the contents and meaning of genomes, has been standing in the central stage of scientific research since its birth. The twentieth century witnessed three milestones of genomics research [1]. It began with the discovery of Mendel's laws of inheritance [2], sparked a climax in the middle with the reveal of DNA double helix structure [3], and ended with the accomplishment of a first draft of complete human genome sequences [4]. -

Masthead (PDF)
Proceedings of the National Academy ofPNAS Sciences of the United States of America www.pnas.org PRESIDENT OF Robert G. Roeder Geophysics John J. Mekalanos THE ACADEMY Michael Rosbash Michael L. Bender Peter Palese Ralph J. Cicerone David D. Sabatini Thomas E. Shenk Gertrud M. Schupbach Human Environmental Thomas J. Silhavy SENIOR EDITOR Robert Tjian Sciences Peter K. Vogt Solomon H. Snyder Susan Hanson Cellular and Molecular Physics ASSOCIATE EDITORS Neuroscience Immunology Anthony Leggett William C. Clark Pietro V. De Camilli Peter Cresswell Paul C. Martin Alan Fersht Richard L. Huganir Douglas T. Fearon Jack Halpern L. L. Iversen Richard A. Flavell Physiology and Jeremy Nathans Charles F. Stevens Dan R. Littman Pharmacology Thomas C. Su¨dhof Tak Wah Mak Susan G. Amara Joseph S. Takahashi William E. Paul David Julius EDITORIAL BOARD Hans Thoenen Michael Sela Ramon Latorre Ralph M. Steinman Masashi Yanagisawa Animal, Nutritional, and Chemistry Applied Microbial Sciences Stephen J. Benkovic Mathematics Plant Biology David L. Denlinger Bruce J. Berne Richard V. Kadison Maarten J. Chrispeels R. Michael Roberts Harry B. Gray Robion C. Kirby Enrico Coen Robert Haselkorn Linda J. Saif Mark A. Ratner George H. Lorimer Ryuzo Yanagimachi Barry M. Trost Medical Genetics, Hematology, and Nicholas J. Turro Anthropology Oncology Plant, Soil, and Charles T. Esmon Microbial Sciences Jeremy A. Sabloff Computer and Joseph L. Goldstein Roger N. Beachy Information Sciences Mark T. Groudine Steven E. Lindow Applied Mathematical Sciences Shafrira Goldwasser David O. Siegmund Tony Hunter M. S. Swaminathan Philip W. Majerus Susan R. Wessler Economic Sciences Newton E. Morton Applied Physical Sciences Ronald W. -

CURRICULUM VITAE George M. Weinstock, Ph.D
CURRICULUM VITAE George M. Weinstock, Ph.D. DATE September 26, 2014 BIRTHDATE February 6, 1949 CITIZENSHIP USA ADDRESS The Jackson Laboratory for Genomic Medicine 10 Discovery Drive Farmington, CT 06032 [email protected] phone: 860-837-2420 PRESENT POSITION Associate Director for Microbial Genomics Professor Jackson Laboratory for Genomic Medicine UNDERGRADUATE 1966-1967 Washington University EDUCATION 1967-1970 University of Michigan 1970 B.S. (with distinction) Biophysics, Univ. Mich. GRADUATE 1970-1977 PHS Predoctoral Trainee, Dept. Biology, EDUCATION Mass. Institute of Technology, Cambridge, MA 1977 Ph.D., Advisor: David Botstein Thesis title: Genetic and physical studies of bacteriophage P22 genomes containing translocatable drug resistance elements. POSTDOCTORAL 1977-1980 Postdoctoral Fellow, Department of Biochemistry TRAINING Stanford University Medical School, Stanford, CA. Advisor: Dr. I. Robert Lehman. ACADEMIC POSITIONS/EMPLOYMENT/EXPERIENCE 1980-1981 Staff Scientist, Molec. Gen. Section, NCI-Frederick Cancer Research Facility, Frederick, MD 1981-1983 Staff Scientist, Laboratory of Genetics and Recombinant DNA, NCI-Frederick Cancer Research Facility, Frederick, MD 1981-1984 Adjunct Associate Professor, Department of Biological Sciences, University of Maryland, Baltimore County, Catonsville, MD 1983-1984 Senior Scientist and Head, DNA Metabolism Section, Lab. Genetics and Recombinant DNA, NCI-Frederick Cancer Research Facility, Frederick, MD 1984-1990 Associate Professor with tenure (1985) Department of Biochemistry -
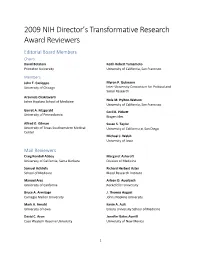
2009 NIH Director's Transformative Research Award Reviewers
2009 NIH Director’s Transformative Research Award Reviewers Editorial Board Members Chairs David Botstein Keith Robert Yamamoto Princeton University University of California, San Francisco Members John T. Cacioppo Myron P. Gutmann University of Chicago Inter-University Consortium for Political and Social Research Aravinda Chakravarti Johns Hopkins School of Medicine Nola M. Hylton-Watson University of California, San Francisco Garret A. Fitzgerald Cecil B. Pickett University of Pennsylvania Biogen Idec Alfred G. Gilman Susan S. Taylor University of Texas Southwestern Medical University of California at San Diego Center Michael J. Welsh University of Iowa Mail Reviewers Craig Kendall Abbey Margaret Ashcroft University of California, Santa Barbara Division of Medicine Samuel Achilefu Richard Herbert Aster School of Medicine Blood Research Institute Manuel Ares Arleen D. Auerbach University of California Rockefeller University Bruce A. Armitage J. Thomas August Carnegie Mellon University Johns Hopkins University Mark A. Arnold Kevin A. Ault University of Iowa Emory University School of Medicine David C. Aron Jennifer Bates Averill Case Western Reserve University University of New Mexico 1 Mary Helen Barcellos-Hoff Leslie A. Bruggeman New York University School of Medicine Case Western Reserve University David P. Bartel Peter Burkhard New Cambrige Center University of Connecticut Ralf Bartenschlager Alma L. Burlingame University of Heidelberg University of California, San Francisco Rashid Bashir Frederic D. Bushman University of Illinois at Urbana – Champaign University of Pennsylvania Carl A. Batt Robert William Caldwell Cornell University Medical College of Georgia Mark T. Bedford Phil Gordon Campbell Research Division Carnegie Mellon University Kevin D. Belfield Joseph Nicholas Cappella University of Central Florida University of Pennsylvania Andrew Steven Belmont William A. -

The Path to New Therapies for Schizophrenia and Bipolar Illness
THE JOURNAL • PERSPECTIVE • www.fasebj.org The Path to New Therapies for Schizophrenia and Bipolar Illness Edward M. Scolnick1 Stanley Center for Psychiatric Research, Broad Institute, Cambridge, Massachusetts, USA ABSTRACT: Schizophrenia and bipolar illness are two of the most serious forms of mental illness. Until relatively recently, almost nothing was known about the molecular pathogenesis of either illness. The single largest risk factor that predisposes people to schizophrenia or bipolar illness is genetic risk. Heritability is high, and the incidence is significantly higher in identical twins than in nonidentical twins. Despite decades of work aimed at identifying the genes involved in these two illnesses, virtually no progress had been made until the past decade. With the knowledge and technologies that have been gained from the Human Genome Project, it has been possible to begin to understand the underlying genetics and to use the new information to begin the effort to discover new and better medicines to treat these illnesses. This article will describe the past decade of work toward this goal and articulate both the promise that now exists and what is still needed to bring dramatic and tangible change to patients.—Scolnick, E. M. The path to new therapies for schizophrenia and bipolar illness. FASEB J. 31, 1254–1259 (2017). www.fasebj.org KEY WORDS: genetics • pharmacology • progress In the fall of 2004, I became an associate member of the bipolar illness for many years. Virtually no reproducible Broad Institute, founded on the principle of collaboration results had been achieved. The Broad Institute had a su- among scientists at the Massachusetts Institute of Tech- perb group of scientific experts in human genetics, a field nology, Harvard, and Harvard-affiliated hospitals. -

Molecular and Cellular Biology Volume 8 May 1988 Number 5
MOLECULAR AND CELLULAR BIOLOGY VOLUME 8 MAY 1988 NUMBER 5 Aaron J. Shatkin, Editor in Chief(1990) Randy W. Schekman, Editor Joan A. Steitz, Editor (1990) Center for Advanced (1992) Yale University Biotechnology and Medicine University of California New Haven, Conn. Piscataway, N.J. Berkeley Robert Tjian, Editor (1991) David J. L. Luck, Editor (1992) Louis Siminovitch, Editor (1990) University of California Rockefeller University Mount Sinai Hospital Berkeley New York, N.Y. Toronto, Canada Harold E. Varmus, Editor (1989) Steven L. McKnight, Editor (1992) University of California Carnegie Institution of Washington San Francisco Baltimore, Md. EDITORIAL BOARD Frederick W. Alt (1990) Michael Green (1988) Douglas Lowy (1990) Matthew P. Scott (1989) Susan Berget (1990) Jack F. Greenblatt (1988) Paul T. Magee (1988) Fred Sherman (1988) Arnold J. Berk (1988) Leonard P. Guarente (1988) James Manley (1989) Arthur Skoultchi (1988) Alan Bernstein (1990) Christine Guthrie (1989) Janet E. Mertz (1990) Barbara Sollner-Webb (1989) Barbara K. Birshtein (1990) James E. Haber (1990) Robert L. Metzenberg (1988) Frank Solomon (1988) J. Michael Bishop (1990) Hidesaburo Hanafusa (1989) Robert K. Mortimer (1988) Karen Sprague (1989) Michael R. Botchan (1990) Leland D. Hartwell (1990) Bernardo Nadal-Ginard (1990) Pamela Stanley (1988) David Botstein (1990) Ari Helenius (1990) Paul Neiman (1989) Nat Sternberg (1989) Bruce P. Brandhorst (1990) Ira Herskowitz (1990) Joseph R. Nevins (1990) Bruce Stiliman (1988) James R. Broach (1988) James B. Hicks (1989) Carol Newlon (1988) Kevin Struhl (1989) Joan Brugge (1988) Alan Hinnebusch (1988) Mary Ann Osley (1990) Bill Sugden (1988) Mario R. Capecchi (1990) Michael J. Holland (1990) Brad Ozanne (1989) Lawrence H. -
David Botstein 2015 Book.Pdf
Princeton University HONORS FACULTY MEMBERS RECEIVING EMERITUS STATUS May 2015 The biographical sketches were written by colleagues in the departments of those honored. Copyright © 2015 by The Trustees of Princeton University 550275 Contents Faculty Members Receiving Emeritus Status 2015 Steven L. Bernasek .......................3 David Botstein...........................6 Erhan Çinlar ............................8 Caryl Emerson.......................... 11 Christodoulos A. Floudas ................. 15 James L. Gould ......................... 17 Edward John Groth III ...................20 Philip John Holmes ......................23 Paul R. Krugman .......................27 Bede Liu .............................. 31 Alan Eugene Mann ......................33 Joyce Carol Oates .......................36 Clarence Ernest Schutt ...................39 Lee Merrill Silver .......................41 Thomas James Trussell ...................43 Sigurd Wagner .........................46 { 1 } { 2 } David Botstein avid Botstein was educated at Harvard (A.B. 1963) and the D University of Michigan (Ph.D. 1967). He joined the faculty of the Massachusetts Institute of Technology, rising through the ranks from instructor to professor of genetics. In 1987, he moved to Genentech, Inc. as vice president–science, and, in 1990, he joined Stanford University’s School of Medicine, where he was chairman of the Department of Genetics. In July, 2003 he became director of the Lewis-Sigler Institute for Integrative Genomics and the Anthony B. Evnin ’62 Professor of Genomics at Princeton University. David’s research has centered on genetics, especially the use of genetic methods to understand biological functions. His early work in bacterial genetics contributed to the discovery of transposable elements in bacteria and an understanding of their physical structures and genetic properties. In the early 1970s, he turned to budding yeast (Saccharomyces cerevisiae) and devised novel genetic methods to study the functions of the actin and tubulin cytoskeletons. -

Celebrating Years of 60Science Welcome to the 60Th Anni- Versary Symposium of the Miller Institute
Celebrating Years of 60Science Welcome to the 60th Anni- versary Symposium of the Miller Institute. In an age of ever increasing special- ization, the Miller Institute stands apart as one of the very few enterprises to embrace all of Science as its purview. For 60 years the Miller Institute has provided generous sup- port to some of the lead- ing postdoctoral fellows in all fields of science, has supported extended visits from famous scientists from around the world, and has provided critical adminis- trative and teaching relief for Berkeley faculty at par- ticularly important points in their career. This grand tradition lives on, even in the face of ever-greater challenges, with a refresh- ing emphasis on clarity in cross-discipline communi- cation. We have assembled a panel of eight luminaries drawn from past and pres- ent members of the Miller Institute each of whom leads their field with cre- ative research at the fron- tiers of human knowledge. So relax, enjoy, and be sure to ask that question that you always wanted to have answered. Jasper Rine, Professor of Genetics and Developmental Biology Chair, Miller Institute 60th 60th Anniversary Agenda Friday, January 15 – Sunday, January 17, 2016 Friday evening - Alumni House 5:00 - 7:00 Reception Saturday – Stanley Hall 8:00 - 8:45 Registration 8:45 - 9:00 Welcome 9:00 - 11:45 Maha Mahadevan: “On growth and form: geometry, physics and biology” Alice Guionnet: “About Universal Laws” Roger Bilham: “Earthquakes and Money: Frail Buildings, Philanthropic Engineers and a Few Corrupt Bad Guys -

Annual Rpt 2004 For
I N S T I T U T E for A D V A N C E D S T U D Y ________________________ R E P O R T F O R T H E A C A D E M I C Y E A R 2 0 0 3 – 2 0 0 4 EINSTEIN DRIVE PRINCETON · NEW JERSEY · 08540-0631 609-734-8000 609-924-8399 (Fax) www.ias.edu Extract from the letter addressed by the Institute’s Founders, Louis Bamberger and Mrs. Felix Fuld, to the Board of Trustees, dated June 4, 1930. Newark, New Jersey. It is fundamental in our purpose, and our express desire, that in the appointments to the staff and faculty, as well as in the admission of workers and students, no account shall be taken, directly or indirectly, of race, religion, or sex. We feel strongly that the spirit characteristic of America at its noblest, above all the pursuit of higher learning, cannot admit of any conditions as to personnel other than those designed to promote the objects for which this institution is established, and particularly with no regard whatever to accidents of race, creed, or sex. TABLE OF CONTENTS 4·BACKGROUND AND PURPOSE 7·FOUNDERS, TRUSTEES AND OFFICERS OF THE BOARD AND OF THE CORPORATION 10 · ADMINISTRATION 12 · PRESENT AND PAST DIRECTORS AND FACULTY 15 · REPORT OF THE CHAIRMAN 20 · REPORT OF THE DIRECTOR 24 · OFFICE OF THE DIRECTOR - RECORD OF EVENTS 31 · ACKNOWLEDGMENTS 43 · REPORT OF THE SCHOOL OF HISTORICAL STUDIES 61 · REPORT OF THE SCHOOL OF MATHEMATICS 81 · REPORT OF THE SCHOOL OF NATURAL SCIENCES 107 · REPORT OF THE SCHOOL OF SOCIAL SCIENCE 119 · REPORT OF THE SPECIAL PROGRAMS 139 · REPORT OF THE INSTITUTE LIBRARIES 143 · INDEPENDENT AUDITORS’ REPORT 3 INSTITUTE FOR ADVANCED STUDY BACKGROUND AND PURPOSE The Institute for Advanced Study was founded in 1930 with a major gift from New Jer- sey businessman and philanthropist Louis Bamberger and his sister, Mrs. -

Report and Recommendations of the Panel to Assess the Nih Investment in Research on Gene Therapy
REPORT AND RECOMMENDATIONS OF THE PANEL TO ASSESS THE NIH INVESTMENT IN RESEARCH ON GENE THERAPY Stuart H. Orkin, M.D. Arno G. Motulsky, M.D. Co-chairs December 7, 1995 Executive Summary of Findings and Recommendations Dr. Harold Varmus, Director, National Institutes of Health (NIH), appointed an ad hoc committee to assess the current status and promise of gene therapy and provide recommendations regarding future NIH-sponsored research in this area. The Panel was asked specifically to comment on how funds and efforts should be distributed among various research areas and what funding mechanisms would be most effective in meeting research goals. The Panel finds that: 1. Somatic gene therapy is a logical and natural progression in the application of fundamental biomedical science to medicine and offers extraordinary potential, in the long-term, for the management and correction of human disease, including inherited and acquired disorders, cancer, and AIDS. The concept that gene transfer might be used to treat disease is founded on the remarkable advances of the past two decades in recombinant DNA technology. The types of diseases under consideration for gene therapy are diverse; hence, many different treatment strategies are being investigated, each with its own set of scientific and clinical challenges. 2. While the expectations and the promise of gene therapy are great, clinical efficacy has not been definitively demonstrated at this time in any gene therapy protocol, despite anecdotal claims of successful therapy and the initiation of more than 100 Recombinant DNA Advisory Committee (RAC)-approved protocols. 3. Significant problems remain in all basic aspects of gene therapy. -

The I Nstitute L E T T E R
THE I NSTITUTE L E T T E R INSTITUTE FOR ADVANCED STUDY PRINCETON, NEW JERSEY · FALL 2004 ARNOLD LEVINE APPOINTED FACULTY MEMBER IN THE SCHOOL OF NATURAL SCIENCES he Institute for Advanced Study has announced the appointment of Arnold J. Professor in the Life Sciences until 1998. TLevine as professor of molecular biology in the School of Natural Sciences. Profes- He was on the faculty of the Biochemistry sor Levine was formerly a visiting professor in the School of Natural Sciences where he Department at Princeton University from established the Center for Systems Biology (see page 4). “We are delighted to welcome 1968 to 1979, when he became chair and to the Faculty of the Institute a scientist who has made such notable contributions to professor in the Department of Microbi- both basic and applied biological research. Under Professor Levine’s leadership, the ology at the State University of New York Center for Systems Biology will continue working in close collaboration with the Can- at Stony Brook, School of Medicine. cer Institute of New Jersey, Robert Wood Johnson Medical School, Lewis-Sigler Center The recipient of many honors, among for Integrative Genomics at Princeton University, and BioMaPS Institute at Rutgers, his most recent are: the Medal for Out- The State University of New Jersey, as well as such industrial partners as IBM, Siemens standing Contributions to Biomedical Corporate Research, Inc., Bristol-Myers Squibb, and Merck & Co.,” commented Peter Research from Memorial Sloan-Kettering Goddard, Director of the Institute. Cancer Center (2000); the Keio Medical Arnold J. Levine’s research has centered on the causes of cancer in humans and ani- Science Prize of the Keio University mals. -

Aarhus University Honorary Doctorate Seminar Friday 13 September 2019 at 10.00 – 11.15
Department of Biomedicine Center for Genomics Personalized Medicine and Personalized Medicine Aarhus University Honorary Doctorate Seminar Friday 13 September 2019 at 10.00 – 11.15 Professor Mark Daly, Institute for Molecular Medicine Finland. Analytic and Translational Genetics Unit, USA. Broad Institute of Harvard and MIT, USA. Talk: Global partnerships: From Psychiatric Genetics to FinnGen and opportunities in discovery, prevention and personalized medicine. Venue: Eduard Biermann Auditory, The Lakeside Theatres, Aarhus University, Bartholins Allé 3, 8000 Aarhus C. Programme 10.00 – 10.05 Welcome by Anders Børglum 10.05 – 10.50 AU Honorary Doctorate lecture by Mark Daly 10.50 – 11.15 Open discussion Biosketch: Mark Daly, PhD, was appointed Director of the Institute for Molecular Medicine Finland (FIMM) in February 2018. He retains also his affiliations in Boston at the Harvard Medical School, Massachusetts General Hospital and as an institute member of the Broad Institute and co-director of the Program in Medical and Population Genetics. Daly received his B.S. in physics from the Massachusetts Institute of Technology and his Ph.D. in human genetics from Leiden University, Netherlands. He received the Curt Stern Award from the American Society of Human Genetics in 2014 and is a member of the National Academy of Medicine. Department of Biomedicine Center for Genomics Personalized Medicine and Personalized Medicine His research primarily focuses on the development and application of statistical methods for the discovery and interpretation of genetic variation responsible for complex human disease. In addition to foundational work in human genetics methodology, his lab has made major contributions to gene discovery in inflammatory bowel disease, autism and schizophrenia - primarily through catalyzing global collaborative research efforts which he continues to help lead.