Phenobarbitonetab.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phenobarbital Brand Name: Phenobarb
Generic Name: Phenobarbital Brand Name: Phenobarb What Is It Used For? Decreasing seizure activity in various types of seizures. Especially useful for controlling seizures in neonates and infants Given intravenously in the emergency department for status epilepticus. How Long Does The Oral Medicine Take to Work? 10-30 days What Are The Important Safety Concerns? When first starting the medicine, your child may be slightly drowsy and/or dizzy. Only adjust the dosage as recommended by your health care provider. They will usually increase this medication slowly to avoid side effects. Never increase the dosage more than once per week unless directed otherwise. Once you have started with one brand of the medication stay with it. Avoid switching between different brands. Check with your pharmacist before taking herbal medications and/or over-the- counter medications. They may have adverse effects if taken with anti-seizure medications. Do not stop taking this medication suddenly because this could result in seizures. It is important to keep a record of your child’s seizures and side effects to determine how well they are responding to the medication. Does My Child Need Bloodwork With This Medication? Routine blood work may be done to help determine the best dosage for your child, and also if they have side effects to the medication. If your child is required to have blood work it must be done BEFORE they get the medication. This is called a trough level. This level usually falls between 65 and 170. A blood test may be done before starting this medication to check your child’s liver function and blood counts. -

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -
CDHO Factsheet Epilepsy
Disease/Medical Condition EPILEPSY Date of Publication: August 7, 2014 (also known as “seizure disorder”) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No Is medical consult advised? ...................................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled) Is the initiation of invasive dental hygiene procedures contra-indicated?** No Is medical consult advised? ....................................... Possibly (e.g., if there is medication non-compliance) Is medical clearance required? .................................. Possibly (e.g., if there is significant risk of seizure; patient/ client should be seizure-free for several months to be considered controlled) Is antibiotic prophylaxis required? .............................. No Is postponing treatment advised? ............................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled and for which there are no anticipated exacerbating factors in the office setting) Oral management implications Important considerations in the management of epileptic patients/clients are prevention of seizures in the dental chair and preparation for managing seizures if they occur. When a patient/client responds positively to questions about seizures/ epilepsy during health history taking, further information should be obtained. Based on the patient/client’s responses, the dental hygienist may choose to postpone treatment to avoid triggering a seizure in the dental chair. It is valuable for the dental hygienist to know what factors have the potential to exacerbate epileptic seizures in a particular patient/client in order that trigger stimuli can be avoided. The dental hygienist can reduce stress and anxiety by explaining procedures before starting. Bright light should be kept out of the patient/client’s eyes, and dark glasses may assist with this. -

Pentobarbital Sodium
PENTobarbital Sodium Brand names Nembutal Sodium Medication error Look-alike, sound-alike drug names. Tall man letters (not FDA approved) are recommended potential to decrease confusion between PENTobarbital and PHENobarbital.(1,2) ISMP recommends the following tall man letters (not FDA approved): PENTobarbital.(30) Contraindications Contraindications: In patients with known hypersensitivity to barbiturates or any com- and warnings ponent of the formulation.(2) If an allergic or hypersensitivity reaction or a life-threatening adverse event occurs, rapid substitution of an alternative agent may be necessary. If pentobarbital is discontinued due to development of a rash, an anticonvulsant that is structurally dissimilar should be used (i.e., nonaromatic). (See Rare Adverse Effects in the Comments section.) Also contraindicated in patients with a history of manifest or latent porphyria.(2) Warnings: Rapid administration may cause respiratory depression, apnea, laryngospasm, or vasodilation with hypotension.(2) Should be withdrawn gradually if large doses have been used for prolonged periods.(2) Paradoxical excitement may occur or important symptoms could be masked when given to patients with acute or chronic pain.(2) May be habit forming. Infusion-related Respiratory depression and arrest requiring mechanical ventilation may occur. Monitor cautions oxygen saturation. If hypotension occurs, the infusion rate should be decreased and/or the patient should be treated with IV fluids and/or vasopressors. Pentobarbital is an alkaline solution (pH = 9–10.5); therefore, extravasation may cause tissue necrosis.(2) (See Appendix E for management.) Gangrene may occur following inadvertent intra-arterial injection.(2) Dosage Medically induced coma (for persistently elevated intracranial pressure (ICP) or refractory status epilepticus): Patient should be intubated and mechanically ventilated. -

Chapter 25 Mechanisms of Action of Antiepileptic Drugs
Chapter 25 Mechanisms of action of antiepileptic drugs GRAEME J. SILLS Department of Molecular and Clinical Pharmacology, University of Liverpool _________________________________________________________________________ Introduction The serendipitous discovery of the anticonvulsant properties of phenobarbital in 1912 marked the foundation of the modern pharmacotherapy of epilepsy. The subsequent 70 years saw the introduction of phenytoin, ethosuximide, carbamazepine, sodium valproate and a range of benzodiazepines. Collectively, these compounds have come to be regarded as the ‘established’ antiepileptic drugs (AEDs). A concerted period of development of drugs for epilepsy throughout the 1980s and 1990s has resulted (to date) in 16 new agents being licensed as add-on treatment for difficult-to-control adult and/or paediatric epilepsy, with some becoming available as monotherapy for newly diagnosed patients. Together, these have become known as the ‘modern’ AEDs. Throughout this period of unprecedented drug development, there have also been considerable advances in our understanding of how antiepileptic agents exert their effects at the cellular level. AEDs are neither preventive nor curative and are employed solely as a means of controlling symptoms (i.e. suppression of seizures). Recurrent seizure activity is the manifestation of an intermittent and excessive hyperexcitability of the nervous system and, while the pharmacological minutiae of currently marketed AEDs remain to be completely unravelled, these agents essentially redress the balance between neuronal excitation and inhibition. Three major classes of mechanism are recognised: modulation of voltage-gated ion channels; enhancement of gamma-aminobutyric acid (GABA)-mediated inhibitory neurotransmission; and attenuation of glutamate-mediated excitatory neurotransmission. The principal pharmacological targets of currently available AEDs are highlighted in Table 1 and discussed further below. -

1,1,1-Trichloroethane (CASRN 71-55-6) | IRIS
Integrated Risk Information System (IRIS) U.S. Environmental Protection Agency Chemical Assessment Summary National Center for Environmental Assessment 1,1,1-Trichloroethane; CASRN 71-55-6 Human health assessment information on a chemical substance is included in the IRIS database only after a comprehensive review of toxicity data, as outlined in the IRIS assessment development process. Sections I (Health Hazard Assessments for Noncarcinogenic Effects) and II (Carcinogenicity Assessment for Lifetime Exposure) present the conclusions that were reached during the assessment development process. Supporting information and explanations of the methods used to derive the values given in IRIS are provided in the guidance documents located on the IRIS website. STATUS OF DATA FOR 1,1,1-Trichloroethane File First On-Line 03/31/1987 Category (section) Assessment Available? Last Revised Oral RfD (I.A.) Acute Oral RfD (I.A.1.) qualitative discussion 09/28/2007 Short-term Oral RfD (I.A.2.) qualitative discussion 09/28/2007 Subchronic Oral RfD (I.A.3.) yes 09/28/2007 Chronic Oral RfD (I.A.4.) yes 09/28/2007 Inhalation RfC (I.B.) Acute Inhalation RfC (I.B.1.) yes 09/28/2007 Short-term Inhalation RfC (I.B.2.) yes 09/28/2007 Subchronic Inhalation RfC (I.B.3.) yes 09/28/2007 1 Integrated Risk Information System (IRIS) U.S. Environmental Protection Agency Chemical Assessment Summary National Center for Environmental Assessment Category (section) Assessment Available? Last Revised Chronic Inhalation RfC (I.B.4.) yes 09/28/2007 Carcinogenicity Assessment (II.) yes 09/28/2007 I. Health Hazard Assessments for Noncarcinogenic Effects I.A. -

Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva
REVIEW ARTICLE Therapeutic Drug Monitoring of Antiepileptic Drugs by Use of Saliva Philip N. Patsalos, FRCPath, PhD*† and Dave J. Berry, FRCPath, PhD† INTRODUCTION Abstract: Blood (serum/plasma) antiepileptic drug (AED) therapeu- Measuring antiepileptic drugs (AEDs) in serum or tic drug monitoring (TDM) has proven to be an invaluable surrogate plasma as an aid to personalizing drug therapy is now a well- marker for individualizing and optimizing the drug management of established practice in the treatment of epilepsy, and guidelines patients with epilepsy. Since 1989, there has been an exponential are published that indicate the particular features of epilepsy and increase in AEDs with 23 currently licensed for clinical use, and the properties of AEDs that make the practice so beneficial.1 recently, there has been renewed and extensive interest in the use of The goal of AED therapeutic drug monitoring (TDM) is to saliva as an alternative matrix for AED TDM. The advantages of saliva ’ fl optimize a patient s clinical outcome by supporting the man- include the fact that for many AEDs it re ects the free (pharmacolog- agement of their medication regimen with the assistance of ically active) concentration in serum; it is readily sampled, can be measured drug concentrations/levels. The reason why TDM sampled repetitively, and sampling is noninvasive; does not require the has emerged as an important adjunct to treatment with the expertise of a phlebotomist; and is preferred by many patients, AEDs arises from the fact that for an individual patient -

