DSM5 Module 6
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EMOTION REGULATION HANDOUT 6 (Emotion Regulation Worksheets 4, 4A) (P
Life Management Associates, LLC 600 Dewey Blvd., Suite B Office: 406-782-4778 Butte, MT 59701 Fax: 406-782-1318 EMOTION REGULATION HANDOUT EMOTION REGULATION HANDOUT 6 (Emotion Regulation Worksheets 4, 4a) (p. 1 of 10) Ways to Describe Emotions ANGER WORDS anger bitterness fury indignation vengefulness aggravation exasperation grouchiness irritation wrath agitation ferocity grumpiness outrage annoyance frustration hostility rage Prompting Events for Feeling Anger • Having an important goal blocked. • Not having things turn out as expected. • You or someone you care about being • Physical or emotional pain. attacked or threatened by others. • Other: • Losing power, status, or respect. Interpretations of Events That Prompt Feelings of Anger • Believing that you have been treated unfairly. • Rigidly thinking, “I’m right.” • Blaming. • Judging that the situation is illegitimate or • Believing that important goals are being wrong. blocked or stopped. • Ruminating about the event that set off the • Believing that things “should” be different anger in the first place. than they are. • Other: Biological Changes and Experiences of Anger • Muscles tightening. • Being unable to stop tears. • Teeth clamping together. • Wanting to hit someone, bang the wall, throw • Hands clenching. something, blow up. • Feeling your face flush or get hot. • Wanting to hurt someone. • Feeling like you are going to explode. • Other: Expressions and Actions of Anger • Physically or verbally attacking. • Clenching your hands or fists. • Making aggressive or threatening gestures. • Frowning, not smiling, mean expression. • Pounding, throwing things, breaking things. • Brooding or withdrawing from others. • Walking heavily, stomping, slamming doors. • Crying. • Walking out. • Grinning. • Using a loud, quarrelsome, or sarcastic voice. • A red or flushed face. -

Mental Health Disorders: Strategies for Approach & Treatment
3/20/2019 Mental Health Disorders: Strategies for Approach & Treatment Transform 2019: OPTA Annual Conference Columbus, Ohio April 6th, 2019 Dawn Bookshar, PT, DPT, GCS Ian Kilbride, PT Marcia Zeiger, OTRL Objectives Participants will: • Understand the prevalence and impact of mental health disorders in client populations • Understand clinical conditions, and associated characteristics of common mental health diagnoses • Apply effective treatment approaches for clients with mental illness. • Produce effective clinical documentation to support intervention for clients with mental illness Mental Illness (MI) www.schizophrenia.com 1 3/20/2019 Mental Illness (MI) The term mental illness refers collectively to all diagnosable mental disorders defined as sustained abnormal alterations in thinking, mood, or behavior associated with distress and impaired functioning which substantially interferes with or limits one or more major life activities. National Institute of Mental Health Prevalence of MI • More than 50% will be diagnosed with a mental illness or disorder at some point in their lifetime. • 1 in 5 Americans will experience a mental illness in a given year. • 1 in 25 Americans lives with a serious mental illness, such as schizophrenia, bipolar disorder, or major depression. Centers for Disease Control & Prevention Prevalence of MI in LTC • 2/3 of people in nursing homes have a mental illness. • Nursing home residents with a primary diagnosis of mental illness range from 18.7% among those aged 65-74 years to 23.5% among those aged 85+ years. • Dementia, Alzheimer disease, and mood disorders are the most common diagnoses of mental illness in long-term care settings. Centers for Disease Control & Prevention 2 3/20/2019 Prevalence of MI in LTC Ohio • Residents with a diagnosis of schizophrenia and bipolar disorder increased from 9% to 16% between 2001 to 2016. -

