Top 50 Frequently Used Diagnostic Codes Gastroenterology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Abnormal Liver Chemistries
ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries Paul Y. Kwo, MD, FACG, FAASLD1, Stanley M. Cohen, MD, FACG, FAASLD2, and Joseph K. Lim, MD, FACG, FAASLD3 1Division of Gastroenterology/Hepatology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California, USA; 2Digestive Health Institute, University Hospitals Cleveland Medical Center and Division of Gastroenterology and Liver Disease, Department of Medicine, Case Western Reserve University School of Medicine, Cleveland, Ohio, USA; 3Yale Viral Hepatitis Program, Yale University School of Medicine, New Haven, Connecticut, USA. Am J Gastroenterol 2017; 112:18–35; doi:10.1038/ajg.2016.517; published online 20 December 2016 Abstract Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defined as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defined as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. -

Inside the Minds: the Art and Science of Gastroenterology
Gastroenterology_ptr.qxd 8/24/07 11:29 AM Page 1 Inside the Minds ™ Inside the Minds ™ The Secrets to Success in The Art and Science of Gastroenterology Gastroenterology The Art and Science of Gastroenterology is an authoritative, insider’s perspective on the var- ious challenges in this field of medicine and the key qualities necessary to become a successful Top Doctors on Diagnosing practitioner. Featuring some of the nation’s leading gastroenterologists, this book provides a Gastroenterological Conditions, Educating candid look at the field of gastroenterology—academic, surgical, and clinical—and a glimpse Patients, and Conducting Clinical Research into the future of a dynamic practice that requires a deep understanding of pathophysiology and a desire for lifelong learning. As they reveal the secrets to educating and advocating for their patients when diagnosing their conditions, these authorities offer practical and adaptable strategies for excellence. From the importance of soliciting a thorough medical history to the need for empathy towards patients whose medical problems are not outwardly visible, these doctors articulate the finer points of a profession focused on treating disorders that dis- rupt a patient’s lifestyle. The different niches represented and the breadth of perspectives presented enable readers to get inside some of the great innovative minds of today, as experts offer up their thoughts around the keys to mastering this fine craft—in which both sensitiv- ity and strong scientific knowledge are required. ABOUT INSIDETHE MINDS: Inside the Minds provides readers with proven business intelligence from C-Level executives (Chairman, CEO, CFO, CMO, Partner) from the world’s most respected companies nationwide, rather than third-party accounts from unknown authors and analysts. -

Nutrition Considerations in the Cirrhotic Patient
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #204 NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #204 Carol Rees Parrish, MS, RDN, Series Editor Nutrition Considerations in the Cirrhotic Patient Eric B. Martin Matthew J. Stotts Malnutrition is commonly seen in individuals with advanced liver disease, often resulting from a combination of factors including poor oral intake, altered absorption, and reduced hepatic glycogen reserves predisposing to a catabolic state. The consequences of malnutrition can be far reaching, leading to a loss of skeletal muscle mass and strength, a variety of micronutrient deficiencies, and poor clinical outcomes. This review seeks to succinctly describe malnutrition in the cirrhosis population and provide clarity and evidence-based solutions to aid the bedside clinician. Emphasis is placed on screening and identification of malnutrition, recognizing and treating barriers to adequate food intake, and defining macronutrient targets. INTRODUCTION The Problem ndividuals with cirrhosis are at high risk of patients to a variety of macro- and micronutrient malnutrition for a multitude of reasons. Cirrhotic deficiencies as a consequence of poor intake and Ilivers lack adequate glycogen reserves, therefore altered absorption. these individuals rely on muscle breakdown as an As liver disease progresses, its complications energy source during overnight periods of fasting.1 further increase the risk for malnutrition. Large Well-meaning providers often recommend a variety volume ascites can lead to early satiety and decreased of dietary restrictions—including limitations on oral intake. Encephalopathy also contributes to fluid, salt, and total calories—that are often layered decreased oral intake and may lead to inappropriate onto pre-existing dietary restrictions for those recommendations for protein restriction. -

Etiology of Upper Gastrointestinal Haemorrhage in a Teaching Hospital
TAJ June 2008; Volume 21 Number 1 ISSN 1019-8555 The Journal of Teachers Association RMC, Rajshahi Original Article Etiology of Upper Gastrointestinal Haemorrhage in a Teaching Hospital M Uddin Ahmed1, M Abdul Ahad2, M A Alim2, A R M Saifuddin Ekram3, Q Abdullah Al Masum4, Sumona Tanu5, Refaz Uddin6 Abstract A descriptive study on all cases of haematemesis and or melaena was carried out at Rajshahi Medical College Hospital to observe the demographic profile, clinical presentation, cause and outcome of upper gastrointestinal bleeding in a tertiary hospital of Bangladesh. Fifty adult patients presenting with haematemesis and or melaena admitted consecutively into medical unit were evaluated through proper history taking, thorough clinical examination, endoscopic examination with in 48 hours of first presentation and other related investigations. Patients those who were not stabilized haemodynamically with in 48 hours of resuscitation and endoscopy could not be done with in that period were excluded from this study. Results our results showed that out of 50 patients 44 were male and 6 were female and average age of the patients was 39.9 years. Most of the patients were from low socio-economic condition. Farmers, service holders and laborers were the most (57%) affected group. Haematemesis and melaena (42%), only melaena (42%) and only haematemesis (16%) were the presenting features. Endoscopy revealed that duodenal ulcer( 34%) was the most common cause of UGI bleeding followed by rupture of portal varices( 16%) , neoplasm( 10%) , gastric ulcer ( 08%) and gastric erosion( 06%). Acute upper GI bleeding is a common medical problem that is responsible for significant morbidity and mortality. -

Obscure Gastrointestinal Bleeding in Cirrhosis: Work-Up and Management
Current Hepatology Reports (2019) 18:81–86 https://doi.org/10.1007/s11901-019-00452-6 MANAGEMENT OF CIRRHOTIC PATIENT (A CARDENAS AND P TANDON, SECTION EDITORS) Obscure Gastrointestinal Bleeding in Cirrhosis: Work-up and Management Sergio Zepeda-Gómez1 & Brendan Halloran1 Published online: 12 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Obscure gastrointestinal bleeding (OGIB) in patients with cirrhosis can be a diagnostic and therapeutic challenge. Recent advances in the approach and management of this group of patients can help to identify the source of bleeding. While the work-up of patients with cirrhosis and OGIB is the same as with patients without cirrhosis, clinicians must be aware that there are conditions exclusive for patients with portal hypertension that can potentially cause OGIB. Recent Findings New endoscopic and imaging techniques are capable to identify sources of OGIB. Balloon-assisted enteroscopy (BAE) allows direct examination of the small-bowel mucosa and deliver specific endoscopic therapy. Conditions such as ectopic varices and portal hypertensive enteropathy are better characterized with the improvement in visualization by these techniques. New algorithms in the approach and management of these patients have been proposed. Summary There are new strategies for the approach and management of patients with cirrhosis and OGIB due to new develop- ments in endoscopic techniques for direct visualization of the small bowel along with the capability of endoscopic treatment for different types of lesions. Patients with cirrhosis may present with OGIB secondary to conditions associated with portal hypertension. Keywords Obscure gastrointestinal bleeding . Cirrhosis . Portal hypertension . -
EGD) Is a Common Endoscopic Procedure Done for Suspected and Proven Lesions of the Upper Gastrointestinal Tract
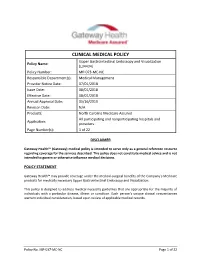
CLINICAL MEDICAL POLICY Upper Gastrointestinal Endoscopy and Visualization Policy Name: (L34434) Policy Number: MP-073-MC-NC Responsible Department(s): Medical Management Provider Notice Date: 07/01/2018 Issue Date: 08/01/2018 Effective Date: 08/01/2018 Annual Approval Date: 05/16/2019 Revision Date: N/A Products: North Carolina Medicare Assured All participating and nonparticipating hospitals and Application: providers Page Number(s): 1 of 22 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical benefits of the Company’s Medicare products for medically necessary Upper Gastrointestinal Endoscopy and Visualization. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. Policy No. MP-037-MC-NC Page 1 of 22 PROCEDURES CMS NATIONAL COVERAGE POLICY Title XVIII of the Social Security Act, §1862(a)(1)(A) allows coverage and payment for only those services that are considered to be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member. Title XVIII of the Social Security Act §1833(e) prohibits Medicare payment for any claim which lacks the necessary information to process the claim. Title XVIII of the Social Security Act §1862(a)(7) excludes routine physical examinations. -

Hematemesis and Melena Chapter
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients. -

