Metabolic Risk Markers and Relative Survival in Patients with Aortic Stenosis Requiring Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vrijdagfriday 11
VRIJVRIJDAGFRIFRIDAY CHECK DE MONITORENVOOR LAATSTE VOOR PROGRAMMAWIJZIGINGENWIJZIGINGENFOR LATEST CHANGES:PLEASE CHECK WWW.NORTHSEAJAZZ.COM THE SCREENS FOR LATEST CHANGES 1111 AHOY OPEN 16.30 h. 16.30 17.00 17.30 18.00 18.30 19.00 19.30 20.00 20.30 21.00 21.30 22.00 22.30 23.00 23.30 00.00 00.30 01.00 01.30 ARTIST IN RESIDENCE CLEO LAINE OMARA BOBBY McFERRIN JOHN DANKWORTH PORTUONDO CRISTINA with BRANCO AMAZONAMAZON NDR BIG BAND AND FRIENDS ’GRACIAS’ HANK JONES 90TH BIRTHDAY CONCERT MARIA SCHNEIDER CHARLES LLOYD with HERBIE HANCOCK NILS FISCHER ORCHESTRA QUARTET ROY HARGROVE & QUINTET & TIMBAZO HUDSONHUDSON ROBERTA GAMBARINI ZUCO 103 AL JARREAU SERGIO MENDESANGIE STONE BOOTSY COLLINS NILENILE A TRIBUTE TO JOE ZAWINUL with the ALAIN CLARK LEE RITENOUR JILL SCOTT METROPOLE ORCHESTRA MAASMAAS conducted by VINCE MENDOZA LARGE & LOUD THE NUBLU NEW COOL MATTHEW ORCHESTRA FLAT EARTH HERBERT conducted by SOCIETY MEETS COLLECTIVE BIG BAND LAWRENCE D. JIMI TENOR with CONGOCONGO ”BUTCH” MORRIS JULES DEELDER ELIZABETH LAURA YUYUKONON SHEPHERD IZIBOR FINK dbCLIFFORD ’THE MUSIC OF IVAN LINS’ HANS TEEUWEN CASSANDRA featuring IVAN LINS MARK MURPHY ZINGT! WILSON special guest DARLINGARLING NNENNA FREELON AHOY OPEN 16.30 h. 16.30 17.00 17.30 18.00 18.30 19.00 19.30 20.00 20.30 21.00 21.30 22.00 22.30 23.00 23.30 00.00 00.30 01.00 01.30 PIANO ROOM NORTH SEA JAZZ RON CARTER ABDULLAH COMPOSITION ’DEAR MILES’ ASSIGNMENT PAUL BLEY ELIANE ELIAS featuring IBRAHIM MADEIRAMADEIRA JEROEN VAN VLIET STEPHEN SCOTT TRIO AND THE WINNER IS.. -

Boklista 1949–2019
Boklista 1949–2019 Såhär säger vår medlem som har sammanställt listan: ”Det här är en lista över böcker som har getts ut under min livstid och som finns hemma i min och makens bokhyllor. Visst förbehåll för att utgivningsåren inte är helt korrekt, men jag har verkligen försökt skilja på utgivningsår, nyutgivning, tryckår och översättningsår.” År Författare Titel 1949 Vilhelm Moberg Utvandrarna Per Wästberg Pojke med såpbubblor 1950 Pär Lagerkvist Barabbas 1951 Ivar Lo-Johansson Analfabeten Åke Löfgren Historien om någon 1952 Ulla Isaksson Kvinnohuset 1953 Nevil Shute Livets väv Astrid Lindgren Kalle Blomkvist och Rasmus 1954 William Golding Flugornas herre Simone de Beauvoir Mandarinerna 1955 Astrid Lindgren Lillebror och Karlsson på taket 1956 Agnar Mykle Sången om den röda rubinen Siri Ahl Två små skolkamrater 1957 Enid Blyton Fem följer ett spår 1958 Yaşar Kemal Låt tistlarna brinna Åke Wassing Dödgrävarens pojke Leon Uris Exodus 1959 Jan Fridegård Svensk soldat 1960 Per Wästberg På svarta listan Gösta Gustaf-Jansson Pärlemor 1961 John Åberg Över förbjuden gräns 1962 Lars Görling 491 1963 Dag Hammarskjöld Vägmärken Ann Smith Två i stjärnan 1964 P.O. E n q u i st Magnetisörens femte vinter 1965 Göran Sonnevi ingrepp-modeller Ernesto Cardenal Förlora inte tålamodet 1966 Truman Capote Med kallt blod 1967 Sven Lindqvist Myten om Wu Tao-tzu Gabriel García Márques Hundra år av ensamhet 1968 P.O. E n q u i st Legionärerna Vassilis Vassilikos Z Jannis Ritsos Greklands folk: dikter 1969 Göran Sonnevi Det gäller oss Björn Håkansson Bevisa vår demokrati 1970 Pär Wästberg Vattenslottet Göran Sonnevi Det måste gå 1971 Ylva Eggehorn Ska vi dela 1972 Maja Ekelöf & Tony Rosendahl Brev 1 År Författare Titel 1973 Lars Gustafsson Yllet 1974 Kerstin Ekman Häxringarna Elsa Morante Historien 1975 Alice Lyttkens Fader okänd Mari Cardinal Orden som befriar 1976 Ulf Lundell Jack 1977 Sara Lidman Din tjänare hör P.G . -

Könsfördelning I Två Läromedel I Ämnet Svenska För Årskurs 9
Beteckning: Institutionen för humaniora och samhällsvetenskap Könsfördelning i två läromedel i ämnet Svenska för årskurs 9. Annakarin Johansson Februari 2009 Examensarbetet/uppsats/30hp/C-nivå Svenska/Litteraturdidaktik LP90/Examensarbet Examinator: Janne Lindqvist Grinde Handledare: Sarah Ljungquist 0 Innehållsförteckning 1. Inledning 2. 1.1 Urval 2. 1.2 Syfte och tes 3. 1.3 Frågeställningar 3. 1.4 Metod 3. 1.5 Begreppen kön och genus 4. 1.6 Begreppet kanon 5. 2. Närläsning av samt urval ur Uppdrag Svenska 3 samt Studio Svenska 4 6. 2.1 Uppdrag Svenska 3 (US3) 6. 2.1.1 Kommentarer till US3 14. 2.2 Studio Svenska 4 (SS4) 18. 2.2.1 Kommentarer till SS4 24. 3. Jämförelse mellan Uppdrag Svenska 3 och Studio Svenska 3 samt slutsats 27. 4. Sammanfattning 31. Litteraturlista 32. 1 1. Inledning När verkligheten ska beskrivas måste den förenklas. Den är helt enkelt för komplex för att beskrivas fullständigt och rättvisande. Detta kan ske genom användning av en modell. Modellen innebär en avgränsning, som i sig innebär att man väljer bort förhållanden eller perspektiv som är betydelsefulla för den totala förståelsen. Det är alltså väldigt viktig hur man "bygger sin modell" och att tala om hur man har gjort, eftersom modellen i sig innebär avsteg från verkligheten. Ett genusperspektivet bidrar till är att justera tidigare medvetna eller omedvetna "modellbyggen" som gör kvinnan till det andra könet1. I strävan mot ett jämställt samhälle är det viktigt att kunna utgå från en bild av verkligheten som är så riktig som möjligt för att kunna åstadkomma en framtida förändring. Litteraturen tecknar bilder av världen och den komplicerade tillvaron ur många erfarenheter, i många former, med många perspektiv. -

Doris Nr 39 2021
Nr 39 2021 FRÅN HARRY MARTINSON-SÄLLSKAPET HARRY FRÅN 1 Omorientering och framåtblick – låt oss gå stärkta ur pandemin För fem år sedan valdes jag till ordförande i Jämshög. Jag minns tydligt den utspruckna bokskogen som alldeles nyligen kastat en tunn grön slöja omkring sig i en plötslig självmedveten het över vårsolens oblyga blickar. Jag minns gemenskapen i folk högskolans samlingssal, en gemenskap som för mig, i mitt minne, lyser starkare än någon vårsol. Och som jag saknar den gemenskapen. Som jag saknar kulturupplevelserna med Harry Martinsonsällskapet men också i andra sammanhang. Under coronaåret har det blivit tydligt vad dessa gemensamma upp levelser betyder, för de lyser som en minnets polstjärna och inger hopp i tider av social distansering och kulturell svältkost. öjligheten att skapa liknande gemensamma minnen uteblev dessvärre eftersom såväl Majdagarna i Jämshög 2020 som i Göteborg 2021 fick ställas in. De flesta av sällskapetsM ordinarie aktiviteter var digitala eller inställda men tack vare vår starka närvaro på sociala medier och hemsidan kunde vi fortsätta vidga och fördjupa intresset för Harry Martinsons liv och författarskap på ett framgångsrikt sätt. Styrelsen ställde också snabbt om till videomöten och vi kunde på så sätt fortsätta bedriva vår kärnverksamhet trots omständigheterna. En av de stora Harry Martinson-händelserna under året var utgivningen av Reine Bry- nolfssons uppläsning av Vägen till Klockrike. Medlemmarna erbjöds en två månader lång provperiod på streamingtjänsten BookBeat för att ha möjlighet att lyssna på uppläsningen. Ingen av oss vet hur länge vi får leva med restriktioner och begräns- ningar på grund av pandemin. Bakom oss har vi förluster av olika slag. -

The Historian-Filmmaker's Dilemma: Historical Documentaries in Sweden in the Era of Häger and Villius
ACTA UNIVERSITATIS UPSALIENSIS Studia Historica Upsaliensia 210 Utgivna av Historiska institutionen vid Uppsala universitet genom Torkel Jansson, Jan Lindegren och Maria Ågren 1 2 David Ludvigsson The Historian-Filmmaker’s Dilemma Historical Documentaries in Sweden in the Era of Häger and Villius 3 Dissertation in History for the Degree of Doctor of Philosophy presented at Uppsala University in 2003 ABSTRACT Ludvigsson, David, 2003: The Historian-Filmmaker’s Dilemma. Historical Documentaries in Sweden in the Era of Häger and Villius. Written in English. Acta Universitatis Upsalien- sis. Studia Historica Upsaliensia 210. (411 pages). Uppsala 2003. ISSN 0081-6531. ISBN 91-554-5782-7. This dissertation investigates how history is used in historical documentary films, and ar- gues that the maker of such films constantly negotiates between cognitive, moral, and aes- thetic demands. In support of this contention a number of historical documentaries by Swedish historian-filmmakers Olle Häger and Hans Villius are discussed. Other historical documentaries supply additional examples. The analyses take into account both the produc- tion process and the representations themselves. The history culture and the social field of history production together form the conceptual framework for the study, and one of the aims is to analyse the role of professional historians in public life. The analyses show that different considerations compete and work together in the case of all documentaries, and figure at all stages of pre-production, production, and post-produc- tion. But different considerations have particular inuence at different stages in the produc- tion process and thus they are more or less important depending on where in the process the producer puts his emphasis on them. -

Salomonsson Agency Fall 2018
Fall 2018 Spring 2018 r e n a K s e L : o t o h p r e v o C SALOMONSSON AGENCY Götgatan 27 | Stockholm | Sweden | PHONE +46 8 22 32 11 | EMAIL [email protected] | INTERNET www.salomonssonagency.com LITERARY FICTION Jonas Gardell JoNAS GARDELL (b. 1963) is one of the greatest and most distinctive voices in Swedish literature today. Since his literary debut in 1985, the novelist, playwright, screenwriter and comedian Gardell has time and again mesmerized the reading audience with moving, stylistically immaculate prose that ricochets off the page. His unique mixture of humor and heartbreaking episodes fetched from his own life as a member of the LGBTQ community has made Gardell a trendsetting authorship in Scandinavia. Deeply personal, utterly unfazed by taboos, and with a humor you can’t guard against, he is finally back with the national No. 1 bestseller, In Memory of an Unconditional Love . Till minne av en villkorslös kärlek (In Memory of an Unconditional Love) In Memory of an Unconditional Love is the story of the (in fiction) late author Jonas Gardell RiGhTS SoLD and his family. A family that is much like any other, except perhaps for the creative way in Finland, Johnny Kniga which it handles weakness. In the Gardell family, secrets and unwanted truths have a Sweden, Norstedts tendency to change shape, transforming into legends that – much like a skillfully executed magic trick – dazzle the eye with a prettier truth. The best teller of such legends was without a doubt Ingegärd Rasmussen, Jonas’ loving mother. The eccentric Free Church-raised Ingegärd, born in the not-so-roaring Swedish twenties, was a woman surrounded on all sides by obstacles dictating what a woman should be. -

Kup Bilet - Sprzeda Ż Bezpo Średnia
Bydgoszcz Jazz Festival 11 edycja festiwalu zapowiada się bardzo imponująco. Koncert inauguracyjny będzie wydarzeniem muzycznym , który na długo pozostanie w naszej pamięci i naszych sercach. Najwybitniejsi muzycy jazzowi dzisiejszych czasów odwiedzą Bydgoszcz. Mike Stern Band to grupa złożona z samych gwiazd światowego formatu. Koncert w Operze Nova będzie pierwszym koncertem zespołu na trasie europejskiej. Muzycy będą mieszkali w Bydgoszczy dwa dni więc będzie okazja do spotkania się z nimi już bardziej prywatnie, a jest planowane również jam session z ich udziałem w klubie Eljazz. Kolejne koncerty również bardzo ciekawe odbywać sie będą na terenie Bydgoszczy w różnych miejscach. Po raz pierwszy koncert festiwalowy odbędzie się w sali Miejskiego Centrum Kultury , na którym wystąpi Krystyna Stańko z zespołem. Bardzo ciekawie zapowiada się koncert w Auli Copernikanum w której wystąpią dwa zespoły w tym gitarzyści z egzotycznych krajów Meksyku i Wenezueli. Koncert w klubie Eljazz tria Macieja Fortuny z kanadyjskim fenomenalnym perkusistą Tylerem Hornby będzie kolejnym wydarzeniem przypominającym koncerty w najlepszych klubach świata takich jak Birldland czy Village Vanguard Dużym wydarzeniem artystycznym będą tegoroczne Zaduszki Jazzowe w Teatrze Polskim , gdzie heppeningowe prezentacje projektu Ananke wprowadzą słuchaczy w świat pełen wrażeń i przeżyć artystycznych. Po przewie tradycyjnie już zamknie festiwal będący w doskonałej formie Eljazz Quintet. Te ciekawe propozycje muzyczne sprawią, że w drugiej połowie października będziemy mieli w Bydgoszczy prawdziwe święto jazzu. KUP BILET - SPRZEDA Ż BEZPO ŚREDNIA • ELJAZZ, UL. KRĘTA 3, BYDGOSZCZ - TU MOŻNA KUPIĆ BILETY NA WSZYSTKIE KONCERTY FESTIWALOWE • OPERA NOVA, UL. FOCHA, BYDGOSZCZ - TU MOŻNA KUPIĆ BILETY NA KONCERT MIKE STERN BAND • MCK, UL. MARCINKOWSKIEGO, BYDGOSZCZ - TU MOŻNA KUPIĆ BILETY NA KONCERT KRYSTYNY STAŃKO • TEATR POLSKI, UL. -

Blues Are the Roots and the Other Are the Fruitswillie Dixon (1915-1985) Forsalg: • Jysk Musikteater • Bibliotekerne I Silkeborg
BLUES I SilKEBORG b’ShARp • SILKEBORG RhyTHM’N BLUES ASSOCIATION • FORÅR 2017 LEVERANDØR AF BLUES GENNEM MERE END 20 ÅR Sønd. d. 22. januar kl. 14 - 17 • døren åbner kl. 13.30 • entre: 30.- (ingen forSalg) lør. d. 11/3 kl. 21 • døren åbner kl. 20.30 • entre: 140.- forSalg: 110.- medl.: 80.- lørd. d. 2/4 kl. 20 • døren åbner kl. 19.30 • entre: 170.- forSalg: 140.- medl.: 100.- ÅBEN BLUES JAM M. HP LANGE FRIED OKRA BAND THE YOUNG GENERATION OF BLUES + GENERALFORSAMLING IDA BANG & The BLuE Tears (S) 21.45-23.30 HP har spillet i mere end 35 år på festivaler, spillesteder, værtshuse og i alle afkroge i Danmark. Det er hvad Dan- En trio fra København, bestående af Morten Lunn (vokal, Ida Bang & The Blue Tears er et ungt svensk bluesband marks bedste old school guitarist, HP Lange, kan skrive guitar & diddley bow), Thomas Foldberg (guitar) og Tho- med base i Stockholm. I 2015 vandt de Swedish Blues på sit visitkort. Country- & Mississippi blues af høj klasse! mas Crawfurd (trommer, mandolin, mandola og percussi- Challenge og repræsenterede Sverige i European Blues Denne eftermiddag skal han holde styr på en masse mu- on). Med den besætning adskiller bandet sig fra meget i Challenge i Italien i 2016. Bandet udgav deres første CD sikere som forhåbentlig dukker op og vil jamme med HP. både blues og rockverdenen og mange har da også fået ‘Possibilities’ i 2013. Frontfigur i bandet er den 26-årige Vi lover at det ikke bliver kedeligt. ørene op for den basløse trio. Bandet har taget deres mu- sangerinde Ida Bang. -
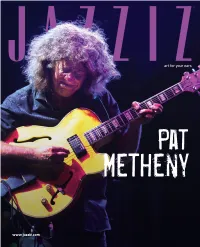
JAZZIZ-Metheny-Interviews.Pdf
Pat Metheny www.jazziz.com JAZZIZ Subscription Ad Lage.pdf 1 3/21/18 10:32 AM Pat Metheny Covered Though I was a Pat Metheny fan for nearly a decade before I special edition, so go ahead and make fun if you please). launched JAZZIZ in 1983, it was his concert, at an outdoor band In 1985, we published a cover story that included Metheny, shell on the University of Florida campus, less than a year but the feature was about the growing use of guitar synthesizers before, that got me to focus on the magazine’s mission. in jazz, and we ran a photo of John McLaughlin on the cover. As a music reviewer for several publications in the late Strike two. The first JAZZIZ cover that featured Pat ran a few ’70s and early ’80s, I was in touch with ECM, the label for years later, when he recorded Song X with Ornette Coleman. whom Metheny recorded. It was ECM that sent me the press When the time came to design the cover, only photos of Metheny credentials that allowed me to go backstage to interview alone worked, and Pat was unhappy with that because he felt Metheny after the show. By then, Metheny had recorded Ornette should have shared the spotlight. Strike three. C around 10 LPs with various instrumental lineups: solo guitar, A few years later, I commissioned Rolling Stone M duo work with Lyles Mays on the chart-topping As Wichita Fall, photographer Deborah Feingold to do a Metheny shoot for a Y So Falls Wichita Falls, trio, larger ensembles and of course his Pat cover story that would delve into his latest album at the time. -

Kurslitteratur NS112U, Svenskt Språk Och Svensk Litteratur, 10 Hp Litteraturlistan Är Fastställd Av Institutionsstyrelsen 2020-05-06
Kurslitteratur NS112U, Svenskt språk och svensk litteratur, 10 hp Litteraturlistan är fastställd av institutionsstyrelsen 2020-05-06. Gäller fr.o.m. 1 juli 2020. Med reservation för ev. ändringar p.g.a. utgången litteratur e.d. Språkvetenskap: Bijvoet, Ellen & Fraurud, Kari. 2013. ”Rinkebysvenska” och andra konstruktioner av språklig variation i dagens flerspråkiga Sverige. I: K. Hyltenstam & I. Lindberg (red.), Svenska som andraspråk – i forskning, undervisning och samhälle (2:a uppl.). Lund: Studentlitteratur. (15 s.) (Finns i kursplattformen.) Deklaration om nordisk språkpolitik. 2006. Nordiska ministerrådet ANP 2007:746. (96 s.) http://norden.diva-portal.org/smash/get/diva2:700895/FULLTEXT01.pdf (5 april 2020) Hellberg, Staffan. 2007. Expressen, Pippi och modern svenska. Språkvård 2007/1. S. 38–44. (7 s.) https://isof.se/download/18.42699e142b734b551698/1529494720672/Spr%C3%A5kv%C3 %A5rd%202007-1.pdf (5 april 2020) Josephson, Olle. 2012. Den nordiska språkgemenskapen. En språkpolitisk jämförelse. 14 s. (Bearbetad svenskspråkig version av artikeln ”La communauté linguistique nordique. Éléments de comparaison des politiques linguistiques dans les pays nordiques.” publicerad i Nordiques. No 24. Automne 2012. (Bibliothèque de Caen. Association Norden). S. 17– 36.) (20 s.) (Finns i kursplattformen.) Kotsinas, Ulla-Britt. 1989. Stockholmsspråk genom 100 år. Tijdschrift voor Skandinavistiek. 1–2/10. S. 14–37. (23 s.) http://rjh.ub.rug.nl/tvs/article/view/10264 (5 april 2020) Kotsinas, Ulla-Britt. 1991. Attityder till Stockholmsspråk. I: K.-L. Berge, U.-B. & Kotsinas, U.-B. (red.), Storstadsspråk och storstadskultur i Norden. MINS 34. Institutionen för nordiska språk. Stockholms universitet. 163–184. (22 s.) (Finns i kursplattformen.) Nelson, Marie. Under utgivning. Språksituationen på Åland – speciell, om inte unik. -

