A Regional Model for Projecting COVID-19 in Northern Mindanao, Philippines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Case Study of Metro Manila
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Manasan, Rosario G.; Mercado, Ruben G. Working Paper Governance and Urban Development: Case Study of Metro Manila PIDS Discussion Paper Series, No. 1999-03 Provided in Cooperation with: Philippine Institute for Development Studies (PIDS), Philippines Suggested Citation: Manasan, Rosario G.; Mercado, Ruben G. (1999) : Governance and Urban Development: Case Study of Metro Manila, PIDS Discussion Paper Series, No. 1999-03, Philippine Institute for Development Studies (PIDS), Makati City This Version is available at: http://hdl.handle.net/10419/187389 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von diesen Nutzungsbedingungen die in der dort Content Licence (especially Creative Commons Licences), you genannten Lizenz gewährten Nutzungsrechte. may exercise further usage rights as specified in the indicated licence. www.econstor.eu Philippine Institute for Development Studies Governance and Urban Development: Case Study of Metro Manila Rosario G. -

Lanao Del Norte – Homosexual – Dimaporo Family – Moro Islamic Liberation Front (MILF)
Refugee Review Tribunal AUSTRALIA RRT RESEARCH RESPONSE Research Response Number: PHL33460 Country: Philippines Date: 2 July 2008 Keywords: Philippines – Manila – Lanao Del Norte – Homosexual – Dimaporo family – Moro Islamic Liberation Front (MILF) This response was prepared by the Research & Information Services Section of the Refugee Review Tribunal (RRT) after researching publicly accessible information currently available to the RRT within time constraints. This response is not, and does not purport to be, conclusive as to the merit of any particular claim to refugee status or asylum. This research response may not, under any circumstance, be cited in a decision or any other document. Anyone wishing to use this information may only cite the primary source material contained herein. Questions 1. Please provide references to any recent, reliable overviews on the treatment of homosexual men in the Philippines, in particular Manila. 2. Do any reports mention the situation for homosexual men in Lanao del Norte? 3. Are there any reports or references to the treatment of homosexual Muslim men in the Philippines (Lanao del Norte or Manila, in particular)? 4. Do any reports refer to Maranao attitudes to homosexuals? 5. The Dimaporo family have a profile as Muslims and community leaders, particularly in Mindanao. Do reports suggest that the family’s profile places expectations on all family members? 6. Are there public references to the Dimaporo’s having a political, property or other profile in Manila? 7. Is the Dimaporo family known to harm political opponents in areas outside Mindanao? 8. Do the Moro Islamic Liberation Front (MILF) recruit actively in and around Iligan City and/or Manila? Is there any information regarding their attitudes to homosexuals? 9. -

Part Ii Metro Manila and Its 200Km Radius Sphere
PART II METRO MANILA AND ITS 200KM RADIUS SPHERE CHAPTER 7 GENERAL PROFILE OF THE STUDY AREA CHAPTER 7 GENERAL PROFILE OF THE STUDY AREA 7.1 PHYSICAL PROFILE The area defined by a sphere of 200 km radius from Metro Manila is bordered on the northern part by portions of Region I and II, and for its greater part, by Region III. Region III, also known as the reconfigured Central Luzon Region due to the inclusion of the province of Aurora, has the largest contiguous lowland area in the country. Its total land area of 1.8 million hectares is 6.1 percent of the total land area in the country. Of all the regions in the country, it is closest to Metro Manila. The southern part of the sphere is bound by the provinces of Cavite, Laguna, Batangas, Rizal, and Quezon, all of which comprise Region IV-A, also known as CALABARZON. 7.1.1 Geomorphological Units The prevailing landforms in Central Luzon can be described as a large basin surrounded by mountain ranges on three sides. On its northern boundary, the Caraballo and Sierra Madre mountain ranges separate it from the provinces of Pangasinan and Nueva Vizcaya. In the eastern section, the Sierra Madre mountain range traverses the length of Aurora, Nueva Ecija and Bulacan. The Zambales mountains separates the central plains from the urban areas of Zambales at the western side. The region’s major drainage networks discharge to Lingayen Gulf in the northwest, Manila Bay in the south, the Pacific Ocean in the east, and the China Sea in the west. -

4. Resources, Security and Livelihood
Violent Conflicts and Displacement in Central Mindanao 4. RESOURCES, SECURITY AND LIVELIHOOD This section examines households’ perceptions of their surrounding environment (e.g. security). It looks at their resources or capital (social, natural, economic) available to households, as well as how those resources were being used to shape livelihood strategies and livelihood outcomes such as food security. The results give insights into the complex interaction between, on the one hand, displacement and settlement options, and, on the other hand, access to basic needs, services and livelihood strategies. Services and Social Relations Access to Services Across the study strata, about one-third of the households ranked their access to services negatively, including access to education (22%), access to (35%) and quality of (32%) health care, and access to roads (37%). Respondents in Maguindanao ranked on average all services more negatively than any other strata. Disaggregated by settlement status, respondents who were displaced at the time of the survey were more likely to rank services negatively compared to others, with the exception of access to roads. Nearly the same percentage of households who were displaced at the time of survey and those returned home found the road to be bad of very bad (47% and 55%, respectively). Figure 11: Ranking of services (% bad - very bad) Two-thirds (67%) of the sampled households had children aged 6-12 years, and among them nearly all had children enrolled in primary school (97%). However, 36 percent of the households reported that their school-enrolled children missed school for at least a week within the 6 months prior to the survey. -

Mindanao-Pricelist-3Rd-Qtr-2020.Pdf
BANK OF COMMERCE ROPA PRICELIST - MINDANAO As of 3RD QTR, 2020 AREA INDICATIVE PROPERTY DESCRIPTION PROPERTY LOCATION TCT / CCT NO. STATUS (SQM) PRICE REGION IX - WESTERN MINDANAO ZAMBOANGA DEL SUR LAND WITH 1-STOREY LOT 1 BLK 3, JOHNSTON ST., BRGY. SAN JOSE GUSU (BRGY. BALIWASAN), T-223,208 820.00 5,063,000.00 RESIDENTIAL & OFFICE BLDG. ZAMBOANGA CITY, ZAMBOANGA DE SUR LOT 513, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA DEL AGRICULTURAL LOT T-217,923 71,424.00 7,143,000.00 SUR LOT 514-B, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA AGRICULTURAL LOT T-217,924 12,997.00 1,300,000.00 DEL SUR LOT 509-B, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA AGRICULTURAL LOT T-217,925 20,854.00 2,086,000.00 DEL SUR LOT 512, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA DEL AGRICULTURAL LOT T-217,926 11,308.00 1,131,000.00 SUR LOT 510, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA DEL AGRICULTURAL LOT T-217,927 4,690.00 469,000.00 SUR LOT 511, BRGYS. LA PAZ AND PAMUCUTAN, ZAMBOANGA CITY, ZAMBOANGA DEL AGRICULTURAL LOT T-217,928 17,008.00 1,701,000.00 SUR BLK 8, COUNTRY HOMES SUBD., BRGY. AYALA, ZAMBOANGA CITY (SITE IV), RESIDENTIAL VACANT LOT T-217,929 1,703.00 1,022,000.00 ZAMBOANGA DEL SUR BLK 9, COUNTRY HOMES SUBD., BRGY. AYALA, ZAMBOANGA CITY (SITE IV), RESIDENTIAL VACANT LOT T-217,930 1,258.00 755,000.00 ZAMBOANGA DEL SUR BLK 11, COUNTRY HOMES SUBD., BRGY. -

Philippines - Complex Emergency Fact Sheet #3, Fiscal Year (Fy) 2018 June 29, 2018
PHILIPPINES - COMPLEX EMERGENCY FACT SHEET #3, FISCAL YEAR (FY) 2018 JUNE 29, 2018 NUMBERS AT USAID/OFDA1 FUNDING HIGHLIGHTS A GLANCE BY SECTOR IN FY 2017–2018 Armed clashes in June displace more 2% 8% than 14,000 people 214,350 10% 33% USAID partners provide emergency Estimated Number of food, shelter, and WASH assistance People Who Remain Displaced by Conflict in 23% USAID/OFDA contributes additional Marawi $3 million to support conflict-affected OCHA – May 2018 24% IDPs and returnees Economic Recovery & Market Systems (33%) Shelter & Settlements (24%) 208,845 Water, Sanitation, & Hygiene (23%) HUMANITARIAN FUNDING Logistics Support & Relief Commodities (10%) FOR THE PHILIPPINES RESPONSE IN Estimated Number of Protection (8%) FY 2017–2018 People Returned to Humanitarian Coordination & Information Management (2%) Marawi and Surrounding USAID/OFDA $9,500,000 Areas OCHA – May 2018 USAID/FFP $2,000,000 USAID/FFP2 FUNDING BY MODALITY IN FY 2017–2018 100% $11,500,000 45 Local & Regional Procurement (100%) Government-Designated Evacuation Centers Sheltering IDPs KEY DEVELOPMENTS DSWD – April 2018 Internally displaced person (IDP) returns to areas of origin continue, following conflict between the Government of the Philippines (GPH) and armed groups that displaced more than 350,000 people from May–October 2017, according to the UN. More than 127,300 208,800 people had returned to areas of origin in Marawi—the capital city of Lanao del Estimated Number of Sur Province in the Philippines’ Autonomous Region in Muslim Mindanao—and IDPs From Heavily- surrounding areas as of May 30, the UN reports. Damaged Areas of Marawi Off-Limits for Mid-June clashes between the GPH and armed groups in Lanao del Sur’s Tubaran Returns municipality displaced nearly 14,900 people, according to the GPH Department of Social GPH – 2018 Welfare and Development. -

Volume Xxiii
ANTHROPOLOGICAL PAPERS OF THE AMERICAN MUSEUM OF NATURAL HISTORY VOLUME XXIII NEW YORK PUBLISHED BY ORDER OF THE TRUSTEES 1925 Editor CLARK WISSLER FOREWORD Louis ROBERT SULLIVAN Since this volume is largely the work of the late Louis Robert Sulli- van, a biographical sketch of this able anthropologist, will seem a fitting foreword. Louis Robert Sullivan was born at Houlton, Maine, May 21, 1892. He was educated in the public schools of Houlton and was graduated from Bates College, Lewiston, Maine, in 1914. During the following academic year he taught in a high school and on November 24, 1915, he married Bessie Pearl Pathers of Lewiston, Maine. He entered Brown University as a graduate student and was assistant in zoology under Professor H. E. Walters, and in 1916 received the degree of master of arts. From Brown University Mr. Sullivan came to the American Mu- seum of Natural History, as assistant in physical anthropology, and during the first years of his connection with the Museum he laid the foundations for his future work in human biology, by training in general anatomy with Doctor William K. Gregory and Professor George S. Huntington and in general anthropology with Professor Franz Boas. From the very beginning, he showed an aptitude for research and he had not been long at the Museum ere he had published several important papers. These activities were interrupted by our entrance into the World War. Mr. Sullivan was appointed a First Lieutenant in the Section of Anthropology, Surgeon-General's Office in 1918, and while on duty at headquarters asisted in the compilation of the reports on Defects found in Drafted Men and Army Anthropology. -
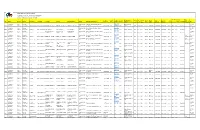
NORTHERN MINDANAO Directory of Mines and Quarries
MINES AND GEOSCIENCES BUREAU REGIONAL OFFICE NO.: X- NORTHERN MINDANAO Directory of Mines and Quarries - CY 2020 Other Plant Locations Status Mine Site Mine Mine Site E- Head Office Head Office Head Office E- Head Office Mine Site Mailing Type of Permit Date Date of Area municipality, Non- Telephon Site Fax mail barangay Year Region Mineral Province Municipality Commodity Contractor Operator Managing Official Position Head Office Mailing Address Telephone No. Fax No. mail Address Website (hectares) province Producing TIN Address e No. No. Address Permit Number Approved Expiration Producing donjieanim 10-Northern Non- Misamis Proprietor/Man Poblacion, Sapang Dalaga, Misamis as@yahoo Dioyo, Sapang 191-223- 2020 Mindanao Metallic Occidental Sapang Dalaga Sand and Gravel ANIMAS, EMILOU M. ANIMAS, EMILOU M. ANIMAS, EMILOU M. ager Occidental 9654955493 N/A .com N/A Dalaga N/A N/A N/A CSAG RP-07-19 11/10/2019 10/10/2020 1.00 N/A N/A Producing 205 10-Northern Non- Misamis Proprietor/Man South Western, Calamba, Misamis ljcyap7@g 432-503- 2020 Mindanao Metallic Occidental Calamba Sand and Gravel YAP, LORNA T. YAP, LORNA T. YAP, LORNA T. ager Occidental 9466875752 N/A mail.com N/A Sulipat, Calamba N/A N/A N/A CSAG RP-18-19 04/02/2020 03/02/2021 1.9524 N/A N/A Producing 363 maconsuel 10-Northern Non- Misamis ROGELIO, MARIA ROGELIO, MA. ROGELIO, MA. Proprietor/Man Northern Poblacion, Calamba, Misamis orogelio@ 325-550- 2020 Mindanao Metallic Occidental Calamba Sand and Gravel CONSUELO A. CONSUELO A. CONSUELO ager Occidental 9464997271 N/A gmail.com N/A Solinog, Calamba N/A N/A N/A CSAG RP-03-20 24/06/2020 23/06/2021 1.094 N/A N/A Producing 921 noel_pagu 10-Northern Non- Misamis Proprietor/Man Southern Poblacion, Plaridel, Misamis e@yahoo. -

RA No. 11565: First Misamis Oriental General Hospital
•I No. 6753 be char^ed against the current year’s appropriations of the Medina Extension Hospital, the amount of Nine hundred ^spuHIit of fIjB ^ijilipjrincs million pesos (P900,000,000.00) is hereby appropriated for the implementation of this Act which shall be included and funded Congress nfflfe pijtltgptnes ^der the 2022 General Appropriations Act under the Health Facilities Enhancement Program (HFEP) of the DOH. Therea^r, such sums as may be necessary for its continued Jigljfgcnflj Soogreas operation shall be included in the annual General Appropriations Act. i3ecoHh ^gular<^£ssdn« Sec. 3. The Secretary of Health shall prepare and issue e necessary rules andregulations for the effective implementation ot this Act consistent with the hospital development plan. Begun and held in Metro Manila, on Monday, the twenty-seventh Sec. 4. This Act shall take effect fifteen (15) days aft/i day of July, two thousand twenty. Its pubhcation in the Official Gazette or in a newspaper of general circulation. proved. [Republic act no. 11565] A.N ACT CONVERTING THE MEDINA EXTENSION VICENTE C. om LORD ALL. Q. VELASCO HOSPITAL IN THE MUNICIPALITY OF MEDINA, President of i enate 2 House PROVINCE OF MISAMIS ORIENTAL INTO A of Representatives GENERAL HOSPITAL TO BE KNOWN AS THE FIRST MISAMIS ORIENTAL GENERAL HOSPITAL This Act which originated in the House of Representatives AND APPROPRIATING FUNDS THEREFOR was p^sed by the House of Representatives on June 3, 2020 amended by the Senate of the Philippines on May 31,2021, and Be it enacted by the Senate and House of Representatives of the which amendment was concurred in by the House of Philippines in Congress assembled: Representatives on Jime 2,2021. -

FAO Philippines Newsletter 2015. Issue 3
WELCOME Contents Asia-Pacific region achieves elcome to the third issue of the capacities of local governments and MDG hunger target, but FAO Philippines newsletter. My farmers in community-based disaster millions still chronically W team and I are pleased to update risk reduction and management. 3 hungry you on the status of our programmes and the activities we have undertaken in DRR is also integral to the three new the second quarter of 2015. livelihood restoration projects that Three new projects launched FAO recently launched in central and to restore agricultural We continue to maintain our western Mindanao. Through these livelihoods and food security engagement in Typhoon Haiyan- new projects, more than 15 000 farmer 4 in Mindanao affected regions as we approach the and fisher-households will be able final phase of our recovery efforts. to resume their farming and fishing Eighteen of our 22 projects have been activities and gain knowledge on DRR. IPC chronic food security completed, with substantial impacts Women and combatants of the Moro analysis of Mindanao in restoring agriculture and fisheries- Islamic Liberation Front who are likely 6 based livelihoods and improving the to be decommissioned as part of the capability of beneficiary communities to peace process will also benefit from prepare for and cope with future shocks FAO’s assistance. and emergencies. We aim to complete Building more resilient our activities by year-end, bringing the I am proud to highlight that all of farming communities after total number of beneficiaries to at least these accomplishments and new 8 Typhoon Haiyan 154 000 households that will be well on opportunities to contribute to their way to longer-term recovery. -

MAKING the LINK in the PHILIPPINES Population, Health, and the Environment
MAKING THE LINK IN THE PHILIPPINES Population, Health, and the Environment The interconnected problems related to population, are also disappearing as a result of the loss of the country’s health, and the environment are among the Philippines’ forests and the destruction of its coral reefs. Although greatest challenges in achieving national development gross national income per capita is higher than the aver- goals. Although the Philippines has abundant natural age in the region, around one-quarter of Philippine fami- resources, these resources are compromised by a number lies live below the poverty threshold, reflecting broad social of factors, including population pressures and poverty. The inequity and other social challenges. result: Public health, well-being and sustainable develop- This wallchart provides information and data on crit- ment are at risk. Cities are becoming more crowded and ical population, health, and environmental issues in the polluted, and the reliability of food and water supplies is Philippines. Examining these data, understanding their more uncertain than a generation ago. The productivity of interactions, and designing strategies that take into the country’s agricultural lands and fisheries is declining account these relationships can help to improve people’s as these areas become increasingly degraded and pushed lives while preserving the natural resource base that pro- beyond their production capacity. Plant and animal species vides for their livelihood and health. Population Reference Bureau 1875 Connecticut Ave., NW, Suite 520 Washington, DC 20009 USA Mangroves Help Sustain Human Vulnerability Coastal Communities to Natural Hazards Comprising more than 7,000 islands, the Philippines has an extensive coastline that is a is Increasing critical environmental and economic resource for the nation. -

Microfinance and Financial Institutions in Bukidnon
Microfinance and Financial Institutions in Bukidnon Author: Beethoven Morales Research Institute for Mindanao Culture (RIMCU) BASIS CRSP This posting is provided by the BASIS CRSP Management Entity Department of Agricultural and Applied Economics, University of Wisconsin-Madison Tel: (608) 262-5538 Email: basis [email protected] http://www.basis.wisc.edu October 2004 Beethoven Morales Research Institute for Mindanao Culture [email protected] BASIS CRSP outputs posted on this website have been formatted to conform with other postings but the contents have not been edited. This output was made possible in part through support provided by the US Agency for International Development (USAID), under the terms of Grant No. LAG-A-00-96-90016-00, and by funding support from the BASIS Collaborative Research Support Program and its management entity, the Department of Agricultural and Applied Economics, University of Wisconsin-Madison, USA. All views, interpretations, recommendations, and conclusions expressed in this paper are those of the author(s) and not necessarily those of the supporting or cooperating organizations. Copyright © by author. All rights reserved. Readers may make verbatim copies of this document for noncommercial purposes by any means, provided that this copyright notice appears on all such copies. ii Microfinance and Financial Institutions in Bukidnon Beethoven C. Morales Research Institute for Mindanao Culture, Xavier University Cagayan de Oro City, Philippines August 2004 1. I NTRODUCTION This report looks at the relationship between microfinance and financial institutions in Bukidnon within the context of the national and local (province) poverty conditions in the Philippines. The report examines government involvement in the provision of credit to low-income groups, and the importance and contributions of nongovernment microfinance providers.