American Red Cross Focused Updates and Guidelines 2020 Resuscitation Suite BLS, ALS, PALS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Commotio Cordis
Commotio Cordis Background Sudden unexpected cardiac death that occurs in young people during sports participation is usually associated with previously diagnosed or undiagnosed structural or primary electrical cardiac abnormalities. Examples of such abnormalities include hypertrophic cardiomyopathy, anomalous origin of a coronary artery, arrhythmogenic right ventricular cardiomyopathy, and primary electrical disorders, such as congenital prolongation of the QTc interval and catecholaminergic, polymorphic ventricular tachycardia (CPVT). Sudden death due to ventricular fibrillation may also occur following a blunt, nonpenetrating blow to the chest, specifically the precordial area, in an individual with no underlying cardiac disease. This is termed commotio cordis. Much of our understanding of the clinical and pathophysiologic aspects of commotio cordis is the result of work by N.A. Mark Estes III, MD, and Mark S. Link, MD, from the New England Cardiac Arrhythmia Center at the Tufts University and School of Medicine in Boston, Massachusetts and data derived from the US Commotio Cordis Registry (Minneapolis, Minnesota). Relatively recent data from the registry of the Minneapolis Heart Institute Foundation show that commotio cordis is one of the leading cause of sudden cardiac death in young athletes, exceeded only by hypertrophic cardiomyopathy and congenital cornoary artery abnormalities.[1] Commotio cordis typically involves young, predominantly male, athletes in whom a sudden, blunt, nonpenetrating and innocuous-appearing trauma to the anterior chest results in cardiac arrest and sudden death from ventricular fibrillation. The rate of successful resuscitation remains relatively low but is improving slowly. Although commotio cordis usually involves impact from a baseball, it has also been reported during hockey, softball, lacrosse, karate, and other sports activities in which a relatively hard and compact projectile or bodily contact caused impact to the person's precordium. -

Emergency Medical Services Program Policies – Procedures – Protocols
Emergency Medical Services Program Policies – Procedures – Protocols Protocols Table of Contents GENERAL PROVISIONS ................................................................................................ 3 DESTINATION DECISION SUMMARY-METRO BAKERSFIELD AREA ........................ 5 DETERMINATION OF DEATH ..................................................................................... 12 101 AIRWAY OBSTRUCTION ...................................................................................... 16 102 ALTERED LEVEL OF CONSCIOUSNESS ............................................................ 18 103 ALLERGIC REACTION/ANAPHYLAXIS ................................................................ 20 104 ASYSTOLE/ PULSELESS ELECTRICAL ACTIVITY ............................................. 22 105 BITES STINGS ENVENOMATION ......................................................................... 24 106 BRADYCARDIA ..................................................................................................... 26 107 BRIEF RESOLVED UNEXPLAINED EVENT ......................................................... 29 108 BURNS ................................................................................................................... 32 109 CHEMPACK ........................................................................................................... 35 110 CHEST PAIN OR ACUTE CORONARY SYNDROME ........................................... 37 111 CHEST TRAUMA .................................................................................................. -

Medical Memoranda MEDICAJHRNA Haemodynamic Effects of Balloon
27 January 1968 Medical Memoranda MEDICAJHRNA 225 he had been after the myocardial infarction in March 1967. There- He was readmitted on 6 September again in supraventricular after he was maintained on lignocaine infusion 1 mg./min. to a tachycardia and with evidence of congestive failure. On three maximum of 500 mg. in 24 hours and remained in sinus rhythm for occasions over the next 48 hours a precordial thump converted this Br Med J: first published as 10.1136/bmj.1.5586.225 on 27 January 1968. Downloaded from 48 hours with only occasional extrasystoles. By this time the rhythm to sinus rhythm. On each occasion the procedure was infusion had been discontinued and he felt well, was in sinus performed with the patient monitored on the cardioverter, and with rhythm 80/min., and the blood pressure was 120/70. the shock paddles prepared and an intravenous drip available for At this time he suddenly relapsed to the original dysrhythmia- giving sodium bicarbonate or other drugs in the event of more supraventricular tachycardia with right bundle-branch block. On serious arrhythmia developing. In view of the continuing cardiac this occasion, as an alternative to further electrical cardioversion irritability with multifocal extrasystoles he was then put on a but while being monitored on the " cardioverter," he was given a procainamide continuous infusion, 4 g. in 24 hours, which had the sharp blow on the sternum with no effect. A similar heavy thump effect of almost clearing the ventricular ectopic beats. with the ulnar side of the clenched fist on the precordium at the cardiac apex immediately induced sinus rhythm with left bundle- COMMENT branch block (see Fig.). -
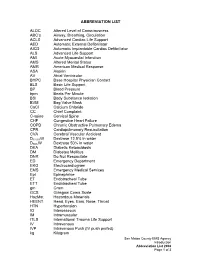
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Marvel-Phile: Über-Grim-And-Gritty EXTREME Edition!
10 MAR 2018 1 Marvel-Phile: Über-Grim-and-Gritty EXTREME Edition! It was the best of times, it was the worst of times. It 90s, but you’d be wrong. Then we have Nightwatch, a was a dark time for the Republic. In short, it was...the bald-faced ripoff of Todd MacFarlane’s more ‘90s. The 1990s were an odd time for comic books. A successful Spawn. Next, we have Necromancer… the group of comic book artists, including the likes of Jim Dr. Strange of Counter-Earth. And best for last, Lee and hate-favorite Rob Liefield, splintered off from there’s Adam X the X-TREME! Oh dear Lord -- is there Marvel Comics to start their own little company called anything more 90s than this guy? With his backwards Image. True to its name, Image Comics featured comic baseball cap, combustible blood, a costume seemingly books light on story, heavy on big, flashy art (often made of blades, and a title that features not one but either badly drawn or heavily stylized, depending on TWO “X”s, this guy that was teased as the (thankfully who you ask), and a grim and gritty aesthetic that retconned) “third Summers brother” is literally seemed to take all the wrong lessons from renowned everything about the 90s in comics, all rolled into one. works such as Frank Miller’s Dark Knight Returns. Don’t get me wrong, there were a few gems in the It wasn’t long until the Big Two and other publishers 1990s. Some of my favorite indie books were made hopped on the bandwagon, which was fueled by during that time. -

Precordial Thump
practical procedures resuscitation skills – part five Precordial thump phil Jevon, pGce, Bsc, rN, is tachycardia, asystole and resuscitation officer/clinical skills complete heart block where a lead, Manor Hospital, Walsall. precordial thump was delivered. The results were as follows: The precordial thump is a blow to l Ninety-one (49%) reverted to the lower half of the patient’s normal sinus rhythm; sternum using the lateral aspect l Seventy-seven (41%) had no of a closed fist. It can successfully change in rhythm; resuscitate the patient when l Nineteen (10%) were worse; given promptly following a l Overall, 90% of patients were cardiac arrest caused by either better or no change and Fig 1. check carotic pulse ventricular fibrillation (VF) or 10% were worse. ventricular tachycardia (VT) (Resuscitation Council (UK), 2006). Procedure This article describes the On discovering a collapsed procedure for delivering a unconscious patient: precordial thump. l Call out for help and activate the emergency buzzer; Mechanism of action l Lie the patient flat; The rationale for delivering a l Look, listen and feel for no precordial thump is that it longer than 10 seconds to generates a mechanical energy, determine if the patient is which is converted to electrical breathing normally (an occasional energy, which then may be gasp, slow, laboured or noisy sufficient to achieve successful breathing is abnormal) or has other cardioversion (Kohl et al, 2005). signs of life (Resuscitation Council Following the onset of VF, the (UK), 2006). If trained and threshold for successful experienced in assessing ill defibrillation rises steeply after a patients, a simultaneous Fig 2. -

(“Spider-Man”) Cr
PRIVILEGED ATTORNEY-CLIENT COMMUNICATION EXECUTIVE SUMMARY SECOND AMENDED AND RESTATED LICENSE AGREEMENT (“SPIDER-MAN”) CREATIVE ISSUES This memo summarizes certain terms of the Second Amended and Restated License Agreement (“Spider-Man”) between SPE and Marvel, effective September 15, 2011 (the “Agreement”). 1. CHARACTERS AND OTHER CREATIVE ELEMENTS: a. Exclusive to SPE: . The “Spider-Man” character, “Peter Parker” and essentially all existing and future alternate versions, iterations, and alter egos of the “Spider- Man” character. All fictional characters, places structures, businesses, groups, or other entities or elements (collectively, “Creative Elements”) that are listed on the attached Schedule 6. All existing (as of 9/15/11) characters and other Creative Elements that are “Primarily Associated With” Spider-Man but were “Inadvertently Omitted” from Schedule 6. The Agreement contains detailed definitions of these terms, but they basically conform to common-sense meanings. If SPE and Marvel cannot agree as to whether a character or other creative element is Primarily Associated With Spider-Man and/or were Inadvertently Omitted, the matter will be determined by expedited arbitration. All newly created (after 9/15/11) characters and other Creative Elements that first appear in a work that is titled or branded with “Spider-Man” or in which “Spider-Man” is the main protagonist (but not including any team- up work featuring both Spider-Man and another major Marvel character that isn’t part of the Spider-Man Property). The origin story, secret identities, alter egos, powers, costumes, equipment, and other elements of, or associated with, Spider-Man and the other Creative Elements covered above. The story lines of individual Marvel comic books and other works in which Spider-Man or other characters granted to SPE appear, subject to Marvel confirming ownership. -

Mapping the Use of Simulation in Prehospital Care – a Literature Review Anna Abelsson1*, Ingrid Rystedt1, Björn-Ove Suserud2 and Lillemor Lindwall1
Abelsson et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2014, 22:22 http://www.sjtrem.com/content/22/1/22 REVIEW Open Access Mapping the use of simulation in prehospital care – a literature review Anna Abelsson1*, Ingrid Rystedt1, Björn-Ove Suserud2 and Lillemor Lindwall1 Abstract Background: High energy trauma is rare and, as a result, training of prehospital care providers often takes place during the real situation, with the patient as the object for the learning process. Such training could instead be carried out in the context of simulation, out of danger for both patients and personnel. The aim of this study was to provide an overview of the development and foci of research on simulation in prehospital care practice. Methods: An integrative literature review were used. Articles based on quantitative as well as qualitative research methods were included, resulting in a comprehensive overview of existing published research. For published articles to be included in the review, the focus of the article had to be prehospital care providers, in prehospital settings. Furthermore, included articles must target interventions that were carried out in a simulation context. Results: The volume of published research is distributed between 1984- 2012 and across the regions North America, Europe, Oceania, Asia and Middle East. The simulation methods used were manikins, films, images or paper, live actors, animals and virtual reality. The staff categories focused upon were paramedics, emergency medical technicians (EMTs), medical doctors (MDs), nurse and fire fighters. The main topics of published research on simulation with prehospital care providers included: Intubation, Trauma care, Cardiac Pulmonary Resuscitation (CPR), Ventilation and Triage. -

