Nurses Information Pack 2018.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How Irish Radio Made Strides for Women's Rights
Salve Regina University Digital Commons @ Salve Regina Pell Scholars and Senior Theses Salve's Dissertations and Theses 5-11-2020 Her Voice on Air: How Irish Radio Made Strides for Women's Rights Emilie R. Hines Follow this and additional works at: https://digitalcommons.salve.edu/pell_theses Part of the English Language and Literature Commons, European History Commons, Film and Media Studies Commons, Women's History Commons, and the Women's Studies Commons Her Voice on Air: How Irish Radio Made Strides for Women’s Rights By Emilie Hines Prepared for Dr. Madeleine Esch Department of English, Communications and Media Salve Regina University May 11, 2020 Hines 1 Her Voice on Air: How Irish Radio Made Strides for Women’s Rights ABSTRACT: Radio is the voice of the people; this is no less true in Ireland, a nation that prefers talk radio and phone-ins. These formats were popular from 1970-2000, formative years for the feminist movement. Scholarship suggests a correlation between radio and women’s issues in Ireland but does not answer what elements create this. Here, I analyze 10 archival radio clips from Ireland’s national public service broadcaster, RTÉ, looking at how women’s issues are framed. After analyzing these clips, I found that Irish identity embedded in the shows allows for the discussion of controversial ideas. Radio promotes an inclusive environment, by dispelling shame and encouraging political conversation among women. This allows women to hear and be heard, creating a space for equal representation. Introduction As I was sitting on a bus from Dublin airport back to my apartment in Cork City, I heard a late-night radio show playing on the bus speakers. -

Rezoning and Amenities in New Development Plan
BUSINESS PRINTING THAT IS RIGHT UP EVERYONE'S STREET Le road to success may not run straight. So it's reassuring to know that, whatever new challenge is waiting around the comer, there's always Rezoning and Amenities one thing you can depend on. TheCardinal Press range of Business Printing in New Development Plan services. At The Cardinal Press we recognise that you Om'local councillors have put the final touc.;hes to the Draft Development Plan for Maynooth need services which exactly match the unique circum" and,fhe plan goes before a full meeting:df the Co. ~ouncil this Friday, February 26th. The main stances of your business. features of the plan include a proposal to rezone 238 aCI:es for hou~ing,.28 acres for sports fields, 10 ac;res fotj public park and 8 acres for a school and chtirch~ In addition, 100 acres ijas That's why we always offer tailOf"made assist" been zoned as Green Belt. The plan also includes provIsion for the building of a regional ring ance service and advice. road from Blacklion to the For exampIC, we'll put together a package of Straffan Road which is to be funded from development levies printing services to suit your individual business needs. Rapid Growth in Maynooth's Population to Continue arising from residential develop Helping you seize new opportunities as they arrive. And ment in that area. pointing out things you may not have considered, too. Significant Growth Planned Because we don't have a fixed tariff, you'll also All councillors appear to have find our charges very competitive. -

White Paper on a Framework for Supporting Voluntary Activity And
White Paper on a Framework for Supporting Voluntary Activity and for Developing the Relationship between the State and the Community and Voluntary sector 2 Foreword by an Taoiseach, Mr. Bertie Ahern TD. Voluntary activity forms the very core of all vibrant and inclusive societies. It involves an incredible diversity of types of activity, ranging from the very informal to the highly structured. It can mean anything from occasionally helping out in a local sports club to participation in major national organisations. Particularly in a time of great change in our country, we must work hard to protect and enhance the spirit of voluntary participation and we must see this as a key social goal. The great strength of voluntary activity is that it emerges organically from communities. It would be wrong for Government to seek to control and be involved in every aspect of voluntary activity, but there is no doubt that it can provide an enabling framework to help this activity. Where this involves direct supports, a delicate balance must be struck between having a relatively light official involvement and maintaining proper accountability. This White Paper signals a very clear intention of the Government to invest in enabling the voluntary Sector to serve individuals, communities and the country as a whole. It recognises the rights and responsibilities of everybody involved. It provides for a number of concrete initiatives to move the agenda forward. I look forward to the implementation of its recommendations and the contribution which it will make in the coming years. 3 Foreword by Minister for Social, Community and Family Affairs, Dermot Ahern TD. -

Raidió Teilifís Éireann Annual Report & Group Financial Statements 2011 Raidió Teilifís Éireann
Raidió Teilifís ÉiReann annual RepoRT & GRoup financial sTaTemenTs 2011 Raidió TeilifíS Éireann Highlights 1 Organisation Structure 2 What We Do 3 Chairman’s Statement 4 Director-General’s Review 6 Operational Review 10 Financial Review 40 Board 46 Executive 48 Corporate Governance 50 Board Members’ Report 54 Statement of Board Members’ Responsibilities 55 Independent Auditor’s Report 56 Financial Statements 57 Accounting Policies 64 Notes forming part of the Group Financial Statements 68 Other Reporting Requirements 103 Other Statistical Information 116 Financial History 121 RTÉ’S vision is to grow the TRust of the peoplE of Ireland as IT informs, inspires, reflects and enriches their lIvES. RTÉ’S mission is to: • NuRTure and reflect the CulTural and regional diversity of All the peoplE of Ireland • Provide distinctivE programming and services of the highest quAlITy and ambition, WITH the emphasis on home production • Inform the Irish PuBlic By delIvering the best comprehensivE independent news service possiblE • ENABlE national participation in All MAjor Events Raidió Teilifís Éireann Board 51st Annual Report and Group Financial Statements for the 12 months ended 31 December 2011, presented to the Minister for Communications, Energy and Natural Resources pursuant to section 109 and 110 of the Broadcasting Act 2009. Is féidir leagan Gaeilge den Tuarascáil a íoslódáil ó www.rte.ie/about/annualreport ANNuAl REPORT & GROuP FINANCIAl STATEMENTS 2011 HiGHliGHTs Since 2008 RTÉ has reduced its operating costs by close to 20% or €86 million. RTÉ continues to be Ireland’s With quality home-produced leading provider of digital programming and the best content with the country’s acquired programming from most popular Irish owned overseas, RTÉ increased its live website, the most popular peak-time viewing share on on-demand video service RTÉ One to 30.9% in 2011. -

