Assessment of Coding Region Variants in Kuwaiti Population: Implications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
An Analysis About Heterogeneity Among Cancers Based on the DNA Methylation Patterns
An analysis about heterogeneity among cancers based on the DNA Methylation Patterns Yang Liu Harbin Institute of Technology Yue Gu Harbin Medical University Mu Su Harbin Institute of Technology Hui Liu Harbin Institute of Technology Shumei Zhang Harbin Medical University Yan Zhang ( [email protected] ) Harbin Institute of Technology https://orcid.org/0000-0002-5307-2484 Research article Keywords: DNA methylation, cancer, epigenetic heterogeneity, survival analysis Posted Date: July 17th, 2019 DOI: https://doi.org/10.21203/rs.2.11636/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Cancer on December 1st, 2019. See the published version at https://doi.org/10.1186/s12885-019-6455-x. Page 1/28 Abstract Background: The occurrence of cancer is usually the result of a co-effect of genetic and environmental factors. It is generally believed that the main cause of cancer is the accumulation of genetic mutations, and DNA methylation, as one of the epigenetic modications closely related to environmental factors, participates in the regulation of gene expression and cell differentiation and plays an important role in the development of cancer. Methods: This article discusses the epigenetic heterogeneity of cancer in detail. Firstly DNA methylation data of 7 cancer types were obtained from Illumina Innium HumanMethylation 450K platform of TCGA database. Diagnostic markers of each cancer were obtained by t-test and absolute difference of DNA differencial methylation analysis. Enrichment analysis of these specic markers indicated that they were involved in different biological functions. -

Brain Gene Expression in a Novel Mouse Model of Postpartum Mood Disorder
bioRxiv preprint doi: https://doi.org/10.1101/555870; this version posted March 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Brain gene expression in a novel mouse model of postpartum mood disorder Trevor Humby1,2,3, William Davies1,2,3* 1School of Psychology, Cardiff University, UK 2Neuroscience and Mental Health Research Institute, Cardiff University, UK 3Medical Research Council Centre for Neuropsychiatric Genetics and Genomics and Division of Psychological Medicine and Clinical Neurosciences, School of Medicine, Cardiff University, UK *to whom correspondence should be addressed: Dr William Davies, Cardiff University School of Psychology, Tower Building, 70, Park Place, Cardiff CF10 3AT, UK Tel:+44-(0)29-2087-0152 e-mail: [email protected] Running title: Transcriptomics of a new mood disorder model bioRxiv preprint doi: https://doi.org/10.1101/555870; this version posted March 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Abstract Introduction: Steroid sulfatase (STS) is an enzyme which cleaves sulfate groups from a variety of steroid hormones, thereby altering their activity and solubility. The expression and activity of STS is increased in female mammalian tissues (including brain) during late pregnancy and into the postpartum period. STS-deficient human and mouse mothers (as a consequence of genetic mutation or acute pharmacological manipulation) show evidence for elevated psychopathology and abnormal behaviour respectively in the postpartum period. -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e . -
An Analysis About Heterogeneity Among Cancers Based on the DNA Methylation Patterns Yang Liu1, Yue Gu2,Musu1, Hui Liu2, Shumei Zhang3* and Yan Zhang1*
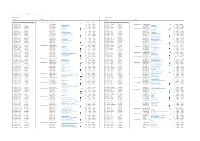
Liu et al. BMC Cancer (2019) 19:1259 https://doi.org/10.1186/s12885-019-6455-x RESEARCH ARTICLE Open Access An analysis about heterogeneity among cancers based on the DNA methylation patterns Yang Liu1, Yue Gu2,MuSu1, Hui Liu2, Shumei Zhang3* and Yan Zhang1* Abstract Background: It is generally believed that DNA methylation, as one of the most important epigenetic modifications, participates in the regulation of gene expression and plays an important role in the development of cancer, and there exits epigenetic heterogeneity among cancers. Therefore, this study tried to screen for reliable prognostic markers for different cancers, providing further explanation for the heterogeneity of cancers, and more targets for clinical transformation studies of cancer from epigenetic perspective. Methods: This article discusses the epigenetic heterogeneity of cancer in detail. Firstly, DNA methylation data of seven cancer types were obtained from Illumina Infinium HumanMethylation 450 K platform of TCGA database. Then, differential methylation analysis was performed in the promotor region. Secondly, pivotal gene markers were obtained by constructing the DNA methylation correlation network and the gene interaction network in the KEGG pathway, and 317 marker genes obtained from two networks were integrated as candidate markers for the prognosis model. Finally, we used the univariate and multivariate COX regression models to select specific independent prognostic markers for each cancer, and studied the risk factor of these genes by doing survival analysis. Results: First, the cancer type-specific gene markers were obtained by differential methylation analysis and they were found to be involved in different biological functions by enrichment analysis. Moreover, specific and common diagnostic markers for each type of cancer was sorted out and Kaplan-Meier survival analysis showed that there was significant difference in survival between the two risk groups. -
Explorations in Olfactory Receptor Structure and Function by Jianghai
Explorations in Olfactory Receptor Structure and Function by Jianghai Ho Department of Neurobiology Duke University Date:_______________________ Approved: ___________________________ Hiroaki Matsunami, Supervisor ___________________________ Jorg Grandl, Chair ___________________________ Marc Caron ___________________________ Sid Simon ___________________________ [Committee Member Name] Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Neurobiology in the Graduate School of Duke University 2014 ABSTRACT Explorations in Olfactory Receptor Structure and Function by Jianghai Ho Department of Neurobiology Duke University Date:_______________________ Approved: ___________________________ Hiroaki Matsunami, Supervisor ___________________________ Jorg Grandl, Chair ___________________________ Marc Caron ___________________________ Sid Simon ___________________________ [Committee Member Name] An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Neurobiology in the Graduate School of Duke University 2014 Copyright by Jianghai Ho 2014 Abstract Olfaction is one of the most primitive of our senses, and the olfactory receptors that mediate this very important chemical sense comprise the largest family of genes in the mammalian genome. It is therefore surprising that we understand so little of how olfactory receptors work. In particular we have a poor idea of what chemicals are detected by most of the olfactory receptors in the genome, and for those receptors which we have paired with ligands, we know relatively little about how the structure of these ligands can either activate or inhibit the activation of these receptors. Furthermore the large repertoire of olfactory receptors, which belong to the G protein coupled receptor (GPCR) superfamily, can serve as a model to contribute to our broader understanding of GPCR-ligand binding, especially since GPCRs are important pharmaceutical targets. -

Downloaded 2021-09-30T18:44:19Z
Provided by the author(s) and University College Dublin Library in accordance with publisher policies. Please cite the published version when available. Title A novel approach of homozygous haplotype sharing identifies candidate genes in autism spectrum disorder Authors(s) Casey, Jillian; Magalhaes, Tiago; Conroy, Judith M.; Regan, Regina; Shah, Naisha; Shields, Denis C.; Green, Andrew; Ennis, Sean; et al. Publication date 2012-04 Publication information Human Genetics, 131 (4): 565-579 Publisher Springer Item record/more information http://hdl.handle.net/10197/6163 Publisher's statement The final publication is available at www.springerlink.com Publisher's version (DOI) 10.1007/s00439-011-1094-6 Downloaded 2021-09-30T18:44:19Z The UCD community has made this article openly available. Please share how this access benefits you. Your story matters! (@ucd_oa) © Some rights reserved. For more information, please see the item record link above. A novel approach of homozygous haplotype sharing identifies candidate genes in autism spectrum disorder Jillian P. Casey1, Tiago Magalhaes2,3,4, Judith M. Conroy1, Regina Regan1, Naisha Shah1, Richard Anney5, Denis C. Shields1, Brett S. Abrahams6, Joana Almeida7, Elena Bacchelli8, Anthony J. Bailey9 , Gillian Baird10, Agatino Battaglia11, Tom Berney12, Nadia Bolshakova5, Patrick F. Bolton13, Thomas Bourgeron14, Sean Brennan5, Phil Cali15, Catarina Correia2,3,4, Christina Corsello16, Marc Coutanche63, Geraldine Dawson17,18, Maretha de Jonge19, Richard Delorme20, Eftichia Duketis21, Frederico Duque7, Annette Estes22, Penny Farrar23, Bridget A. Fernandez24, Susan E. Folstein25, Suzanne Foley63, Eric Fombonne26, Christine M. Freitag21, John Gilbert27, Christopher Gillberg28, Joseph T. Glessner29, Jonathan Green30, Stephen J. Guter15, Hakon Hakonarson29, 31, Richard Holt23, Gillian Hughes5, Vanessa Hus16, Roberta Igliozzi11, Cecilia Kim29, Sabine M. -

Characterization of the Genomic Features and Expressed Fusion Genes In
1 SUPPLEMENTARY INFORMATION (ONLINE SUPPORTING INFORMATION) Characterization of the genomic features and expressed fusion genes in micropapillary carcinomas of the breast Natrajan et al. Supplementary Methods Supplementary Figures S1-S6 Supplementary Tables S1-S7 2 SUPPLEMENTARY METHODS Tumor samples Two cohorts of micropapillary carcinomas (MPCs) were analyzed; the first cohort comprised 16 consecutive formalin fixed paraffin embedded (FFPE) MPCs, 11 pure and 5 mixed, which were retrieved from the authors' institutions (Table 1), and a second, validation cohort comprised 14 additional consecutive FFPE MPCs, retrieved from Molinette Hospital, Turin, Italy. Frozen samples were available from five out of the 16 cases from the first cohort of MPCs. As a comparator for the results of the Sequenom mutation profiling, a cohort of 16 consecutive IC-NSTs matched to the first cohort of 16 MPCs according to ER and HER2 status and histological grade were retrieved from a series of breast cancers previously analyzed by aCGH[1]. In addition, 14 IC-NSTs matched according to grade, and ER and HER2 status to tumors from the second cohort of 14 MPCs, and 48 grade 3 IC-NSTs were retrieved from Hospital La Paz, Madrid, Spain[1] (Supplementary Table S1). Power calculation For power calculations, we have assumed that if MPCs were driven by a recurrent fusion gene in a way akin to secretory carcinomas (which harbor the ETV6-NTRK3 fusion gene in >95% of cases[2-4]) or adenoid cystic carcinomas of the breast (which harbor the MYB-NFIB fusion gene in >90% of cases[5]), a ‘pathognomonic’ driver event would be present in at least ≥70% of cases (an estimate that is conservative). -

Supplementary Methods
doi: 10.1038/nature06162 SUPPLEMENTARY INFORMATION Supplementary Methods Cloning of human odorant receptors 423 human odorant receptors were cloned with sequence information from The Olfactory Receptor Database (http://senselab.med.yale.edu/senselab/ORDB/default.asp). Of these, 335 were predicted to encode functional receptors, 45 were predicted to encode pseudogenes, 29 were putative variant pairs of the same genes, and 14 were duplicates. We adopted the nomenclature proposed by Doron Lancet 1. OR7D4 and the six intact odorant receptor genes in the OR7D4 gene cluster (OR1M1, OR7G2, OR7G1, OR7G3, OR7D2, and OR7E24) were used for functional analyses. SNPs in these odorant receptors were identified from the NCBI dbSNP database (http://www.ncbi.nlm.nih.gov/projects/SNP) or through genotyping. OR7D4 single nucleotide variants were generated by cloning the reference sequence from a subject or by inducing polymorphic SNPs by site-directed mutagenesis using overlap extension PCR. Single nucleotide and frameshift variants for the six intact odorant receptors in the same gene cluster as OR7D4 were generated by cloning the respective genes from the genomic DNA of each subject. The chimpanzee OR7D4 orthologue was amplified from chimpanzee genomic DNA (Coriell Cell Repositories). Odorant receptors that contain the first 20 amino acids of human rhodopsin tag 2 in pCI (Promega) were expressed in the Hana3A cell line along with a short form of mRTP1 called RTP1S, (M37 to the C-terminal end), which enhances functional expression of the odorant receptors 3. For experiments with untagged odorant receptors, OR7D4 RT and S84N variants without the Rho tag were cloned into pCI. -

Research/0018.1
http://genomebiology.com/2001/2/6/research/0018.1 Research The human olfactory receptor repertoire comment Sergey Zozulya, ernando Echeverri and Trieu Nguyen Address: Senomyx Inc., 11099 North Torrey Pines Road, La Jolla, CA 92037, USA. Correspondence: Sergey Zozulya. E-mail: [email protected] reviews Published: 1 June 2001 Received: 8 March 2001 Revised: 12 April 2001 Genome Biology 2001, 2(6):research0018.1–0018.12 Accepted: 18 April 2001 The electronic version of this article is the complete one and can be found online at http://genomebiology.com/2001/2/6/research/0018 © 2001 Zozulya et al., licensee BioMed Central Ltd (Print ISSN 1465-6906; Online ISSN 1465-6914) reports Abstract Background: The mammalian olfactory apparatus is able to recognize and distinguish thousands of structurally diverse volatile chemicals. This chemosensory function is mediated by a very large family of seven-transmembrane olfactory (odorant) receptors encoded by approximately 1,000 genes, the majority of which are believed to be pseudogenes in humans. deposited research Results: The strategy of our sequence database mining for full-length, functional candidate odorant receptor genes was based on the high overall sequence similarity and presence of a number of conserved sequence motifs in all known mammalian odorant receptors as well as the absence of introns in their coding sequences. We report here the identification and physical cloning of 347 putative human full-length odorant receptor genes. Comparative sequence analysis of the predicted gene products allowed us to identify and define a number of consensus sequence motifs and structural features of this vast family of receptors. -

Ectopic Odorant Receptor Responding to Flavor Compounds: Versatile Roles in Health and Disease
pharmaceutics Review Ectopic Odorant Receptor Responding to Flavor Compounds: Versatile Roles in Health and Disease Tao Tong 1,* , Yanan Wang 1, Seong-Gook Kang 2 and Kunlun Huang 1,3,4,* 1 Beijing Advanced Innovation Center for Food Nutrition and Human Health, College of Food Science and Nutritional Engineering, China Agricultural University, Beijing 100083, China; [email protected] 2 Department of Food Engineering, Mokpo National University, Muangun 58554, Korea; [email protected] 3 Key Laboratory of Safety Assessment of Genetically Modified Organism (Food Safety), Ministry of Agriculture, Beijing 100083, China 4 Beijing Laboratory for Food Quality and Safety, Beijing 100083, China * Correspondence: [email protected] (T.T.); [email protected] (K.H.); Tel.: +86-10-6273-7244 (T.T.); +86-10-6273-7786 (K.H.) Abstract: Prompted by the ground-breaking discovery of the rodent odorant receptor (OR) gene family within the olfactory epithelium nearly 30 years ago, followed by that of OR genes in cells of the mammalian germ line, and potentiated by the identification of ORs throughout the body, our appreciation for ORs as general chemoreceptors responding to odorant compounds in the regulation of physiological or pathophysiological processes continues to expand. Ectopic ORs are now activated by a diversity of flavor compounds and are involved in diverse physiological phenomena varying from adipogenesis to myogenesis to hepatic lipid accumulation to serotonin secretion. In this review, we outline the key biological functions of the ectopic ORs responding to flavor compounds and the underlying molecular mechanisms. We also discuss research opportunities for utilizing ectopic ORs as therapeutic strategies in the treatment of human disease as well as challenges to be overcome in the Citation: Tong, T.; Wang, Y.; Kang, future. -
Lupus Nephritis Supp Table 7
Supplementary Table 7 : Transcripts and DAVID pathways correlating with expression of CD3 in lupus kidney biopsies Positive correlation Negative correlation Transcripts Pathways Transcripts Pathways Identifier Gene Symbol Correlation coefficient with CD3 Annotation Cluster 1 Enrichment Score: 11.22 Count P_Value Benjamini Identifier Gene Symbol Correlation coefficient with CD3 ILMN_2325837 CD3D 1 SP_PIR_KEYWORDS ribosome 42 5.40E-21 1.20E-18 ILMN_1726667 LOC728758 -0.40000032 Annotation Cluster 1 Enrichment Score: 8.3 Count P_Value Benjamini ILMN_2061043 CD48 0.905183649 GOTERM_BP_FAT translational elongation 49 2.00E-18 8.60E-15 ILMN_1767032 DDI1 -0.400066325 SP_PIR_KEYWORDS oxidoreductase 98 1.10E-11 3.90E-09 ILMN_2261416 CD3D 0.880984568 GOTERM_CC_FAT cytosolic ribosome 42 3.50E-17 2.30E-14 ILMN_3307863 TAOK3 -0.400088253 GOTERM_BP_FAT oxidation reduction 105 3.70E-10 1.40E-06 ILMN_1886655 TCRVB 0.875380574 SP_PIR_KEYWORDS protein biosynthesis 64 1.10E-16 1.00E-14 ILMN_1840934 AJ420430 -0.400098378 GOTERM_MF_FAT electron carrier activity 40 3.10E-05 5.90E-03 ILMN_1659800 BCL11A 0.861258356 KEGG_PATHWAY Ribosome 44 6.90E-15 1.10E-12 ILMN_3235584 TRIM66 -0.400113232 Annotation Cluster 2 Enrichment Score: 7.1 Count P_Value Benjamini ILMN_2098126 CCL5 0.853134526 GOTERM_CC_FAT cytosolic part 55 8.50E-14 1.80E-11 ILMN_2145760 YIPF4 -0.400116748 SP_PIR_KEYWORDS mitochondrion 143 3.20E-16 2.30E-13 ILMN_1716651 RUNX2 0.839003672 GOTERM_CC_FAT ribosomal subunit 48 8.70E-13 1.40E-10 ILMN_2146648 PRB3 -0.400169733 GOTERM_CC_FAT mitochondrion 176 -

Seeing Cells Smell: Dynamic Optical Measurements of Ca2+ and Camp Signaling from Olfactory Receptors Transiently Expressed in HEK293TN Cells
bioRxiv preprint doi: https://doi.org/10.1101/771261; this version posted September 16, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Seeing cells smell: Dynamic optical measurements of Ca2+ and cAMP signaling from Olfactory Receptors transiently expressed in HEK293TN cells A Pietraszewska-Bogiel1, L van Weeren1, J Goedhart1* 1 Section of Molecular Cytology and van Leeuwenhoek Centre for Advanced Microscopy, Swammerdam Institute for Life Sciences, University of Amsterdam, P.O. box 94215, 1090 GE, Amsterdam, The Netherlands *Corresponding author: [email protected] ABSTRACT Olfactory receptors (ORs) constitute the largest family of G-protein coupled receptors. They are responsible for the perception of odor (olfaction) and also play important roles in other biological processes, including regulation of cell proliferation. Their increasing diagnostic and therapeutic potential, especially for cancer research, requests the ongoing development of methodologies that would allow their robust functional expression in non- olfactory cells, and dynamic analysis of their signaling pathways. To enable realtime detection of OR activity, we use single cell imaging with genetically encoded fluorescent biosensors, Yellow Cameleon or EPAC, which are routinely used for kinetic measurements of Ca2+ or cAMP signaling downstream of various G-protein coupled receptors. We demonstrate that the co-expression of Lucy-Rho tagged variants of ORs together with an accessory protein, RTP1s, in HEK293TN cells is sufficient to detect the activity of a panel of ORs. Using this methodology, we were able to detect both Ca2+ and cAMP signaling downstream of twelve ORs within 2 minutes from the application of odorant.