DOCUMENT RESUME ED 300 697 CG 021 192 AUTHOR Gougelet, Robert M.; Nelson, E. Don TITLE Alcohol and Other Chemicals. Adolescent A
DOCUMENT RESUME ED 300 697 CG 021 192 AUTHOR Gougelet, Robert M.; Nelson, E. Don TITLE Alcohol and Other Chemicals. Adolescent Alcoholism: Recognizing, Intervening, and Treating Series No. 6. INSTITUTION Ohio State Univ., Columbus. Dept. of Family Medicine. SPONS AGENCY Health Resources and Services Administration (DHHS/PHS), Rockville, MD. Bureau of Health Professions. PUB DATE 87 CONTRACT 240-83-0094 NOTE 30p.; For other guides in this series, see CG 021 187-193. AVAILABLE FROMDepartment of Family Medicine, The Ohio State University, Columbus, OH 43210 ($5.00 each, set of seven, $25.00; audiocassette of series, $15.00; set of four videotapes keyed to guides, $165.00 half-inch tape, $225.00 three-quarter inch tape; all orders prepaid). PUB TYPE Guides - Classroom Use - Materials (For Learner) (051) -- Reports - General (140) EDRS PRICE MF01 Plus Plstage. PC Not Available from EDRS. DESCRIPTORS *Adolescents; *Alcoholism; *Clinical Diagnosis; *Drug Use; *Family Problems; Physician Patient Relationship; *Physicians; Substance Abuse; Units of Study ABSTRACT This document is one of seven publications contained in a series of materials for physicians on recognizing, intervening with, and treating adolescent alcoholism. The materials in this unit of study are designed to help the physician know the different classes of drugs, recognize common presenting symptoms of drug overdose, and place use and abuse in context. To do this, drug characteristics and pathophysiological and psychological effects of drugs are examined as they relate to administration, -

5 Clinical Pearls for Contraception and Preconception Counseling
EDITORIAL Women with epilepsy: 5 clinical pearls for contraception and preconception counseling For women with epilepsy, intrauterine devices are the optimal reversible contraceptive, and, preconception, the use of antiepileptic drugs with the lowest teratogenic potential should be considered Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital, Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School, Boston n 2015, 1.2% of the US population bazepine (Aptiom), felbamate (Fel- becoming pregnant while taking the was estimated to have active epi- batol), oxcarbazepine (Trileptal), oral contraceptive.6 Carbamazepine, Ilepsy.1 For neurologists, key goals perampanel (Fycompa), phenobarbi- a strong inducer of hepatic enzymes, in the treatment of epilepsy include: tal, phenytoin (Dilantin), primidone was the most frequently used AED in controlling seizures, minimizing (Mysoline), rufinamide (Banzel), this sample. adverse effects of antiepileptic drugs and topiramate (Topamax) (at dos- Many studies report that carba- (AEDs) and optimizing quality of ages >200 mg daily). According to mazepine accelerates the metabo- life. For obstetrician-gynecologists, Lexicomp, the following AEDs do not lisms of estrogen and progestins and women with epilepsy (WWE) have cause clinically significant changes reduces contraceptive efficacy. For unique contraceptive, preconcep- in hepatic enzymes that metabolize example, in one study 20 healthy tion, and obstetric needs that require steroid hormones: acetazolamide women were administered an ethi- highly specialized approaches to (Diamox), clonazepam (Klonopin), nyl estradiol (20 µg)-levonorgestrel care. Here, I highlight 5 care points ethosuximide (Zarontin), gabapentin (100 µg) contraceptive, and randomly that are important to keep in mind (Neurontin), lacosamide (Vimpat), assigned to either receive carbamaze- when counseling WWE. -
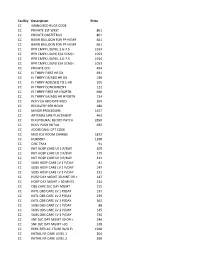
NMMC West Point CDM.Xlsx
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine