Emergency Airway Management in the Trauma Patient (Full Guideline)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Program 0700
PROGRAM 0700 – 1700 Registration Desk Open 0730 - 0800 Arrival Coffee & Tea 0800 – 0810 Welcome and Acknowledgement to Country Dr Sandy Zalstein, Head of Trauma Services, Royal Hobart Hospital Clinical Associate Professor Marcus Skinner, Clinical Director, Surgical and Perioperative Services, Royal Hobart Hospital 0810 – 0820 Official Symposium Opening Address The Hon. Michael Ferguson MP Minister for Health, TAS Session One: State of Readiness Chair: Dr Sandy Zalstein, Head of Trauma Services, Royal Hobart Hospital 0820 – 0920 Opening Keynote Address Thoughts on the unthinkable Dr Greg Robertson Chief of Surgery, Canterbury District Health Board General and Colorectal Surgeon 0920 – 1000 Working Together to Prepare and Respond. Are we ready? Dr Paul Barnes Head of Risk and Resilience Program, Australian Strategic Policy Institute 1000– 1030 Morning Refreshment Break + Trade Exhibition Session Two: Lessons Learned Chair: Clinical Associate Professor Marcus Skinner, Clinical Director, Surgical and Perioperative Services, Royal Hobart Hospital 1030 – 1110 2004 Boxing Day Tsunami: Australia’s response to Banda Aceh GPCAPT Assoc Prof David M Scott Immediate Past President, Australian Society of Anaesthetists Group Captain, Royal Australian Air Force 1110 – 1150 2009 Black Saturday Bushfires: Hospital, state and national responses to the worst bushfire in Australian history Miss Heather Cleland Visiting Plastic Surgeon and Head of the Victorian Adult Burns Unit, Alfred Hospital Associate Professor, Dept of Surgery, Central Clinical School, -

Importance of Validation Risk Prediction Tools
Art: toc Input-citi 22:40 12/2/7 12؍balt6/z7i-anesth/z7i-anesth/z7i00812/contents panickes S ON THE COVER: David Mackey, M.D., has organized a fascinating series of commentaries by national leaders In this issue of ANESTHESIOLOGY, two original research articles and three editorial views examine in the construction and use of clinical data registries by regulatory agencies and physician the use of data in clinical decision making. practices, the first two of which appear in this month’s issue: ● Kheterpal et al.: Impact of a Novel Multiparameter Decision Support System on Intraoperative ● Mackey: Can We Finally Conquer the Problem of Medical Quality? The Systems-based Processes of Care and Postoperative Outcomes, p. 272 Opportunities of Data Registries and Medical Teamwork, p. 225 ● Liu et al.: Defining the Intrinsic Cardiac Risks of Operations to Improve Preoperative Cardiac ● Jain et al.: A Public-Private Strategy to Advance the Use of Clinical Registries, p. 227 Risk Assessments, p. 283 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/128/2/A1/364553/20180200_0-00001.pdf by guest on 01 October 2021 ● Sessler: Decision Support Alerts: Importance of Validation, p. 241 ● Glance et al.: Risk Prediction Tools: The Need for Greater Transparency, p. 244 ● Javitt: Regulatory Landscape for Clinical Decision Support Technology, p. 247 ᭛ THIS MONTH IN ANESTHESIOLOGY 9A ᭛◆ THISEDITORIAL MONTH VIEWS IN ANESTHESIOLOGY 1A . Can We Finally Conquer the Problem of Medical Quality? The Systems-based ◼ SCIENCE, MEDICINE, AND THE ANESTHESIOLOGIST 15A Opportunities of Data Registries and Medical Teamwork 225 David C. Mackey ◼ INFOGRAPHICS IN ANESTHESIOLOGY 19A . A Public-Private Strategy to Advance the Use of Clinical Registries 227 Sachin H. -
RN to EMT-Basic Transition Course
State of Wisconsin Registered Nurse to EMT-Basic Transition Course November 2010 Wisconsin EMS Section State of Wisconsin RN to EMT-Basic Transition Course TABLE OF CONTENTS Introduction .....................................................................................................iv List of Appendices...........................................................................................vi Module 1 – Preparatory 1-1 Introduction to Emergency Care .................................................. 1-1 1-2 Well-Being of the EMT Basic ....................................................... 1-6 1-3 Medical/Legal and Ethical Issues............................................... 1-12 1-5 Lifting and Moving Patients........................................................ 1-16 1-6 Evaluation .................................................................................. 1-25 Module 2 - Patient Assessment 2-1 Scene Size-up ............................................................................. 2-1 2-2 Initial Assessment........................................................................ 2-6 2-3 Baseline Vital Signs, SAMPLE History and the Use of Pulse Oximetry .......................................................................... 2-11 2-4 Focused History and Physical Exam: Trauma ........................... 2-16 2-5 Focused History and Physical Exam: Medical ........................... 2-22 2-6 Detailed Physical Exam ............................................................. 2-27 2-7 On-Going Assessment.............................................................. -

Responses to Questions on Notice – Inquiry Into the Work Health and Safety Bill 2019
17 July 2020 Hon Dr Sally Talbot MLC Chair, Standing Committee on Legislation Legislative Council Committee Office Parliament House 4 Harvest Terrace WEST PERTH WA 6005 Dear Dr Talbot Responses to Questions on Notice – Inquiry into the Work Health and Safety Bill 2019 The Master Builders Association Western Australia (Master Builders) thanks the Standing Committee on Legislation for the opportunity to appear at its hearing into the Inquiry into the Work Health and Safety Bill 2019 on Thursday 9 July 2020. Please find enclosed Master Builders’ responses to the relevant Questions on Notice arising from that hearing, and Supplementary Information. Should you have any queries or wish to discuss this response, please contact me. Yours sincerely Cathryn Greville Acting Executive Director Encl. Responses to Questions on Notice and Supplementary Information Attachment 1 – Coroner’s Report: Jorge Alberto Castillo-Riffo Attachment 2 – Breaches by Officials Attachment 3 – Joint Industry Group letter to the Premier Responses to Questions on Notice Question on Notice 2 – Coroner’s Report Provision of South Australian coroner’s report where the coroner commented on what would have happened if industrial manslaughter was in place – in particular with respect to defensive strategies and blame culture. 1. The relevant Coroners report is that of South Australian State Coroner Mark Frederick Johns, Inquest into death of Jorge Alberto Castillo-Riffo (2014), delivered 1 November 2018, Inquest Number 9/2018 (2071/2014).1 A copy is attached to this response at Attachment 1. 2. The extract referenced during the hearing appears at paragraphs 36.1 and 36.2 of that report, where the question of the value of criminal prosecution for fatal industrial accidents is raised. -
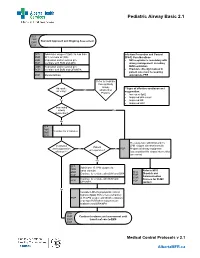
Pediatric Airway Basic 2.1
Pediatric Airway Basic 2.1 SFA FMR Standard Approach and Ongoing Assessment EMR PCP SFA Administer oxygen if SpO2 Is less than Infection Prevention and Control FMR 94% on room air (RA) (IP&C) Considerations EMR Reposition and/or suction prn • N95 respirator is mandatory with PCP Ventilate with BVM and OPA airway management, including EMR Reposition and/or suction prn BVM ventilation PCP Ventilate with BVM and OPA/NPA • Providers directly involved in patient care must be wearing PCP Monitor EtCO2 appropriate PPE Refer to Pediatric Foreign Body Airway Adequate **Signs of effective ventilation and No Obstruction air entry? oxygenation: Protocol • Increased Sp02 • Improved skin colour Yes • Improved HR • Improved LOC Impending airway Yes obstruction? No SFA FMR Ventilate for 2 minutes EMR PCP Pre-oxygenate with NRB and 15 Ventilation LPM oxygen via nasal cannula Patient and oxygenation No No PCP Prepare all airway equipment unresponsive? effective?** Assess patient for airway intervention (see notes) Yes SFA Administer 15 LPM oxygen via FMR nasal cannula Refer to MFR EMR SFA Continue to ventilate with BVM and OPA Dispatch and PCP FMR Communication EMR Continue to ventilate with BVM and Process for OLMC PCP PCP OPA/NPA contact Yes Consider LMA if symptomatic critical hypoxia (SpO2 85% or less) refractory PCP to 15 LPM oxygen with BVM ventilation (2-person BVM when resources are available) and OPA/NPA SFA FMR Continue treatment and assessment until EMR transfer of care to EMS PCP Medical Control Protocols v 2.1 AlbertaMFR.ca Pediatric Airway Basic 2.1 Definition Basic airway management is known to improve patient survival rates in the prehospital field. -

St Mark's News
St Mark’s NEWSISSUE MARCH 2015 THE UNIVERSITIES OF ADELAIDE, PENNINGTON TERRACE NORTH ADELAIDE East Wing Opening Completing the Vision Academic and Sporting Success The College Library in the 1990s In this Issue From the Master .............................................................................................................. 3 The East Wing Project ..................................................................................................... 4 Scholarships and Academic Results ............................................................................... 6 Hawker Scholarship ......................................................................................................... 7 Cowan Grants .................................................................................................................. 7 College Club Committee ................................................................................................. 8 Students Dhow a Committment to Social Justice .......................................................... 9 About St Mark’s Sporting Success ........................................................................................................... 10 Around the College ........................................................................................................ 12 College Paralympic Hopeful Gives Back to Charity .................................................................... 14 Founded in 1925 as the first Honorary Degrees ......................................................................................................... -

Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444
Airway: 2 Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444 UNIT TERMINAL OBJECTIVE 2-1 At the completion of this unit, the EMT-Intermediate student will be able to establish and/ or maintain a patent airway, oxygenate, and ventilate a patient. COGNITIVE OBJECTIVES At the completion of this unit, the EMT-Intermediate student will be able to: 2-1.1 Explain the primary objective of airway maintenance. (C-1) 2-1.2 Identify commonly neglected prehospital skills related to airway. (C-1) 2-1.3 Identify the anatomy and functions of the upper airway. (C-1) 2-1.4 Describe the anatomy and functions of the lower airway. (C-1) 2-1.5 Explain the differences between adult and pediatric airway anatomy. (C-1) 2-1.6 Define normal tidal volumes for the adult, child, and infant. (C-1) 2-1.7 Define atelectasis. (C-1) 2-1.8 Define FiO2. (C-1) 2-1.9 Explain the relationship between pulmonary circulation and respiration. (C-3) 2-1.10 List factors which cause decreased oxygen concentrations in the blood. (C-1) 2-1.11 List the factors which increase and decrease carbon dioxide production in the body. (C 2-1.12 Describe the measurement of oxygen in the blood. (C-1) 2-1.13 Describe the measurement of carbon dioxide in the blood. (C-1) 2-1.14 List the concentration of gases which comprise atmospheric air. (C-1) 2-1.15 List the factors which affect respiratory rate and depth. (C-1) 2-1.16 Describe the voluntary and involuntary regulation of respiration. -

An Anesthesiologist's Perspective on the History of Basic Airway Management
Anesthesiology ALN SPECIAL ARTICLE ANET anet ABSTRACT aln This fourth and last installment of my history of basic airway management dis- cusses the current (i.e., “modern”) era of anesthesia and resuscitation, from 1960 to the present. These years were notable for the implementation of inter- ALN An Anesthesiologist’s mittent positive pressure ventilation inside and outside the operating room. Basic airway management in cardiopulmonary resuscitation (i.e., expired air Perspective on the ventilation) was de-emphasized, as the “A-B-C” (airway-breathing-circula- ALN tion) protocol was replaced with the “C-A-B” (circulation-airway-breathing) History of Basic Airway intervention sequence. Basic airway management in the operating room 0003-3022 (i.e., face-mask ventilation) lost its predominant position to advanced airway Management management, as balanced anesthesia replaced inhalation anesthesia. The one-hand, generic face-mask ventilation technique was inherited from the 1528-1175 The “Modern” Era, 1960 to Present progressive era. In the new context of providing intermittent positive pres- sure ventilation, the generic technique generated an underpowered grip with Lippincott Williams & WilkinsHagerstown, MD Adrian A. Matioc, M.D. a less effective seal and an unspecified airway maneuver. The significant advancement that had been made in understanding the pathophysiology of ANESTHESIOLOGY 2019; 130:00–00 upper airway obstruction was thus poorly translated into practice. In contrast 10.1097/ALN.0000000000002646 to consistent progress in advanced airway management, progress in basic airway techniques and devices stagnated. “Anesthetists who have not tried this two-handed ANESTHESIOLOGY 2019; 130:00–00 hyperextension manipulation will be surprised to observe the combined effects of simultaneously Special Article pushing the vertex of the head backward and pulling The generic one-hand face-mask ventilation inher- upward on the symphysis of the mandible.” ited from the progressive era (i.e., the “E-C” technique) 2019 Editorial. -

Basic Airway Management & Decision Making
Roberts: Clinical Procedures in Emergency Medicine, 5th ed. CHAPTER 3 – Basic Airway Management and Decision-Making Robert F. Reardon, Phillip E. Mason, Joseph E. Clinton Over the last few decades, several important changes have occurred in emergency airway management. Bag-mask ventilation has been supplemented by intermediate, or backup, ventilation devices like the laryngeal mask airway (LMA), the Combitube, and the laryngeal tube. These have become important devices for the initial resuscitation of apneic patients and for rescue ventilation when intubation fails.[1] Noninvasive positive-pressure ventilation (NPPV) is now used in place of tracheal intubation in some critically ill patients. Despite these advances, basic techniques such as opening the airway, oxygenation, and bag-mask ventilation remain the cornerstones of good emergency airway management. [2] [3] Airway maintenance without endotracheal intubation is one of the most important emergency [4] airway management techniques to keep patients alive until a definitive airway can be established. This chapter describes basic airway skills including opening the airway, O2 therapy, NPPV, bag-mask ventilation, and intermediate ventilation devices. Because of the complexity of these skills and decisions, providers should develop a simple, organized approach to emergency airway management, being cognizant that when a specific intervention has failed, it is time to move rapidly to a different approach. Developing a simple preconceived algorithm that employs proven techniques and is applicable to a broad range of clinical scenarios will help providers manage difficult, anxiety-provoking emergency airways. THE CHALLENGE OF EMERGENCY AIRWAY MANAGEMENT Although other specialists are sometimes available, most emergency airways are managed by emergency clinicians.[5] Airway management in the emergency department (ED) is much different from airway management in the controlled setting of the operating room. -

Education Update 65 | April 6 / 2011
SAASSO Education Bulletin 02 | June 24 / 2009 SAASSO Education Update 65 | April 6 / 2011 Education System Flawed Vandalism: Schools Count The Cost University Backs Medicine Exam Social media link puts parents in the picture Australian Chamber of Commerce and Industry Vandalism costs South Australian schools over The University of Adelaide will continue to test year A senior lecturer at Flinders University proposes chief executive Peter Anderson says that $6 million each year. 12 students with the Undergraduate Medicine and schools use social media in the classroom to unite Australia's education system is structurally flawed Health Sciences Admission Test (UMAT). parents and the school community in a bid to in the fields of literacy and numeracy. Figures obtained under Freedom of Information by educate young people about its use. MLC Rob Brokenshire show the average spend per The exam is under scrutiny after a study published The Industry Skills Councils report, „No More school on vandalism was $11,100 in 2010. in the Medical Journal of Australia found only a A recent study by Dr. Rahamathulla found parents' Excuses‟, finds that almost half of Australia's "weak correlation" between a student‟s UMAT involvement in their children's online activities was working age population do not have the literacy or "The (Education) Department needs to do much score and grade point average at university. "disturbingly" low. The TeenSpeak survey of 500 numeracy skills required to study a trade. more than a budget line of millions of dollars to fix South Australian teenagers from 13 to 17 found; vandalism," Mr Brokenshire says. -

Airway Management
AIRWAY MANAGEMENT Angkana Lurngnateetape, MD. Department of Anesthesiology Siriraj Hospital Perhaps the most important responsibility of the anesthesiologist is “management of the patient’s airway” Miller RD’s Anesthesia 2000 Barash PG, Cullen BF, Stoelting RK’s Clinical Anesthesia 2001 What should we know about “airway management”? ● Airway anatomy and function ● Evaluation of airway ● Clinical management of the airway - Maintenance and ventilation - Intubation and extubation - Difficult airway management Airway anatomy The term “airway” refers to the upper airway, consisting of ● Nasal and oral cavities ● Pharynx ● Larynx ● Trachea ● Principle bronchi Anatomy of upper airway Larynx in laryngoscopic view Nerves V1 V2 V3 IX Vagus nerve • Superior laryngeal n – External br (Motor) • cricothyroid m SL – Internal br (Sensory) • area above cord • Recurrent laryngeal n - Motor br • intrinsic m RL – Sensory br • area below cord Evaluation of the airway ● History ● Physical examination ● Special investigation Evaluation of the airway “History” ● Previous history of difficult airway ● Airway-related untoward events ● Airway-related symptoms/diseases Evaluation of the airway Physical examination ● Ease of open airway and maintenance ● Ease of tracheal intubation ● Teeth ● Neck movement ● Intubation hazards ● Signs of airway distress Evaluation of the airway Anatomic characteristics associated with difficult airway management ● Short muscular neck ● Receding mandible ● Protruding maxillary incisors ● Long high-arched palate ● Inability to visualize -

Tutor Guide – Pre-Oxygenation and Basic Airway Management Thank
Tutor Guide – Pre-oxygenation and Basic Airway Management Thank you very much for helping with the airway mastery learning program. Attached is the pre-course material which trainees should read and complete before attending. It includes a checklist and you should use this when assessing them. It also includes a pass mark, which should be regarded as formative rather than summative. Ideally the programme should be delivered as described here, but we recognise that not every department will be able to achieve this. • Teaching can take up to 60 minutes depending on the trainee. • There should ideally only be up to two trainees per tutor at a time. • Ideally the trainee should also have had an opportunity to practice with the equipment on the manikin prior to the session. • It is very important to create a safe space and non-threatening environment for the learner. Stages of the process are: 1. Trainee reads pre-course material and watches video before attending. 2. Participant performs procedure on the manikin as a formative assessment. 3. Tutor gives specific feedback about performance. 4. Trainee repeats procedure until you are happy they do it properly (this may need more than one session). Skills to assess as part of formative assessment (use checklist): 1. Conditions for airway management – demonstrate an understanding of equipment, monitoring, personnel and supervision needed for safe practice. 2. Demonstrates knowledge of pre-oxygenation goals. 3. Perform airway opening manoeuvres (including use of adjuncts). 4. Effective bag-valve-mask