Mhi Annual Report 2008
2008 annual report CHAIRMAN’S ADDRESS Mental Health Ireland Supporting Positive Mental Health Mensana House, 6 Adelaide Street, Dun Laoghaire, Co. Dublin Tel: 01 284 1166 Fax: 01 284 1736 Email: [email protected] Website: www.mentalhealthireland.ie CONTENTS CONTENTS Page Chairman’s Address 7 - 8 Funding and Fundraising 9 Work of Development Officers and Local Mental Health Associations 2008 10 - 11 Summary of their main activities and achievements 12 - 36 Information 37 Media Coverage 38 Annual Conference 2008 39 World Mental Health Day National Choral Singing Events 40 Partnerships 41 - 42 Mental Health Promotion in Schools and with Young People 43 Human Resources 44 Directors’ Report and Financial Statements 45 - 57 Directors’ Report Independent Auditors’ Report Audited Accounts Appendix : Local Mental Health Associations 59 Mental Health Ireland ANNUAL REPORT 2008 3 CHAIRMAN’S ADDRESS Board of Directors Officers Chairman: Mr John McGetrick Vice Chairman: Mr Michael Hughes Honorary Secretary: Mr Brian Glanville Honorary Treasurer: Dr John Connolly Members Mr Joe Casey Ms Colette Nolan Mr Liam Flynn Mr Derry O’Dwyer Mr Tom Giblin Fr Dan Joe O’Mahony Mr Liam Hassett Mr Diarmaid Ring Dr Tim Lynch Mr Brendan Madden Mr Paddy McGowan Mrs Fidelma Ryan Ms Maria Molloy Mr Jim Walsh Mr P. J. Murphy Mr John Whelan Registered Office Mensana House, 6 Adelaide Street, Dun Laoghaire, Co. Dublin. Bankers Bank of Ireland, Smithfield, Dublin 7 and AIB Investment Managers Ltd., Percy Place, Dublin 4. Auditors Brenson Lawlor. Brenson Lawlor House, Argyle Square, Morehampton Road, Dublin 4. Date of Incorporation As a company limited by guarantee, 22nd November, 1966 Place of Incorporation Dublin, Republic of Ireland Mental Health Ireland ANNUAL REPORT 2008 5 CHAIRMAN’S ADDRESS Dear Friends, It is with great pleasure that I introduce to you the Mental Health Ireland Annual Report for 2008. -
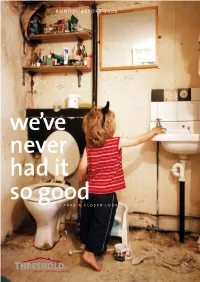
S O Ta K E a C L O S E R L O O K a N N UA L R E P O RT 2 0
ANNUAL REPORT 2005 we’ve never had it so goodso take a closer look threshold bridges the gap between housing and homelessness Threshold is a national not-for-profit organisation providers about the provisions of housing established in 1978. Our mission is to solve people’s legislation. housing problems and to campaign for a better By campaigning for appropriate housing as a right, housing system. We focus on those who are in Threshold promotes the vision that everyone in greatest need of our support - the marginalised and Ireland has access to an affordable, secure and those suffering from poverty and inequality. suitable home. We campaign for policies that Over the past 27 years, Threshold has helped more develop vibrant neighbourhoods and sustainable than 500,000 people move from inadequate communities that promote an inclusive society. housing and homelessness to becoming successful In carrying out research through our Housing members of sustainable communities. We Research Unit, and presenting our findings at local influence housing policy in Ireland and provide and national levels, Threshold makes the case an independent voice on housing issues. We for housing reform. A major report Opportunity significantly contributed to the introduction of the Knocks: Institutional Investment in the Private Residential Tenancies Act 2004, which provides Rented Sector in Ireland, supported by the Irish increased protections for tenants and landlords in Bankers Federation, looked at ways of encouraging the private rented sector. Irish financial institutions to directly invest in the Threshold provides independent advice and private rented property market, especially at the end advocacy services through our regional centres in of the market providing for households on modest Dublin, Cork and Galway, and via outreach clinics in or low incomes. -

Heffernan, Margaret
TEXT OF THE INTRODUCTORY ADDRESS DELIVERED BY: DR MICHAEL MURPHY, President, University College Cork on 20 September 2007, on the occasion of the conferring of the Degree of Doctor of Laws, honoris causa, on MARGARET HEFFERNAN A Sheánsailéir, a mhuintir na hOllscoile agus a dhaoine uaisle, Margaret Heffernan was born in Cork in 1942, the eldest of six children of Ben and Nora Dunne. Two years later, in March 1944 her father opened his first clothing shop in Patrick Street, Cork. This was the start of the retail phenomenon which became known as Dunnes Stores and is today Ireland's largest private retailer. Probably everyone in Ireland has shopped for food in Dunnes Stores and worn a St Bernard or a Dunnes Stores labeled garment. Margaret left school at 14 to join the family business, where she has remained to this day. Since the early 1990’s, together with her brother Frank, Margaret has been responsible for the leadership and direction of Dunnes Stores, and, in that time, the company has experienced enormous growth and transformation. Today, it is not only Ireland’s leading retailer, but also one of the country’s largest employers. The Dunnes Stores business encompasses 166 stores in Ireland (North and South), the United Kingdom and Spain, employing 20,000 people. Margaret Heffernan is justifiably proud of the fact that it is an Irish company and will continue as a family business through the Dunne, Heffernan and McMahon families. Whilst heavily involved in all aspects of the business, it is in the area of textiles that Margaret has been most influential. -
Health Service Executive Annual Report and Financial Statements
Health Service Executive Annual Report and Financial Statements 2008 Health Service Executive Annual Report and Financial Statements 2008 Oak House Dr Steevens’ Hospital Limetree Avenue Steevens’ Lane Millennium Park Dublin 8 Naas Telephone: 01 6352000 Co. Kildare www.hse.ie Telephone: 045 880400 www.hse.ie May 2009 ISBN 978-1-906218-24-9 © 2009 HSE 2008 HSE Calendar Examples of some of the milestones achieved during the year January July The new Haematology and Oncology Day Unit at Our Lady’s SKILL project commenced to educate, develop and train Children Hospital, Crumlin, opened. support staff to enhance their role in the quality of services National Maternity Hospital, Holles St, Dublin and St. Lukes, delivered. Kilkenny became the first hospitals to introduceprescribing ‘Improving our Services: A User’s Guide to Managing by nurses and midwives. Change in the HSE’ launched on www.hseland.ie New Consultants Contract commenced. February Oncology Day Unit at Our Lady of Lourdes Hospital, Drogheda. www.hseland.ie the HSE on line learning centre launched. August National International Health Strategy 2007-2012 launched by Minister for Health and Children. Major Cost Management Initiative commenced with key Ireland’s firstCommunity Infusion Centre opened on site HSE suppliers. of Kilcreene Hospital, Kilkenny. Tenders invited for main Mater Adult Hospital, Dublin and Letterkenny General Hospital Emergency Department March and Ward Block. A joint initiative with Irish Coast Guard, the Marine Ambulance September Response Team (MART) for deployment to major emergencies in inland waterways and at sea, was established. Treo Nua, a Multidimensional Treatment Foster Care Cardiac First Responder Guide launched. -

Annual Report & Group Financial Statements 2018 Vision, Mission and Values Some Highlights from 2018 Who We Are Statistical Information
A Year in Review Annual Report & Group Financial Statements 2018 Vision, Mission and Values Some Highlights from 2018 Who We Are Statistical Information RTÉ: The Year in Numbers Chair’s Statement What We Made in 2018 Director-General’s Review What We Won in 2018 Financial Review What We Did in 2018 Distribution, Digital, Delivery RTÉ is Ireland’s Raidió Teilifís Éireann Board Today, The 58th Annual Report and Group Financial national public-service Statements for the 12 months ended 31 tomorrow, media organisation December 2018 presented to the Minister for Communications, Climate Action and – on television, radio, Environment in line with sections 109 and 110 together online and mobile. of the Broadcasting Act 2009. Is féidir leagan Gaeilge den Tuarascáil a íoslódáil ó www.rte.ie/annualreport Board of RTÉ Independent Auditor’s Report Other Reporting Requirements Executive Financial Statements Other Statistical Information Corporate Governance Notes Forming Part of the Group Financial History Financial Statements Board Members’ Report Appendix to the Group Financial Statements – Accounting Policies Statement of Board Members’ Responsibilities Vision Mission To champion Irish culture by captivating To enrich Irish life with content that audiences with trusted, engaging and challenges, educates and entertains. challenging content; celebrating our country’s rich diversity; and cultivating Ireland’s talent. Values As an organisation and individually, RTÉ will be outward looking, creative, respectful, sustainable and accountable, collaborative and transparent, and will demonstrate the following behaviours: Outward Looking Have a deep understanding of its audience and their needs. Invest time and energy in monitoring changes in the media landscape. Creative Be resourceful and innovative in how it makes its content. -

