A Case of Dimethoate Poisoning Requiring Prolonged Skin Decontamination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
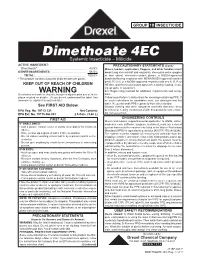
Dimethoate 4EC Systemic Insecticide – Miticide ACTIVE INGREDIENT: PRECAUTIONARY STATEMENTS (Cont.) Dimethoate*
GROUP 1B INSECTICIDE Dimethoate 4EC Systemic Insecticide – Miticide ACTIVE INGREDIENT: PRECAUTIONARY STATEMENTS (Cont.) Dimethoate* .......................................................... 43.5% Mixers, loaders, applicators, flaggers, and other handlers must OTHER INGREDIENTS: .......................................... 56.5% wear: Long-sleeved shirt and long pants, shoes plus socks, goggles TOTAL: .............................................................. 100.0% or face shield, chemical-resistant gloves, a NIOSH-approved * This product contains 4 pounds of dimethoate per gallon. dust/mist filtering respirator with MSHA/NIOSH approval number prefix TC-21C or a NIOSH-approved respirator with any N, R, P, or KEEP OUT OF REACH OF CHILDREN HE filter, and chemical-resistant apron when mixing, loading, clean- ing up spills, or equipment. WARNING See Engineering Controls for additional requirements and excep- Si usted no entiende la etiqueta, busque a alguien para que se la ex- tions. plique a usted en detalle. (If you do not understand the label, find Follow manufacturer’s instructions for cleaning/maintaining PPE. If someone to explain it to you in detail.) no such instructions for washables exist, use detergent and hot water. Keep and wash PPE separately from other laundry. See FIRST AID Below Discard clothing and other absorbent materials that have been EPA Reg. No. 19713-231 Net Content: drenched or heavily contaminated with this product’s concentrate. EPA Est. No. 19713-GA-001 2.5 Gals. (9.46 L) Do not reuse them. ENGINEERING CONTROLS FIRST AID Mixers and loaders supporting aerial application to alfalfa, cotton, IF SWALLOWED: soybeans, corn, safflower, sorghum, and wheat, must use a closed • Call a poison control center or doctor immediately for treatment system that meets the requirements listed in the Worker Protections advice. -

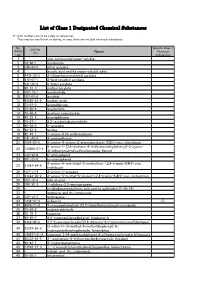
Chemical Name Federal P Code CAS Registry Number Acutely
Acutely / Extremely Hazardous Waste List Federal P CAS Registry Acutely / Extremely Chemical Name Code Number Hazardous 4,7-Methano-1H-indene, 1,4,5,6,7,8,8-heptachloro-3a,4,7,7a-tetrahydro- P059 76-44-8 Acutely Hazardous 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide P050 115-29-7 Acutely Hazardous Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- P197 17702-57-7 Acutely Hazardous 1-(o-Chlorophenyl)thiourea P026 5344-82-1 Acutely Hazardous 1-(o-Chlorophenyl)thiourea 5344-82-1 Extremely Hazardous 1,1,1-Trichloro-2, -bis(p-methoxyphenyl)ethane Extremely Hazardous 1,1a,2,2,3,3a,4,5,5,5a,5b,6-Dodecachlorooctahydro-1,3,4-metheno-1H-cyclobuta (cd) pentalene, Dechlorane Extremely Hazardous 1,1a,3,3a,4,5,5,5a,5b,6-Decachloro--octahydro-1,2,4-metheno-2H-cyclobuta (cd) pentalen-2- one, chlorecone Extremely Hazardous 1,1-Dimethylhydrazine 57-14-7 Extremely Hazardous 1,2,3,4,10,10-Hexachloro-6,7-epoxy-1,4,4,4a,5,6,7,8,8a-octahydro-1,4-endo-endo-5,8- dimethanonaph-thalene Extremely Hazardous 1,2,3-Propanetriol, trinitrate P081 55-63-0 Acutely Hazardous 1,2,3-Propanetriol, trinitrate 55-63-0 Extremely Hazardous 1,2,4,5,6,7,8,8-Octachloro-4,7-methano-3a,4,7,7a-tetra- hydro- indane Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]- 51-43-4 Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]-, P042 51-43-4 Acutely Hazardous 1,2-Dibromo-3-chloropropane 96-12-8 Extremely Hazardous 1,2-Propylenimine P067 75-55-8 Acutely Hazardous 1,2-Propylenimine 75-55-8 Extremely Hazardous 1,3,4,5,6,7,8,8-Octachloro-1,3,3a,4,7,7a-hexahydro-4,7-methanoisobenzofuran Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime 26419-73-8 Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime. -

Lifetime Organophosphorous Insecticide Use Among Private Pesticide Applicators in the Agricultural Health Study
Journal of Exposure Science and Environmental Epidemiology (2012) 22, 584 -- 592 & 2012 Nature America, Inc. All rights reserved 1559-0631/12 www.nature.com/jes ORIGINAL ARTICLE Lifetime organophosphorous insecticide use among private pesticide applicators in the Agricultural Health Study Jane A. Hoppin1, Stuart Long2, David M. Umbach3, Jay H. Lubin4, Sarah E. Starks5, Fred Gerr5, Kent Thomas6, Cynthia J. Hines7, Scott Weichenthal8, Freya Kamel1, Stella Koutros9, Michael Alavanja9, Laura E. Beane Freeman9 and Dale P. Sandler1 Organophosphorous insecticides (OPs) are the most commonly used insecticides in US agriculture, but little information is available regarding specific OP use by individual farmers. We describe OP use for licensed private pesticide applicators from Iowa and North Carolina in the Agricultural Health Study (AHS) using lifetime pesticide use data from 701 randomly selected male participants collected at three time periods. Of 27 OPs studied, 20 were used by 41%. Overall, 95% had ever applied at least one OP. The median number of different OPs used was 4 (maximum ¼ 13). Malathion was the most commonly used OP (74%) followed by chlorpyrifos (54%). OP use declined over time. At the first interview (1993--1997), 68% of participants had applied OPs in the past year; by the last interview (2005--2007), only 42% had. Similarly, median annual application days of OPs declined from 13.5 to 6 days. Although OP use was common, the specific OPs used varied by state, time period, and individual. Much of the variability in OP use was associated with the choice of OP, rather than the frequency or duration of application. -

Investigation on the Behavior of Pesticides in Atmosphere
Aerosol and Air Quality Research, 11: 783–790, 2011 Copyright © Taiwan Association for Aerosol Research ISSN: 1680-8584 print / 2071-1409 online doi: 10.4209/aaqr.2010.10.0085 Investigation on the Behavior of Pesticides in Atmosphere Pasquale Avino1, Giuseppe Cinelli2, Ivan Notardonato2, Mario V. Russo2* 1 DIPIA, INAIL (ex-ISPESL), via Urbana 167, 00184 Rome, Italy 2 Faculty of Agriculture, University of Molise, via De Sanctis, Campobasso, Italy ABSTRACT Although pesticides are widely used in agriculture, they and in particular the relative residues in foodstuffs, water and atmosphere, may cause remarkable sanitary problems due to the harmful effects (carcinogenic and mutagenic effects) on the human health. In fact, their spread in waters and atmosphere can produce undesired effects on various organisms and/or water contamination. This paper shows an analytical approach based on XAD-2 adsorbent and GC analysis for evaluating the pesticide trend in atmosphere: in particular, the pesticides investigated are omethoate, dicrotofos, disulfoton, dimethoate, parathion methyl, formothion, paraoxon ethyl, malaoxon, parathion ethyl, iodofenfos and triazofos. For the analytical methodology a linearity response was obtained (r2 = 0.9988) in GC-NPD whereas the limits of detection range between 2 and 5 pg/μL in GC-NPD with a Relative Standard Deviation below 9.5. Finally, this approach has been successfully applied to real samples: the results show that dimethoate concentration decreases with increasing distance from the sampling site but it is still persistent in atmosphere after few days from the pesticide spraying. Keywords: Pesticides; XAD-2 adsorbent; GC analysis; Atmosphere; Air quality. INTRODUCTION 2009). One of the most important OP reactions is water hydrolysis. -

Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2019 Theinternational Programme on Chemical Safety (IPCS) Was Established in 1980
The WHO Recommended Classi cation of Pesticides by Hazard and Guidelines to Classi cation 2019 cation Hazard of Pesticides by and Guidelines to Classi The WHO Recommended Classi The WHO Recommended Classi cation of Pesticides by Hazard and Guidelines to Classi cation 2019 The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2019 TheInternational Programme on Chemical Safety (IPCS) was established in 1980. The overall objectives of the IPCS are to establish the scientific basis for assessment of the risk to human health and the environment from exposure to chemicals, through international peer review processes, as a prerequisite for the promotion of chemical safety, and to provide technical assistance in strengthening national capacities for the sound management of chemicals. This publication was developed in the IOMC context. The contents do not necessarily reflect the views or stated policies of individual IOMC Participating Organizations. The Inter-Organization Programme for the Sound Management of Chemicals (IOMC) was established in 1995 following recommendations made by the 1992 UN Conference on Environment and Development to strengthen cooperation and increase international coordination in the field of chemical safety. The Participating Organizations are: FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD. The purpose of the IOMC is to promote coordination of the policies and activities pursued by the Participating Organizations, jointly or separately, to achieve the sound management of chemicals in relation to human health and the environment. WHO recommended classification of pesticides by hazard and guidelines to classification, 2019 edition ISBN 978-92-4-000566-2 (electronic version) ISBN 978-92-4-000567-9 (print version) ISSN 1684-1042 © World Health Organization 2020 Some rights reserved. -

Dimethoate 400 Systemic Insecticide
POISON KEEP OUT OF REACH OF CHILDREN READ SAFETY DIRECTIONS BEFORE OPENING OR USING Adama Dimethoate 400 Systemic Insecticide ACTIVE CONSTITUENT: 400 g/L DIMETHOATE (an anti-cholinesterase compound) GROUP 1B INSECTICIDE For the control of certain insects including aphids, thrips, jassids, lucerne flea, redlegged earthmite, Queensland fruit fly, leaf hoppers and wingless grasshopper as specified in the Directions For Use table Formulation type Emulsifiable Concentrate EC adama.com CONTENTS: 5 L, 20 L, 10 L, 110 L, 200 L DIRECTIONS FOR USE RESTRAINTS DO NOT use to control pests that are resistant to organophosphorus insecticides as treatment may be ineffective. DO NOT apply to any non-food tree crop (except oil tea tree) or plantation (including Eucalyptus spp.) by air. DO NOT apply by misting or fogging equipment. DO NOT apply with airblast spray equipment unless operators are protected by engineering controls such as enclosed cabs fitted with appropriate air filters. DO NOT use open mixing/loading systems for aerial application. FIELD CROPS CROP PEST STATE RATE WHP CRITICAL COMMENTS (days) Cereals Lucerne Flea NSW, Vic, 55 - 85 mL/ha 4 weeks DO NOT harvest for 4 weeks after application. (Wheat, Tas, SA, (H) DO NOT graze or cut for stock feed for 14 day after application Barley, Oats, WA only 14 days Apply 3-5 weeks after the commencement of autumn rains or Triticale) (G) when outbreak occurs. Use the higher rate in cold weather. Redlegged Vic, Tas, SA, DO NOT spray on bare ground. Allow the crop to emerge Earth Mite WA only before application. Apply from boom spray in 50 -100 L NSW only 85 mL/ha water/ha or Aircraft in 20 - 40 L of water per hectare. -