Osobnosť Pata Methenyho
JANÁČKOVA AKADÉMIA MÚZICKÝCH UMENÍ V BRNE HUDOBNÁ FAKULTA Katedra jazzovej interpretácie Jazzová interpretácia Osobnosť Pata Methenyho Bakalárska práca Autor práce: Samuel Marinčák Vedúci práce: MgA. Vilém Spilka Oponent práce: MgA. Jan Dalecký Brno 2014 Bibliografický záznam MARINČÁK, Samuel. Osobnosť Pata Methenyho /Personality of Pat Metheny/ Brno : Janáčkova akadémia múzických umení v Brne, Hudobná fakulta, Katedra jazzovej interpretácie, 2014, 36 s, vedúci práce : MgA. Vilém Spilka Anotácia Bakalárska práca je zameraná na osobnosť jednej z najväčších postáv vo svete jazzu v súčasnosti. Ponúka zaujímavé informácie o jeho živote, kariére, diskografii a o mnohých iných aspektoch súvisiacich s ním. Kľúčové slová jazz, improvizácia, biografia, diskografia, ocenenia, zvuk Annotation This bachelor thesis is focused on the life and work of one of the greatest artists in the world of jazz. It will offer you a very interesting insight to his life, career, discography and other aspects connected to him. Key Words jazz, improvisation, biography, discography, awards, sound Prehlásenie: Prehlasujem, že som predloženú prácu spracoval samostatne, s použitím uvedených zdrojov a prameňov. Zároveň dávam zvolenie k tomu, aby táto práca bola umiestnená v Knižnici JAMU a slúžila na študijné účely. V Brne, dňa 28.7.2014 Samuel Marinčák Poďakovanie: Na tomto mieste by som sa rád poďakoval vedúcemu mojej práce MgA. Vilémovi Spilkovi a oponentovi MgA. Janovi Daleckému, ktorí ma pri písaní usmerňovali a ponúkli mi cenné rady. Obsah Úvod ............................................................................................................................ -

March/April 2004 Issue 267 Free Aged 30 Years
March/April 2004 Issue 267 Free Aged 30 Years www.jazz-blues.com March/April 2004 • Issue 267 Published by Martin Wahl Communications Editor & Founder Bill Wahl Layout & Design Bill Wahl Operations Jim Martin Pilar Martin Contributors Michael Braxton, Mark Cole, Chris Hovan, Nancy Ann Lee, David McPherson, Peanuts, Mark Smith, Duane Verh and Ron Cleveland’s jazz festival – Weinstock. 25 years and still swingin’!! Check out our new, updated web For 25 years Highlighting the season are two gala con- page. Now you can search for CD Tri-C JazzFest certs with special performances by Diana Reviews by artists, Titles, Record Cleveland has Krall, George Benson, Joe Sample, Dr. Labels or JBR Writers. Twelve years of reviews are up and we’ll be going been presenting John, Christian McBride, the Clayton- all the way back to 1974! the brightest jazz Hamilton Jazz Orchestra, and a host of luminaries – from others. In addition, we acknowledge Address all Correspondence to.... young lions to the Cleveland’s contributions to the jazz world Jazz & Blues Report legends. Beyond through performances by Joe Lovano, 19885 Detroit Road # 320 world-class per- Jimmy Scott, and an exploration of the Rocky River, Ohio 44116 formances, JazzFest is nationally recog- works of composer Tadd Dameron. Main Office ...... 216.651.0626 nized as a dynamic force for jazz educa- Our 25th anniversary season truly of- Editor's Desk ... 440.331.1930 tion, reaching more than 20,000 students fers something for every jazz palate, along annually through clinics, workshops and with our offering of world-class educational [email protected] in-school performances.