Diarrhea Gastroenterology
Diarrhea Referral Guide: Gastroenterology Page 1 of 2 Diagnosis/Definition: The rectal passage of an increased number of stools per day which are watery, bloody or loosely formed. By history and stool sample. Initial Diagnosis and Management: Most patients don’t need to be worked up for their diarrhea. Most cases of diarrhea are self-limiting, caused by a gastroenteritis viral agent. Patients need to be advised to drink plenty of fluids, take some NSAIDSs or Tylenol for fevers and flu-related myalgias. If the patient comes to you with a history of bloody diarrhea, fever, severe abdominal pain, and diarrhea longer than 2 weeks or associated with electrolyte abnormalities or is elderly or immunocompromised, they need to be seen by GI. Work-up in these patients should consist of a thorough history (be sure to get travel history, medications including herbal remedies and possible infectious contacts) and physical examination. Labs should include a chem. 7, CBC with differential and stool WBCs, cultures, qualitative fecal fat. If there is the possibility that this could be antibiotic related C. difficile then order a C. diff toxin on the stool. Only order an O and P on the stool\l if the patient gives you a recent history of international travel, wildern4ess camping/hiking or may be immunocompromised. Make sure to ask about mil product ingestion as it relates to the diarrhea. Fifty percent of adult Caucasians and up to 90% of African Americans, Hispanics, and Asians have some degree of milk intolerance. If from your history and laboratory studies indicate a specific etiology the following chart may help with initial therapy. -

Children's Gastroenterology, Hepatology, and Nutrition
GI_InsertCard 4/24/09 2:03 PM Page 1 CHILDREN’S GASTROENTEROLOGY, HEPATOLOGY, AND NUTRITION CONSULT AND REFERRAL GUIDELINES FOR COMMON GI PROBLEMS DIAGNOSIS/SYMPTOM SUGGESTIONS FOR POSSIBLE PRE-REFERRAL CONSIDER INITIAL WORK-UP THERAPY REFERRAL WHEN CHRONIC ABDOMINAL PAIN ICD-9 code – 789.0 • Weight and height percentiles • Treatment of constipation, If symptoms persist after Age: toddler to adolescence • Urinanalysis if present improvement of stooling • CBC with dif ESR or CRP • Acid suppression - H2 receptor pattern, trial of a lactose-free • Stool Studies: • Antagonist or proton pump diet and lack of response – guaiac • Inhibitor to acid suppression, referral – consider EIA antigen for giardia • Trial off lactose should be made. The child • Careful evaluation of stooling pattern may require endoscopy • Diary to look for possible triggers such as foods, (EGD) and/or colonoscopy. activities or stressors CHRONIC, NON-BLOODY DIARRHEA ICD-9 code – 787.91 • Weight and height percentiles • Treat any dietary abnormality If Symptoms persist, referral Age: preschool to adolescence • Stool studies: (e.g. high fructose and/or low fat) should be made. The child – guaiac • Try increased fiber in diet may require EGD and/or – consider leukocytes • Diary of dairy and other food colonoscopy. – culture intake in relation to symptoms – EIA antigen for giardia – C. difficile toxin titer – Reducing substances, pH, – Sudan stain (spot test for fecal fat) • CBC with differential, ESR or CRP • Albumin • Quantitative IgA and anti-tTG Antibody (screen for celiac) • Consider sweat test • Consider upper GI with small bowel follow through • Consider laxative abuse, especially in adolescent females BLOODY DIARRHEA (COLITIS) ICD-9 code – 556 • Stool studies: If evaluation is negative, food If symptoms persist, referral Age: infancy – guaiac protein allergy is likely. -

Hematemesis Melena Due to Helicobacter Pylori Infection in Duodenal Ulcer: a Case Report and Literature Review
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Index Copernicus Value (2016): 79.57 | Impact Factor (2017): 7.296 Hematemesis Melena due to Helicobacter Pylori Infection In Duodenal Ulcer: A Case Report and Literature Review Ayu Budhi Trisna Dewi Rahayu Sutanto1, I Made Suma Wirawan2 1General Practitioner Wangaya Hospital Denpasar Bali Indonesia 2 Endoscopy Unit of Internal Medicine Wangaya Hospital Denpasar Bali Indoensia Abstract: A Balinese woman, 60 years old complaint of hematemesis and melena. Esophagogastroduodenoscopy performed one day after admission and revealed a soliter ulcer at duodenum bulb. Histopathology examination revealed a spherical like organism suspected Helicobacter pylori (H. pylori) infection. Eradication of H. pylori by triple drug consisting of omeprazole, amoxicillin and chlarythromycin as the standard protocol of eradication within 14 days. Reevaluation by esophagogastroduodenoscopy examination will perform in the next 3 months to evaluate the treatment succesfull. Keywords: peptic ulcer, duodenum, H. pylori 1. Background also normal. The patient diagnosed with hematemesis suspect peptic ulcer. The patient was then admitted to ward Approximately 500,000 persons develop peptic ulcer disease and giving infusion ringer lactat, proton pump inhibitor in the United States each year. in 70 percent of patients it esomeprazole bolus 40 mg intravenous and continuous with occurs between the ages of 25 and 64 years. The annual 8 mg/ hours and planned for esofagogastroduodenoscopy to direct and indirect health care costs of the disease are evaluate the source of hematemesis. estimated at about $10 billion. However, the incidence of peptic ulcers is declining, possibly as a result of the increasing use of proton pump inhibitors and decreasing rates of Helicobacter pylori (H. -

Dysphagia: a Symptom Not a Disease
th Case al Re e p Lohe and Kadu, Oral health case Rep 2016, 2:2 H o l r a t r s O Oral Health Case Reports DOI: 10.4172/2471-8726.1000117 ISSN: 2471-8726 ResearchReview Article Article OpenOpen Access Access Dysphagia: A Symptom Not a Disease Vidya K Lohe1* and Ravindra P Kadu2 1Sharad Pawar Dental College and Hospital, DMIMS (DU), Maharashtra, India 2Jawaharlal Nehru Medical College and Hospital DMIMS (DU), Maharashtra, India Abstract Dysphagia is difficulty in swallowing food semi-solid or solid, liquid, or both. There are many disorder conditions predisposing to dysphagia such as mechanical strokes or esophageal diseases even if neurological diseases represent the principal one. Cerebrovascular pathology is today the leading cause of death in developing countries, and it occurs most frequently in individuals who are at least 60 years old. Patients with dysphagia may walk into dental clinic and because dysphagia is a symptom not a disease, it is a practicing dentist’s duty to recognize the underlying cause and then take treatment decisions. Among the most frequent complications of dysphagia are increased mortality and aspiration pneumonia, dehydration, malnutrition, and long-term hospitalization. This review article discusses the pathophysiology, classification, evaluation, investigations and treatment modalities of dysphagia. Keywords: Oropharyngeal dysphagia; Oesophageal dysphagia; Classification of Dysphagia Barium swallow • Oropharyngeal dysphagia is usually described as the inability to Introduction initiate the act of swallowing. It is a “transfer” problem of impaired ability to move food from the mouth into the upper esophagus. It is Phagia meaning swallowing and dysphagia means difficulty in caused by weakness of tongue muscles. -

Liver Dysfunction in the Intensive Care Unit ANNALS of GASTROENTEROLOGY 2005, 18(1):35-4535
Liver dysfunction in the intensive care unit ANNALS OF GASTROENTEROLOGY 2005, 18(1):35-4535 Review Liver dysfunction in the intensive care unit Aspasia Soultati, S.P. Dourakis SUMMARY crosis factor-alpha, is pivotal for the development of liver injury at that stage. Liver dysfunction plays a significant role in the Intensive Care Unit (ICU) patients morbidity and mortality. Although determinations of aminotransferases, coagulation Metabolic, hemodynamic and inflammatory factors studies, glucose, lactate and bilirubin can detect hepatic contribute in liver damage. Hemorrhagic shock, septic shock, injury, they only partially reflect the underlying pathophys- multiple organ dysfunction, acute respiratory dysfunction, iological mechanisms. Both the presence and degree of jaun- metabolic disorders, myocardial dysfunction, infection from dice are associated with increased mortality in a number of hepatitis virus, and therapeutic measures such as blood non hepatic ICU diseases. transfusion, parenteral nutrition, immunosuppresion, and Therapeutic approaches to shock liver focus on the drugs are all recognised as potential clinical situations on prevention of precipitating causes. Prompt resuscitation, the grounds of which liver dysfunction develops. definitive treatment of sepsis, meticulous supportive care, The liver suffers the consequences of shock- or sepsis-in- controlling of circulation parameters and metabolism, in ducing circumstances, which alter hepatic circulation pa- addition to the cautious monitoring of therapeutic measures rameters, oxygen supply and inflammatory responses at the such as intravenous nutrition, mechanical ventilation and cellular level. Moreover, the liver is an orchestrator of met- catecholamine administration reduce the incidence and abolic arrangements which promote the clearance and pro- severity of liver dysfunction. Only precocious measures can duction of inflammatory mediators, the scavenging of bac- be taken to prevent hepatitis in ICU.