List of Class 1 Designated Chemical Substances
List of Class 1 Designated Chemical Substances *1:CAS numbers are to be solely as references. They may be insufficient or lacking, in case there are multiple chemical substances. No. Specific Class 1 CAS No. (PRTR Chemical (*1) Name Law) Substances 1 - zinc compounds(water-soluble) 2 79-06-1 acrylamide 3 140-88-5 ethyl acrylate 4 - acrylic acid and its water-soluble salts 5 2439-35-2 2-(dimethylamino)ethyl acrylate 6 818-61-1 2-hydroxyethyl acrylate 7 141-32-2 n-butyl acrylate 8 96-33-3 methyl acrylate 9 107-13-1 acrylonitrile 10 107-02-8 acrolein 11 26628-22-8 sodium azide 12 75-07-0 acetaldehyde 13 75-05-8 acetonitrile 14 75-86-5 acetone cyanohydrin 15 83-32-9 acenaphthene 16 78-67-1 2,2'-azobisisobutyronitrile 17 90-04-0 o-anisidine 18 62-53-3 aniline 19 82-45-1 1-amino-9,10-anthraquinone 20 141-43-5 2-aminoethanol 21 1698-60-8 5-amino-4-chloro-2-phenylpyridazin-3(2H)-one; chloridazon 5-amino-1-[2,6-dichloro-4-(trifluoromethyl)phenyl]-3-cyano- 22 120068-37-3 4[(trifluoromethyl)sulfinyl]pyrazole; fipronil 23 123-30-8 p-aminophenol 24 591-27-5 m-aminophenol 4-amino-6-tert-butyl-3-methylthio-1,2,4-triazin-5(4H)-one; 25 21087-64-9 metribuzin 26 107-11-9 3-amino-1-propene 27 41394-05-2 4-amino-3-methyl-6-phenyl-1,2,4-triazin-5(4H)-one; metamitron 28 107-18-6 allyl alcohol 29 106-92-3 1-allyloxy-2,3-epoxypropane 30 - n-alkylbenzenesulfonic acid and its salts(alkyl C=10-14) 31 - antimony and its compounds 32 120-12-7 anthracene 33 1332-21-4 asbestos ○ 34 4098-71-9 3-isocyanatomethyl-3,5,5-trimethylcyclohexyl isocyanate 35 78-84-2 isobutyraldehyde -

Pesticide Resistance of Agricultural Pests in Japan
Pesticide Resistance of Agricultural Pests in Japan By TOSHIKAZU IWATA Chief, 3rd Laboratory of Insect Control Investigation, Department of Phytopathology and Entomology, National Institute of Agricultural Sciences A quarter century has passed since DDT other organophosphorus chemicals such as was firstly applied to control agricultural in methyl paration. As the result the parathion sect pests. The amount of synthesized organic resistant borer was prevented from spreading insecticides applied in fields increased rapidly by changing insecticide to be applied for the since 1952 and the rate of increase was about control. 10 per cent a year. In 1960 an evident report Control of the rice stem borer by BHC dust was made on insecticide resistance of insects, was established in about 1950, and application so 10 years have passed following the first of fine dust or granular formulation of BHC appearance of insecticide-resistant insects. to paddy fields became very popular in 1961 Today, pest species developed or suspected of or 1962. In 1964, declination of susceptibility resistance totals 11 species of insects and 6 of the borers to BHC was found in Kagawa species of mites as shown in Table 1. The Prefecture. After that, similar phenomena author reviews the circumstances of occur were reported in some other prefectures. The rence and some results of studies on major amount of BHC applied to paddy fields has instances of resistant pests. been decreased for its residue in rice plants. Consequently, BHC resistance of rice stem Rice stem borer, Chilo suppressalis borer may not become a serious problem in Walker future. Recently, declination of susceptibility of The rice stem borer is one of the most im the borer to fenitrothion is suspected in a portant pests of rice plants in Japan. -

United States Patent (19) 11 Patent Number: 5,703,064 Yokoi Et Al
US005703064A United States Patent (19) 11 Patent Number: 5,703,064 Yokoi et al. 45) Date of Patent: Dec. 30, 1997 54 PESTICIDAL COMBINATIONS FOREIGN PATENT DOCUMENTS 75 Inventors: Shinji Yokoi; Akira Nishida, both of 0 196524 10/1986 European Pat. Of.. Shiga-ken; Tokio Obata; Kouichi Golka, both of Ube, all of Japan OTHER PUBLICATIONS 73) Assignees: Sankyo Company, Limited, Tokyo; Worthing et al, The Pesticide Manual, 9th Ed. (1991), pp. Ube industries Ltd., Ube, both of 747 and 748. Japan L.C. Gaughan et al., "Pesticide interactions: effects of orga nophosphorus pesticides on the metabolism, toxicity, and 21 Appl. No.: 405,795 persistence of selected pyrethroid insecticides". Chemical Abstracts, vol. 94, No. 9, 1981, No. 59740k of Pestic. 22 Filed: Mar 16, 1995 Biochem. Physio., vol. 14, No. 1, 1980, pp. 81-85. 30 Foreign Application Priority Data I. Ishaaya et al., "Cypermethrin synergism by pyrethroid esterase inhibitors in adults of the whitefly Bemisia tabaci". Mar 16, 1994 JP Japan ............................ HE6045.405 Chemical Abstracts, vol. 107, No. 9, 1987, No. 72818y of (51) Int. Cl................. A01N 43/54; A01N 57/00 Pestic Biochem. Physiol., vol. 28, No. 2, 1987, pp. 155-162. 52 U.S. C. ......................................... 51480; 514/256 (58) Field of Search ..................................... 514/80, 256 Primary Examiner Allen J. Robinson Attorney, Agent, or Firm-Frishauf, Holtz, Goodman, 56 References Cited Langer & Chick, P.C. U.S. PATENT DOCUMENTS 57 ABSTRACT 4,374,833 2/1983 Badmin et al. ...................... 424/225 Combinations of the known compound pyrimidifen with 4,845,097 7/1989 Matsumoto et al... 514/234.2 phosphorus-containing pesticides have a synergistic pesti 4,935,516 6/1990 Ataka et al. -

US EPA, Pesticide Product Label, DIMETHOATE 400, 08/07/2013
OS 01 201S in UNITED STATES ENVIRONMENTAL PROTECTION AGENCY WASHINGTON, D.C. 20460 OFFICE OF CHEMICAL SAFETY AND POLLUTION PREVENTION AUG 7 Dr. Premjit Halarnkar Registration Manager Loveland Products, Inc. P.O. Box 1286 Greeley, CO 80632-1286 Subject: DIMETHOATE 400 EPA Registration No. 34704-207 EPA-Initiated Action Concerning Protective Eyewear Revised Label Submitted on July 19, 2013 Dear Dr. Halarnkar: The proposed amended label submitted on July 19, 2013, for this product is accepted under the provisions of the Federal Insecticide, Fungicide and Rodenticide Act (FIFRA), as amended. A stamped copy of the label is enclosed for your records. Submit two copies of final printed labeling before releasing this product for shipment under the labeling accepted via this letter. Products shipped after 18 months from the date of this Notice or the next printing of the label, whichever occurs first, must bear this revised label. If you have any questions, please call Dr. William W. Jacobs at 703-305-6406 or contact him via [email protected]. Sincerely, \jJLl_Ji Venus Eagle Product Manager 01 Insecticide-Rodenticide Branch Registration Division (7505P) Office of Pesticide Programs •z. DIMETHOATE Under the Federal Insecticide, Fungici III and Rodentlcide Act, as amended, for 4 pesticide registered under: EPA. Reg. Mn: Organophosphate Insecticide SYSTEMIC INSECTICIDE-MITICIDE ACTIVE INGREDIENT: Dimethoate (0,0-dimethyl-S-[(methylcarbamoyl) methyl] phosphorodithioate) 43.5% OTHER INGREDIENTS:* 56.5% TOTAL 100.0% This product contains petroleum distillates. (1.0 gallon contains 4.0 pounds of dimethoate) KEEP OUT OF REACH OF CHILDREN WARNING—AVISO Si listed no entiende la etiqueta, busque a alguien para que se la explique a listed en detalle. -
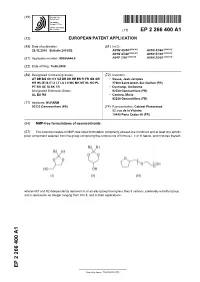
NMP-Free Formulations of Neonicotinoids
(19) & (11) EP 2 266 400 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 29.12.2010 Bulletin 2010/52 A01N 43/40 (2006.01) A01N 43/86 (2006.01) A01N 47/40 (2006.01) A01N 51/00 (2006.01) (2006.01) (2006.01) (21) Application number: 09305544.0 A01P 7/00 A01N 25/02 (22) Date of filing: 15.06.2009 (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • Gasse, Jean-Jacques HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL 27600 Saint-Aubin-Sur-Gaillon (FR) PT RO SE SI SK TR • Duchamp, Guillaume Designated Extension States: 92230 Gennevilliers (FR) AL BA RS • Cantero, Maria 92230 Gennevilliers (FR) (71) Applicant: NUFARM 92233 Gennevelliers (FR) (74) Representative: Cabinet Plasseraud 52, rue de la Victoire 75440 Paris Cedex 09 (FR) (54) NMP-free formulations of neonicotinoids (57) The invention relates to NMP-free liquid formulation comprising at least one nicotinoid and at least one aprotic polar component selected from the group comprising the compounds of formula I, II or III below, and mixtures thereof, wherein R1 and R2 independently represent H or an alkyl group having less than 5 carbons, preferably a methyl group, and n represents an integer ranging from 0 to 5, and to their applications. EP 2 266 400 A1 Printed by Jouve, 75001 PARIS (FR) EP 2 266 400 A1 Description Technical Field of the invention 5 [0001] The invention relates to novel liquid formulations of neonicotinoids and to their use for treating plants, for protecting plants from pests and/or for controlling pests infestation. -
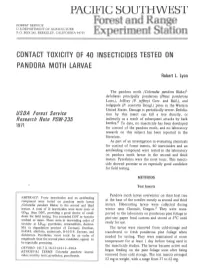
PACIFIC SOUTHWEST Forest and Range Experiment St Ation
PACIFIC SOUTHWEST Forest and Range FOREST SERVICE U. S.DEPARTMENT OF AGRICULTURE P.O. BOX 245, BERKELEY, CALIFORNIA 94701 Experiment St ation CONTACT TOXICITY OF 40 INSECTICIDES TESTED ON PANDORA MOTH LARVAE Robert L. Lyon The pandora moth (Coloradia pandora Blake)' defoliates principally ponderosa (Pinus ponderosa Laws.), Jeffrey (P. jeffreyi Grev. and Balf.), and lodgepole (P. contorta Dougl.) pines in the Western United States. Damage is periodically severe. Defolia- USDA Forest Service tion by this insect can kill a tree directly, or Research Iote PSW-235 indirectly as a result of subsequent attacks by bark beetles.* To date, no insecticide has been developed 1971 for control of the pandora moth, and no laboratory research on this subject has been reported in the literature. As part of an investigation in evaluating chemicals for control of forest insects, 40 insecticides and an antifeeding compound were tested in the laboratory on pandora moth larvae in the second and third instars. Pyrethrins were the most toxic. This insecti- cide showed promise as an especially good candidate for field testing. METHODS Test Insects Pandora moth larvae overwinter on their host tree ABSTRACT: Forty insecticides and an antifeeding compound were tested on pandora moth larvae at the base of the needles mostly as second and third (Coloradia pandora Blake) in the second and third instars. Hibernating larvae were collected during instars. A total of 21 insecticides were more toxic at winter near Chemult, O~egon.~They were trans- LDgO than DDT, providing a good choice of candi- ported to the laboratory on ponderosa pine foliage in dates for field testing.