Intestinal Transplantation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MD Anderson Lodging
All information is subject to change! For the latest lodging information see http://joeshouse.org/Lodging/tabid/115/Default.aspx?hid=184&state=Texas MD Anderson Lodging List - Other Name Address Phone Amenities Notes Reservations Rates Distance American Various Hotels 888 227 6333 Varies with ACS along with local hotels provide T0 request hotel Some hotels offer Varies with Cancer Society’s hotel overnight accommodations to cancer lodging, please contact free nights, others hotel Hotel Partners patients who travel for outpatient the American Cancer offer rooms at Program treatment. All accommodations are Society at 877-227- discounted rates. provided based on eligibility 1618. Requests for Patients are requirements, are subject to lodging are met on a responsible for all availability and restrictions imposed first-come, first-served additional charges, by the participating hotels. Special basis and must be other than the room requests, such as pet-friendly and submitted at least two- charge…i.e. shuttle services, are taken into weeks prior to the date parking fees, room consideration if mentioned. lodging is needed. service, etc. Name Address Phone Amenities Notes Reservations Rates Distance Ronald 1907 713.795.3500 LF, NS, P, I, ** Temporarily closed to new A health care provider Requested rate - .4 Miles MacDonald Holcombe patients due to COVID-19 ** Ronald or state social worker $25.00 per night., House Blvd, Houston, Microwave McDonald House is a "home away must refer families however no family TX 77030 Refrigerator from home" for families and children staying for the first is turned away due Free Local being treated at Texas Medical time. -

The Herbivore Digestive System Buffalo Zebra
The Herbivore Digestive System Name__________________________ Buffalo Ruminant: The purpose of the digestion system is to ______________________________ _____________________________. Bacteria help because they can digest __________________, a sugar found in the cell walls of________________. Zebra Non- Ruminant: What is the name for the largest section of Organ Color Key a ruminant’s Mouth stomach? Esophagus __________ Stomach Small Intestine Cecum Large Intestine Background Information for the Teacher Two Strategies of Digestion in Hoofed Mammals Ruminant Non‐ruminant Representative species Buffalo, cows, sheep, goats, antelope, camels, Zebra, pigs, horses, asses, hippopotamus, rhinoceros giraffes, deer Does the animal Yes, regurgitation No regurgitation regurgitate its cud to Grass is better prepared for digestion, as grinding Bacteria can not completely digest cell walls as chew material again? motion forms small particles fit for bacteria. material passes quickly through, so stool is fibrous. Where in the system do At the beginning, in the rumen Near the end, in the cecum you find the bacteria This first chamber of its four‐part stomach is In this sac between the two intestines, bacteria digest that digest cellulose? large, and serves to store food between plant material, the products of which pass to the rumination and as site of digestion by bacteria. bloodstream. How would you Higher Nutrition Lower Nutrition compare the nutrition Reaps benefits of immediately absorbing the The digestive products made by the bacteria are obtained via digestion? products of bacterial digestion, such as sugars produced nearer the end of the line, after the small and vitamins, via the small intestine. intestine, the classic organ of nutrient absorption. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Newsletter Spring 2018
A NEWSLETTER OF GIFT OF LIFE TRANSPLANT HOUSE SPRING/SUMMER 2018 DONATE LIFE MONTH GIFT OF LIFE Join us in recognition at the TRANSPLANT HOUSE following April events: A HOME THAT HELPS AND HEALS April 13 - Walk of Remembrance April 14 - Timmay 5k See our Facebook for details. AWAKENED BY THE GIFT OF LIFE sk Teresa Hoff what her favorite movie is and she will tell you empathicallyA it is Sleeping Beauty. Unlike the Disney movie, Teresa’s story is not a fairy tale and she wasn’t awakened by a prince. Teresa was awakened by a liver transplant! It all began at age 14. Teresa swam in a hometown lake which contained the e-coli bacteria. She spent the entire summer becoming increasingly ill and a visit to the doctor revealed a diagnosis of both Crohn’s disease and ulcerative colitis. The course of treatment was prednisone and while not Teresa, on right, four days pre-transplant with completely recovered, Teresa completed her her sister, Mary. high school career with honors. She entered the University of North Dakota, but grew While this was an intensely difficult time, it increasingly ill. She was referred to Mayo was also a happy time. Teresa met and Clinic at age 19 and was told her colon married her husband, Brad in May of 2005 would have to be removed. Teresa had the and began her 1st job. A bout of cholangitis procedure performed and, amazingly, landed her back at Mayo Clinic and in June returned to college, graduating in 2005 2008, Teresa received her 1st life-saving liver with a degree in Physical Therapy. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -

Epithelial Control of Gut-Associated Lymphoid Tissue Formation Through P38α-Dependent Restraint of NF-Κb Signaling
Epithelial Control of Gut-Associated Lymphoid Tissue Formation through p38 α -Dependent Restraint of NF-κB Signaling This information is current as Celia Caballero-Franco, Monica Guma, Min-Kyung Choo, of September 27, 2021. Yasuyo Sano, Thomas Enzler, Michael Karin, Atsushi Mizoguchi and Jin Mo Park J Immunol 2016; 196:2368-2376; Prepublished online 20 January 2016; doi: 10.4049/jimmunol.1501724 Downloaded from http://www.jimmunol.org/content/196/5/2368 Supplementary http://www.jimmunol.org/content/suppl/2016/01/19/jimmunol.150172 Material 4.DCSupplemental http://www.jimmunol.org/ References This article cites 53 articles, 20 of which you can access for free at: http://www.jimmunol.org/content/196/5/2368.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 27, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Epithelial Control of Gut-Associated Lymphoid Tissue Formation through p38a-Dependent Restraint of NF-kB Signaling Celia Caballero-Franco,* Monica Guma,†,‡ Min-Kyung Choo,* Yasuyo Sano,* Thomas Enzler,*,x Michael Karin,†,{ Atsushi Mizoguchi,‖ and Jin Mo Park* The protein kinase p38a mediates cellular responses to environmental and endogenous cues that direct tissue homeostasis and immune responses. -
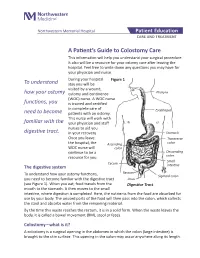
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -

Overview of Gastrointestinal Function
Overview of Gastrointestinal Function George N. DeMartino, Ph.D. Department of Physiology University of Texas Southwestern Medical Center Dallas, TX 75390 The gastrointestinal system Functions of the gastrointestinal system • Digestion • Absorption • Secretion • Motility • Immune surveillance and tolerance GI-OP-13 Histology of the GI tract Blood or Lumenal Serosal Side or Mucosal Side Structure of a villus Villus Lamina propria Movement of substances across the epithelial layer Tight junctions X Lumen Blood Apical membrane Basolateral membrane X X transcellular X X paracellular GI-OP-19 Histology of the GI tract Blood or Lumenal Serosal Side or Mucosal Side Motility in the gastrointestinal system Propulsion net movement by peristalsis Mixing for digestion and absorption Separation sphincters Storage decreased pressure GI-OP-42 Intercellular signaling in the gastrointestinal system • Neural • Hormonal • Paracrine GI-OP-10 Neural control of the GI system • Extrinsic nervous system autonomic central nervous system • Intrinsic (enteric) nervous system entirely with the GI system GI-OP-14 The extrinsic nervous system The intrinsic nervous system forms complete functional circuits Sensory neurons Interneurons Motor neurons (excitatory and inhibitory) Parasympathetic nerves regulate functions of the intrinsic nervous system Y Reflex control of gastrointestinal functions Vago-vagal Afferent reflex Salivary Glands Composition of Saliva O Proteins α−amylase lactoferrin lipase RNase lysozyme et al mucus O Electrolyte solution water Na+ , K + - HCO3 -

42 CFR Ch. IV (10–1–12 Edition) § 410.35
§ 410.35 42 CFR Ch. IV (10–1–12 Edition) the last screening mammography was (1) Colorectal cancer screening tests performed. means any of the following procedures furnished to an individual for the pur- [59 FR 49833, Sept. 30, 1994, as amended at 60 FR 14224, Mar. 16, 1995; 60 FR 63176, Dec. 8, pose of early detection of colorectal 1995; 62 FR 59100, Oct. 31, 1997; 63 FR 4596, cancer: Jan. 30, 1998] (i) Screening fecal-occult blood tests. (ii) Screening flexible § 410.35 X-ray therapy and other radi- sigmoidoscopies. ation therapy services: Scope. (iii) In the case of an individual at Medicare Part B pays for X-ray ther- high risk for colorectal cancer, screen- apy and other radiation therapy serv- ing colonoscopies. ices, including radium therapy and ra- (iv) Screening barium enemas. dioactive isotope therapy, and mate- (v) Other tests or procedures estab- rials and the services of technicians ad- lished by a national coverage deter- ministering the treatment. mination, and modifications to tests [51 FR 41339, Nov. 14, 1986. Redesignated at 55 under this paragraph, with such fre- FR 53522, Dec. 31, 1990] quency and payment limits as CMS de- termines appropriate, in consultation § 410.36 Medical supplies, appliances, with appropriate organizations and devices: Scope. (2) Screening fecal-occult blood test (a) Medicare Part B pays for the fol- means— lowing medical supplies, appliances (i) A guaiac-based test for peroxidase and devices: activity, testing two samples from (1) Surgical dressings, and splints, each of three consecutive stools, or, casts, and other devices used for reduc- (ii) Other tests as determined by the tion of fractures and dislocations. -

Silent Reflux (Also Called LPR Or EOR)
Silent reflux (also called LPR or EOR) This leaflet explains what your condition is, why it happens, what the symptoms are and how it can be managed. If there is anything you don’t understand or if you have any further questions please talk to your doctor or nurse. What is silent reflux? Everyone has juices in the stomach which are acidic and digest and break down food. At the top of the stomach there is a muscular valve which closes to prevent food and stomach juices escaping upwards into the gullet. If this muscular valve (oesophageal sphincter) does not work very well, the stomach juices can leak backwards into the gullet, causing reflux or symptoms of indigestion (heartburn). However, in some people, small amounts of stomach juice can spill even further back into the back of your throat, affecting the throat lining and your voice box (larynx) and causing irritation and hoarseness. This is known as laryngo pharyngeal reflux (LPR) or extra oesophageal reflux (EOR). Its common name is 'silent reflux' because many people do not experience any of the classic symptoms of heartburn or indigestion. Silent reflux can occur during the day or night, even if a person hasn't eaten anything. Usually, however, silent reflux occurs at night. What are the symptoms of silent reflux? The most common symptoms are: • A sensation of food sticking or a feeling of a lump in the throat. • A hoarse, tight or 'croaky' voice. • Frequent throat clearing. • Difficulty swallowing (especially tablets or solid foods). • A sore, dry and sensitive throat. • Occasional unpleasant "acid" or "bilious" taste at the back of the mouth. -

Anatomy of Small Intestine Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Anatomy of Small Intestine Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives: At the end of the lecture, students should: List the different parts of small intestine. Describe the anatomy of duodenum, jejunum & ileum regarding: the shape, length, site of beginning & termination, peritoneal covering, arterial supply & lymphatic drainage. Differentiate between each part of duodenum regarding the length, level & relations. Differentiate between the jejunum & ileum regarding the characteristic anatomical features of each of them. Abdomen What is Mesentery? It is a double layer attach the intestine to abdominal wall. If it has mesentery it is freely moveable. L= liver, S=Spleen, SI=Small Intestine, AC=Ascending Colon, TC=Transverse Colon Abdomen The small intestines consist of two parts: 1- fixed part (no mesentery) (retroperitoneal) : duodenum 2- free (movable) part (with mesentery) :jejunum & ileum Only on the boys’ slides RELATION BETWEEN EMBRYOLOGICAL ORIGIN & ARTERIAL SUPPLY مهم :Extra Arterial supply depends on the embryological origin : Foregut Coeliac trunk Midgut superior mesenteric Hindgut Inferior mesenteric Duodenum: • Origin: foregut & midgut • Arterial supply: 1. Coeliac trunk (artery of foregut) 2. Superior mesenteric: (artery of midgut) The duodenum has 2 arterial supply because of the double origin The junction of foregut and midgut is at the second part of the duodenum Jejunum & ileum: • Origin: midgut • Arterial