Rter, and Global Competition Becomes Even Greater, the Effects of Digital Disruption on Media Are Likely to Become Even More Fast-Moving and Profound
Contents Introduction 1. How should Government develop and support the concept and role of public service media, and what should its role in relation to public service content in the wider media be? 2. What is the best model for future funding of public service media in Ireland? What approach best supports independent editorial oversight while achieving value for money and delivering on public service aims? 3. How should media be governed and regulated? Conclusion 1 The establishment of the Future of Media Commission is timely and necessary. The public space occupied by the media is fundamental to our sense of ourselves – daily it shapes our shared understanding of the society and culture in which we all live. Much is at stake if a sustainable future for the sector is not secured. For 60 years RTÉ has been companion to, participant in, and observer of all that has changed in Ireland. It has been RTÉ’s duty to investigate it, report it, reflect it, and celebrate it. RTÉ has simultaneously been a mirror and a lens, reflecting and focusing the national conversations, making sense of our shared, constantly unfolding story. Public service media now exists in a very different world from when RTÉ was established. Audiences in Ireland now live in a transformed media and communications landscape. With unlimited choice, with every interest and taste catered for, audiences enjoy a digital world - always on, accessible across multiple devices and, increasingly, delivered or mediated by global companies. Audiences today exercise control over when and how they consume information, journalism, programming and content. -

Devils and Angels
Devils and Angels The Ideological Construction of Poverty Stories on RTE Television Eoin Devereux BA MA (NUI) Thesis presented for the award of PhD. Supervisor: Professor Farrel Corcoran, School of Communications, Dublin City University, Glasnevin, Dublin 9. Submitted April 1996. Declaration I hereby certify that this material, which I now submit for assessment on the programme of study leading to the award of the degree of PhD, is entirely my own work and has not been taken from the work of others save and to the extent that such work has been cited and acknowledged within the text of my own work. Date: 1 / ^ ^ L ii Thesis Abstract This thesis investigates how Radio Telelis Eireann (RTE) constructs television stories about poverty. Using a combination of critical content analysis and an ethnography of the production context of television programmes, the study examines poverty stories on factual, fictional and fund-raising television. The study begins with an account of how existing social science discourse has considered the phenomenon of poverty in the Republic of Ireland. It proceeds to examine the limited amount of debate about media coverage of poverty. The case for a largely qualitative methodological approach is then outlined. The main part of the study is an analysis of how poverty stories are constructed on RTE’s Six-One News, Tuesday File, Glenroe and the People in Need Telethon. Each of these four chapters consider the respective programmes in terms of their history, production context, the content of their poverty coverage, as well as a consideration of the ideology of that coverage. -

Welcome to Teaching
VOL.30 / NO.1 SEPTEMBER ‘07 WELCOME TO TEACHING – A GUIDE FOR NEW MEMBERS GENDER IMBALANCES IN IRISH EDUCATION TUI CREDIT UNION CELEBRATES 40 YEARS PENSION ISSUES CONTENTS Cover Story VOL.30 / NO.1 SEPTEMBER ‘07 Social Partnership – A Fair Deal? With social partnership in Ireland now 20 years old, TUI General Secretary Jim Dorney examines its ups and downs and highlights the negative effect of rising infl ation in the context of Towards 2016. WELC OME TO TEAC HING – A GUIDE FOR NEW MEMBERS GENDER IMBALANCES IN IRISH EDUCAT ION TUI CREDIT UNION CELEBRAT ES 40 YEARS PENSION ISSUES Contents TUI NEWS FEATURES Gender Imbalances in Irish Education Minister Ms. Mary Hanafi n, launched a new report on gender in Irish education recently entitled Sé Sí. This report gives an overview of the issue of gender in education from primary school right through to higher and further education. 4 A Fair Deal? The article focuses on chapter 8 of the Report in relation to Educational Personnel. 4 Gender Imbalances Second Level Teachers The report presents an overview of second level teachers by gender from 1985 to 2003. In 1985 the ratio among second level teachers was 50-50. From 6 SéSí Gender Report Analysis 1985 to 2003 while the number of female Posts of Responsibility a proper analysis is not possible as data in teachers at second level increased by respect of the gender of post holders going 3,500 the number of male teachers in No data on the gender breakdown back in time in not available. the second level system declined by 500 of post of responsibility holders in during the same period.