Trauma: What Lurks Beneath the Surface
\\jciprod01\productn\N\NYC\24-2\NYC204.txt unknown Seq: 1 15-MAR-18 13:45 TRAUMA: WHAT LURKS BENEATH THE SURFACE SARA E. GOLD* Scholarship in the behavioral health field demonstrates that an overwhelming majority of clients experiencing urban poverty, and particularly low-income clients living with chronic medical and mental health issues, have endured trauma as children and adults. While legal scholars and service providers have begun to discuss the role that trauma plays in the client’s interactions with the lawyer, the dialogue has largely focused on trauma relevant to the subject matter of the legal representation. This article expands current scholarship by asserting that given the prevalence of trauma, the lawyer serving the urban poor should presumptively adopt a trauma-informed prac- tice approach regardless of the subject matter of the representation. The lawyer engaging in a trauma-informed practice can enrich the client experience generally and enrich it significantly for the many clients who come to the lawyer-client relationship with a history of trauma. I. INTRODUCTION When we first met Ms. A.,1 she was thirty years old and raising * Clinical Law Instructor, University of Maryland Francis King Carey School of Law. I would like to thank Robert Dinerstein, Naomi Mann, Kate Mitchell, and Jennifer Rosen Valverde who provided invaluable feedback at the 2016 NYU Clinical Law Writers’ Work- shop. I would also like to thank the participants in the 2016 American Association of Law Schools (AALS) Clinical Conference Scholarship Working Group, and the Fall 2016 Uni- versity of Maryland Carey School of Law and University of Baltimore Law School Junior Faculty Workshop for their thoughtful comments and support. -

Attachment Styles and Jealousy Induction in Romantic Relationships
Waking the Green-Eyed Monster: Attachment Styles and Jealousy Induction in Romantic Relationships DIANE WHITSON Although the majority of individuals involved in romantic relationships report having experienced jealousy, relatively little research has examined what factors Saint Louis University lead individuals to attempt to induce jealousy in their romantic partners. We examined how adult attachment is related to individuals’ jealousy-induction * BRENT A. MATTINGLY tendencies. Results indicated that (a) jealousy-induction was positively related to both attachment anxiety and attachment avoidance, (b) specific attachment styles Ashland University (i.e., secure, preoccupied, dismissing, fearful) were not associated with more or fewer jealousy-inducing behaviors, and (c) women tend to induce jealousy more than men. Because jealousy is negatively associated with relationship satisfaction, these findings suggest that insecurely attached individuals’ behaviors may actually be counterproductive in that they are unintentionally making their partners less happy with the relationship. any people can think of a friend or previous have paternal uncertainty (i.e., they are never guaran- romantic partner who has purposely induced teed that a woman’s child is truly their offspring), there Mjealousy in a partner. Because jealousy can is a risk that they might invest valuable resources in have negative outcomes on romantic relationships, it raising another man’s child. As such, they experience would be fruitful to understand why individuals would jealousy when their partner engages in sexual infidelity. desire to deliberately make partners jealous. However, However, women are certain of their maternal status. previous research on jealousy has focused on individuals What is more important, then, is that they obtain and who experience or express jealousy, linking it to both maintain the valued resources of the man so that their commitment and attachment style. -

Sexual Orientations and Perceptions of Jealousy Evanie Eve Atencio Walden University
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2017 Sexual Orientations and Perceptions of Jealousy Evanie Eve Atencio Walden University Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations Part of the Feminist, Gender, and Sexuality Studies Commons This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please contact [email protected]. Walden University College of Social and Behavioral Sciences This is to certify that the doctoral dissertation by Evanie Atencio has been found to be complete and satisfactory in all respects, and that any and all revisions required by the review committee have been made. Review Committee Dr. Scott Friedman, Committee Chairperson, Psychology Faculty Dr. Michael Johnson, Committee Member, Psychology Faculty Dr. Stephen Rice, University Reviewer, Psychology Faculty Chief Academic Officer Eric Riedel, Ph.D. Walden University 2017 Abstract Sexual Orientations and Perceptions of Jealousy by Evanie Atencio MAED, University of Phoenix, 2007 MBA, Regis University, 2002 BS, University of Phoenix, 1998 Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Clinical Psychology Walden University May 2017 Abstract This study examined the participants’ level of jealousy towards their significant other and how it affects the longevity and commitment of their respective relationships. Based on a review of the literature, the research filled the gap of explaining the factor that affects the level of jealousy in monogamous relationships, particularly gender, and sexual orientation. -

1 Rethinking Jealousy Experience and Expression
Rethinking Jealousy Experience and Expression: An Examination of Specialness Meaning Framework Threat and Identification of Retroactive Jealousy Responses Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Jessica Renee Frampton Graduate Program in Communication The Ohio State University 2019 Dissertation Committee Dr. Jesse Fox, Advisor Dr. Kelly Garrett Dr. Shelly Hovick Dr. Roselyn Lee-Won 1 Copyrighted by Jessica Renee Frampton 2019 2 Abstract Extant jealousy models predict jealousy is a response to perceiving a partner’s current or anticipated involvement with a rival as threatening to a relationship’s existence, relational benefits, or self-esteem (e.g., Guerrero & Andersen, 1998; White & Mullen, 1989). Those three threats may explain cases of reactive jealousy, which occurs in response to a partner’s unambiguous involvement with a current rival (Barelds & Barelds-Dijkstra, 2007; Bringle, 1991), but they likely cannot explain cases of retroactive jealousy. Retroactive jealousy entails a negative response to information about a partner’s prior romantic or sexual experiences that occurred before the primary relationship began (Frampton & Fox, 2018b). This type of jealousy is evoked even though the partner is not perceived to be currently romantically or sexually involved with ex-partners. This difference in the nature of retroactive jealousy makes it difficult for current jealousy models to predict retroactive jealousy experience and expression. Two studies were conducted to further explore retroactive jealousy experience and expression. Study 1 experimentally tested predictions about threat to a specialness meaning framework derived from the meaning maintenance model (MMM; Heine, Proulx, & Vohs, 2006; Proulx & Inzlicht, 2012) alongside of predictions about threat to the relationship’s existence, relational benefits, and self-esteem. -

2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry
2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry CİLT | Volume 27 GÜZ | Autumn 2016 EK | Supplement 2: 52. ULUSAL PSİKİYATRİ KONGRESİ TÜRKİYE SİNİR VE ABSTRACTS RUH SAĞLIĞI ISSN 1300 – 2163 DERNEĞİ 2 Türk Psikiyatri Dergisi 2 Mart, Haziran, Eylül ve Aralık aylarında olmak üzere yılda 4 sayı çıkar Turkish Journal of Psychiatry Four issues annually: March, June, September, December CİLT | Volume 27 GÜZ | Autumn 2016 Türkiye Sinir ve Ruh Sağlığı Derneği EK | Supplement 2 tarafından yayınlanmaktadır. ISSN 1300 – 2163 www.turkpsikiyatri.com Türk Psikiyatri Dergisi Bu Sayının Yayın Yönetmeni /Editor in Chief of this Issue Doç. Dr. Semra Ulusoy Kaymak Türkiye Sinir ve Ruh Sağlığı Derneği adına Sahibi ve Sorumlu Müdürü Kongre Başkanları Published by Turkish Association of Nervous and Mental Health Prof. Dr. M. Orhan Öztürk E. Timuçin Oral - Ekrem Cüneyt Evren Düzenleme Kurulu Yayın Yönetmeni/ Editor in Chief Ekrem Cüneyt Evren (Başkan) Prof. Dr. Aygün Ertuğrul Ercan Dalbudak Selim Tümkaya Yazışma Adresi / Corresponding Address Semra Ulusoy Kaymak PK 401, Yenişehir 06442 Ankara Sinan Aydın (Genç Üye) Yönetim Yeri / Editorial Office Bu Sayının Yayın Yönetmen Yardımcıları Kenedi Cad. 98/4, Kavaklıdere, Ankara / Assoc. Editors in Chief of this Issue Telefon: (0-312) 427 78 22 Faks: (0-312) 427 78 02 Sinan Aydın Esra Kabadayı Yayın Türü / Publication Category Selim Tümkaya Yaygın, Süreli, Bilimsel Yayın Yayın Hizmetleri / Publishing Services BAYT Bilimsel Araştırmalar Reklam / Advertisements Basın Yayın ve Tanıtım Ltd. Şti. Reklam koşulları ve diğer ayrıntılar için yayın yönetmeniyle Tel (0-312) 431 30 62, Faks: (0-312) 431 36 02 ilişkiye geçilmesi gerekmektedir. E-posta: [email protected] (Dergide yer alan yazılarda belirtilen görüşlerden yazarlar sorumludur. -

The Grief of Late Pregnancy Loss a Four Year Follow-Up
The grief of late pregnancy loss A four year follow-up Joke Hunfeld The grief of late pregnancy loss A four year follow-up Rouwreacties bij laat zwangerschapsverlies. Een vervolgstudie over vier jaar. Proefschrift Tel' verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnificus Pro£dr P.W.C. Akkermans M.A. en volgens besluit van het college voor promoties. De open bare verdediging zal plaatsvinden op woensdag 13 september 1995 om 15.45 uur door Johanna Aurelia Maria Hunfeld geboren te Utrecht. Promotiecommissie: Promotoren: Pro£ jhr dr J.w, Wladimiroff Pro£ dr E Verhage Overige leden: Pro£ dr H.P. van Geijn Pro£ dr D. Tibboel Pro£ dr Ee. Verhulst Het onderzoek dat in dit proefschrift is beschreven kon worden uitgevoerd dankzij subsidies van Ontwikkelings Geneeskunde, het Universiteitsfonds van de Erasmus Universiteit en het Nationaal Fonds voor de Geestelijke Volksgezondhcid. CIP-gegevens KDninklijke Bibliotheek, Den Haag Hunfeld, J.A.M. The grief onate pregnancy loss / Johanna Aurelia Maria Hunfeld - Delft Eburon P & L Proefschrift Erasmus Universiteit Rotterdam - met samenvatting in het Nederlands ISBN 90-5651-011-8 Nugi Trefw;: perinatal grief Distributie: Eburon P&L, Postbus 2867, 2601 CW Delft Drukwerk: Ponsen & Looijen BY, Wageningen Lay-out verzorging: A. Praamstra All rights reserved Omslagtekening © P. Picasso, 1995 do Becldrecht Amsterdam © Joke Hunfeld, 1995 Rouwreacties bij laat zwangerschapsverlics Eell vcrvolgstudie over vier jaar Contents 1 Theoretical and empirical background -
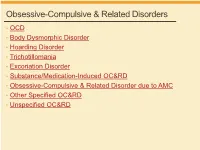
Obsessive-Compulsive & Related Disorders
Obsessive-Compulsive & Related Disorders • OCD • Body Dysmorphic Disorder • Hoarding Disorder • Trichotillomania • Excoriation Disorder • Substance/Medication-Induced OC&RD • Obsessive-Compulsive & Related Disorder due to AMC • Other Specified OC&RD • Unspecified OC&RD B Chow 2019 OCD OCD – Diagnostic Criteria A. Obsessions, compulsions, or both: 1. Obsessions (2/2) • Recurrent thoughts/urges/images, intrusive + unwanted, distressing • Attempts to supress, ignore or neutralize 2. Compulsions (2/2) • Repetitive behaviors, feels driven to do, due to obsession or rules • Aimed to prevent anxiety/distress, but not connected or excessive B. Time-consuming, or sig distress/impairment C. Not due to substance or AMC D. Not better explained by AMD DSM5 OCD – Diagnostic Specifiers • Specify if: • With good or fair insight: recognizes definitely/probably not true • With poor insight: thinks probably true • With absent insight/delusional beliefs: convinced beliefs are true • Specify if: • Tic-related: current OR past hx of tic disorder DSM5 OCD – Diagnostic Specifiers • Dysfunctional beliefs • Inflated sense of responsibility, tendency to overestimate threat • Perfectionism, intolerance of uncertainty • Over-importance of thoughts, need to control thoughts • Degree of insight → accuracy of beliefs, can vary over course • Good/fair insight → many • Poor insight → some • Absent insight/delusional beliefs → 4% or less • Poorer insight → worse long-term outcome • Tic disorders → 30% of OCD have lifetime tic disorder • Most common in MALES with childhood-onset -

Sex Differences in Feelings of Guilt Arising from Infidelity
Evolutionary Psychology www.epjournal.net – 2008. 6(3): 436-446 ¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯ Original Article Sex Differences in Feelings of Guilt Arising from Infidelity Maryanne Fisher, Department of Psychology, St. Mary’s University, Halifax, Canada. Email: [email protected] (Corresponding author) Martin Voracek, Department of Basic Psychological Research, University of Vienna, Vienna, Austria P. Vivien Rekkas, Department of Psychology, University of Toronto (Scarborough), Toronto, Canada Anthony Cox, Centre for Psychology and Computing, Halifax, Canada Abstract: Although there is extensive literature regarding sex differences in jealousy due to infidelity, guilt resulting from infidelity remains unexplored. We hypothesize that men will feel guiltier from imagined emotional rather than sexual infidelity, as it is most important for their partner’s reproductive success. Similarly, we predict that women will feel more guilt from imagined sexual rather than emotional infidelity. The findings indicate a different pattern; men feel guiltier following sexual infidelity, whereas women feel guiltier following emotional infidelity. Results also show that both sexes believe their partners would have a more difficult time forgiving sexual, rather than emotional, infidelity, but women and not men report that sexual infidelity would more likely lead to relationship dissolution. These findings are discussed in view of evolved mating strategies and individual reproductive success. Keywords: infidelity, sex differences, guilt, mate selection. ¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯ Introduction Infidelity in romantic relationships is far from rare; recent national surveys of Americans have documented that between approximately 20 to 25% of respondents report at least one sexual affair during their lifetime (Atkins, Baucom, and Jacobson, 2001; Laumann, Gagnon, Michael, and Michaels, 1994). All infidelity is not the same, however, as women and men apparently do not perceive their affairs in an equivalent manner. -

Cognitive-Behavioural Therapy of Obsessive- Compulsive Disorder
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Veterinary medicine - Repository of PHD, master's thesis UNIVERSITY OF ZAGREB SCHOOL OF MEDICINE Veronika Nives Zoric Cognitive-Behavioural Therapy of Obsessive- Compulsive Disorder GRADUATE THESIS Zagreb, 2017. This graduate thesis was made at the Department of Psychiatry KBC Zagreb, University of Zagreb School of Medicine, mentored by prof. dr. sc. Dražen Begić and was submitted for evaluation in the 2016/2017 academic year. Mentor: prof. dr. sc. Dražen Begić ABBREVIATIONS USED IN THE TEXT: Behaviour Therapy (BT) Bibliotherapy administered CBT (bCBT) Cognitive-Behavioural Therapy (CBT) Cognitive Therapy (CT) Computerized CBT (cCBT) Danger Ideation Reduction Therapy (DIRT) Deep Brain Stimulation (DBS) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Exposure and Response Prevention (ERP) Generalized Anxiety Disorder (GAD) International Classification of Disease (ICD-10) Internet-administered CBT (iCBT) Major Depressive Disorder (MDD) Monoamine Oxidase Inhibitors (MAO) Obsessive-Compulsive Disorder (OCD) Obsessive-Compulsive Personality Disorder (OCPD) Selective Serotonin Reuptake Inhibitor (SSRI) Serotonin; 5-hydroxytryptamine (5HT) Serotonin Reuptake Inhibitor (SRI) Subjective Units of Distress Scale (SUDS) Telephone administered CBT (tCBT) Tricyclic Antidepressants (TCA) Videoconferencing administered CBT (vCBT) Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) TABLE OF CONTENTS 1. SUMMARY 2. SAŽETAK 3. INTRODUCTION ............................................................................................................ -

Library of Research Articles on Veterans and Complementary and Integrative Health Therapies
The VA Office of Patient Centered Care and Cultural Transformation’s and VA Complementary and Integrative Health Evaluation Center’s Library of Research Articles on Veterans and Complementary and Integrative Health Therapies April, 2020 1 Library of Research Articles on Veterans and Complementary and Integrative Health Therapies We are pleased to announce the VA Office of Patient Centered Care and Cultural Transformation’s (OPCC&CT) and VA Complementary and Integrative Health Evaluation Center’s (CIHEC) “Library of Research Articles on Veterans and Complementary and Integrative Health Therapies”. The Library is comprised of two sections: 1) Articles organized by type of CIH therapies, among the nine therapies that the VA considers medical treatments and 2) Articles organized by type of health outcome, among nine outcomes (i.e., pain, anxiety, depression, post-traumatic stress disorder (PTSD), substance/opioid abuse, stress and wellbeing, insomnia, suicide, and Veteran caregiver wellbeing and VA employee wellbeing). The Library provides the citation (with links to either the actual article or to its page in PubMed) as well as the abstract, if available. Although every attempt was made to include all relevant studies conducted, it is possible we missed some and will gladly include additional studies when found. The Library will be updated biannually, with the next update available in June 2020. It can be found at the OPCC&CT website at https://www.va.gov/wholehealth/ and the CIHEC website at https://www.hsrd.research.va.gov/centers/cshiip.cfm. For questions on the Library, please contact both Stephanie L. Taylor, PhD (Director of CIHEC) [email protected] and Mr.