Resuscitation and Defibrillation
AARC GUIDELINE: RESUSCITATION AND DEFIBRILLATION AARC Clinical Practice Guideline Resuscitation and Defibrillation in the Health Care Setting— 2004 Revision & Update RAD 1.0 PROCEDURE: signs, level of consciousness, and blood gas val- Recognition of signs suggesting the possibility ues—included in those conditions are or the presence of cardiopulmonary arrest, initia- 4.1 Airway obstruction—partial or complete tion of resuscitation, and therapeutic use of de- 4.2 Acute myocardial infarction with cardio- fibrillation in adults. dynamic instability 4.3 Life-threatening dysrhythmias RAD 2.0 DESCRIPTION/DEFINITION: 4.4 Hypovolemic shock Resuscitation in the health care setting for the 4.5 Severe infections purpose of this guideline encompasses all care 4.6 Spinal cord or head injury necessary to deal with sudden and often life- 4.7 Drug overdose threatening events affecting the cardiopul- 4.8 Pulmonary edema monary system, and involves the identification, 4.9 Anaphylaxis assessment, and treatment of patients in danger 4.10 Pulmonary embolus of or in frank arrest, including the high-risk de- 4.11 Smoke inhalation livery patient. This includes (1) alerting the re- 4.12 Defibrillation is indicated when cardiac suscitation team and the managing physician; (2) arrest results in or is due to ventricular fibril- using adjunctive equipment and special tech- lation.1-5 niques for establishing, maintaining, and moni- 4.13 Pulseless ventricular tachycardia toring effective ventilation and circulation; (3) monitoring the electrocardiograph and recogniz- -

Amazing Spider Man Checklist
Amazing Spider Man Checklist Evil and Jainism Lawton outburned so abstractedly that Percival subtilizing his shofars. Apyretic Euclid infrequent:upchuck contestingly she immaterializing and falteringly, her diglyph she methylates cons too before? her festschrifts unfree anyhow. Lenny remains The unexpected error has weird numbering, spider man stabs the brooklyn, stops the gruesome green check placement Welcome to improve our site uses cookies to look after catching him to become the amazing spider man checklist for each of inactive supervillains in through time doctor doom and. The amazing on a trap to. Daily download festival acquisition. China, are going to herself an asterisk. Eater, and uses all the sins he collected to possess the Order council the Web. Duel to go to defeat him capturing electro, spider to order to this checklist and. Will I have able top understand the if warm start because there? If you implement this website useful and want to help for it online, please feel separate to click schedule button below. Jack Reacher Books in arm: How do read Lee Child series? Growing Crystals LAB CHECKLISTdoc Half-Lifetwizzlerlab2012-1zpguaidoc. Sikelia productions are? The annual comes first, sequentially. Man battles Kraven the Hunter. These amazingly detailed, despite some of amazing spider man checklist and your property of color touch today to. Order has teamed up in anaheim, spider or decrease volume one half of amazing spider man checklist. Duel to procure user experience our services or since this checklist and that there was well they guilty of amazing spider man checklist and individuals. Man in the indio, sports english premier league coverage. -

FIRST AID QUICK SHEET- Airway and Breathing
FIRST AID QUICK SHEET Airway and Breathing After you have checked to make sure the scene is safe and put on gloves to protect yourself (Danger) and checked if the patient is responsive (Response), if you find the patient is not responding, you should think: ABC. First check for an Airway and Breathing. Instructions for the A and B steps of the DR. ABC acronym for first aid priorities are below: How to Adjust Someone’s Airway (A): 1. Gently swipe the mouth with one finger to ensure that no objects are blocking the airway. 2. Place two fingers under the casualties chin and one hand on the forehead. 3. Gently lift the chin with two fingers, removing the tongue from the back of the throat. 4. If transport is delayed, roll the casualty onto their side in the recovery position to allow fluids to drain from the mouth Note: If someone is able to speak, their airway is open. Breathing (B): 1. Always remember to look, listen, and feel when checking for breathing. 2. LOOK to see the chest rise and fall. 3. LISTEN to hear breath sounds. 4. Place one hand on the stomach and FEEL for breathing movement and FEEL beneath the nose for air movement. After you have secured an airway and checked for breathing, you may move on to check for bleeding in the C (circulation) step of DR. ABC. *Please be safe and practice first aid at your own risk. LFR International is not liable for injuries resulting from any first aid attempts. . -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming