Examination of the Cardiopulmonary System Mary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abdominal Coarctation in a Hypertensive Female Collegiate Basketball Player B Sloan, S Simons, a Stromwall
1of2 Br J Sports Med: first published as 10.1136/bjsm.2002.004176 on 23 September 2004. Downloaded from CASE REPORT Abdominal coarctation in a hypertensive female collegiate basketball player B Sloan, S Simons, A Stromwall ............................................................................................................................... Br J Sports Med 2004;38:e20 (http://www.bjsportmed.com/cgi/content/full/38/5/e20). doi: 10.1136/bjsm.2002.004176 INVESTIGATIONS The purpose of the preparticipation examination is to identify A chest radiograph was within normal limits except for rib health conditions that might adversely affect an athlete while notching. Complete blood count, electrolytes, serum urea participating in sport. Hypertension is the most common. This nitrogen and creatinine, and thyroid stimulating hormone case report details a female basketball player found to be were within normal limits. Urinalysis showed 300 mg/l hypertensive, and complaining of fatigue, at her prepartici- protein. Electrocardiography showed sinus bradycardia with pation physical examination. Presentation, diagnostics, occasional premature atrial contractions. Echocardiography treatment, and final outcome of coarctation involving the revealed mitral valve prolapse, no mitral insufficiency, and an abdominal aorta are summarised. ejection fraction of 69%. One month after the initial presentation, an aortogram was performed. It confirmed the diagnosis of abdominal coarcta- tion, which was about 10 cm in length and 6 mm in diameter reparticipation sports physical examinations have at its greatest stenotic segment. The left renal and coeliac become routine for many institutions at the high school arteries were mildly stenotic. Internal mammary and inter- Pand collegiate level. Their main purpose is to identify costal arteries were dilated. The superior and inferior health conditions that might adversely affect an athlete while mesenteric arteries were patent, and the distal abdominal participating in a particular activity. -

Identifying COPD by Crackle Characteristics
BMJ Open Resp Res: first published as 10.1136/bmjresp-2020-000852 on 5 March 2021. Downloaded from Respiratory epidemiology Inspiratory crackles—early and late— revisited: identifying COPD by crackle characteristics Hasse Melbye ,1 Juan Carlos Aviles Solis,1 Cristina Jácome,2 Hans Pasterkamp3 To cite: Melbye H, Aviles ABSTRACT Key messages Solis JC, Jácome C, et al. Background The significance of pulmonary crackles, Inspiratory crackles— by their timing during inspiration, was described by Nath early and late—revisited: and Capel in 1974, with early crackles associated with What is the key question? identifying COPD by bronchial obstruction and late crackles with restrictive ► In the diagnosis of chronic obstructive pulmonary crackle characteristics. defects. Crackles are also described as ‘fine’ or disease (COPD), is it more useful to focus on the tim- BMJ Open Resp Res ‘coarse’. We aimed to evaluate the usefulness of crackle ing of crackles than on the crackle type? 2021;8:e000852. doi:10.1136/ bmjresp-2020-000852 characteristics in the diagnosis of chronic obstructive What is the bottom line? pulmonary disease (COPD). ► Pulmonary crackles are divided into two types, ‘fine’ Methods In a population-based study, lung sounds Received 2 December 2020 and ‘coarse’ and coarse inspiratory crackles are re- Revised 2 February 2021 were recorded at six auscultation sites and classified in garded to be typical of COPD. In bronchial obstruc- Accepted 5 February 2021 participants aged 40 years or older. Inspiratory crackles tion crackles tend to appear early in inspiration, and were classified as ‘early’ or ‘late and into the types’ this characteristic of the crackle might be easier for ‘coarse’ and ‘fine’ by two observers. -

Download Article
...& more SELF-TEST Respiratory system challenge Test your knowledge with this quick quiz. 1. Gas exchange takes place in the 8. Which continuous breath sounds are 14. Wheezes most commonly suggest a. pharynx. c. alveoli. relatively high pitched with a hissing a. secretions in large airways. b. larynx. d. trachea. or shrill quality? b. abnormal lung tissue. a. coarse crackles c. wheezes c. airless lung areas. 2. The area between the lungs is b. rhonchi d. fine crackles d. narrowed airways. known as the a. thoracic cage. c. pleura. 9. Normal breath sounds heard over 15. Which of the following indicates a b. mediastinum. d. hilum. most of both lungs are described as partial obstruction of the larynx or being trachea and demands immediate 3. Involuntary breathing is controlled by a. loud. c. very loud. attention? a. the pulmonary arterioles. b. intermediate. d. soft. a. rhonchi c. pleural rub b. the bronchioles. b. stridor d. mediastinal crunch c. the alveolar capillary network. 10. Bronchial breath sounds are d. neurons located in the medulla and normally heard 16. Which of the following would you pons. a. over most of both lungs. expect to find over the involved area b. between the scapulae. in a patient with lobar pneumonia? 4. The sternal angle is also known as c. over the manubrium. a. vesicular breath sounds the d. over the trachea in the neck. b. egophony a. suprasternal notch. c. scapula. c. decreased tactile fremitus b. xiphoid process. d. angle of Louis. 11. Which is correct about vesicular d. muffled and indistinct transmitted voice breath sounds? sounds 5. -

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -

Visual Examination
Visual Examination • Consider the impact of chest shape on the respiratory condition of the patient – Barrel chest – Kyphosis – Scoliosis – Pectus excavatum (funnel chest) – Pectus carinatum Visual Assessment of Thorax • Thoracic scars from previous surgery • Chest symmetry • Use of accessory muscles • Bruising • In drawing of ribs • Flail segment www.nejm.org/doi/full/10.1056/NEJMicm0904437 • Paradoxical breathing /seesaw breathing • Pursed lip breathing • Nasal flaring Palpation • For vibration of secretion • Surgical emphysema • Symmetry of chest movement • Tactile vocal fremitus • Check for a tracheal tug • Palpate Nodes http://www.ncbi.nlm.nih.gov/books/NBK368/ https://m.youtube.com/watch?v=uzgdaJCf0Mk Auscultation • Is there any air entry? • Differentiate – Normal vesicular sounds – Bronchial breathing – Wheeze – Distinguish crackles • Fine • Coarse • During inspiration or expiration • Profuse or scanty – Absent sounds – Vocal resonance http://www.easyauscultation.com/lung-sounds.aspx Percussion • Tapping of the middle phalanx of the left middle finger with the right middle finger • Sounds should be resonant but may be – Hyper resonant – Dull – Stony Dull http://stanfordmedicine25.stanford.edu/the25/pulmonary.html Pathological Expansion Mediastinal Percussion Breath Further Process Displacement Note Sounds Examination Consolidation Reduced on None Dull Bronchial affected side breathing Vocal resonance Whispering pectoriloquy Collapse Reduced on Towards Dull Reduced None affected side affected side Pleural Reduced on Towards Stony dull Reduced/ Occasional rub effusion affected side opposite side Absent Empyema Asthma Reduced None Resonant Normal/ Wheeze throughout Reduced COPD Reduced None Resonant/ Normal/ Wheeze throughout Hyper-resonant Reduced Pulmonary Normal or None Normal Normal Bibasal crepitations Fibrosis reduced throughout Pneumothorax Reduced on Towards Hyper-resonant Reduced/ None affected side opposite side Absent http://www.cram.com/flashcards/test/lung-sounds-886428 sign up and test yourself.. -

Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients
Age-Related Pulmonary Crackles (Rales) in Asymptomatic Cardiovascular Patients 1 Hajime Kataoka, MD ABSTRACT 2 Osamu Matsuno, MD PURPOSE The presence of age-related pulmonary crackles (rales) might interfere 1Division of Internal Medicine, with a physician’s clinical management of patients with suspected heart failure. Nishida Hospital, Oita, Japan We examined the characteristics of pulmonary crackles among patients with stage A cardiovascular disease (American College of Cardiology/American Heart 2Division of Respiratory Disease, Oita University Hospital, Oita, Japan Association heart failure staging criteria), stratifi ed by decade, because little is known about these issues in such patients at high risk for congestive heart failure who have no structural heart disease or acute heart failure symptoms. METHODS After exclusion of comorbid pulmonary and other critical diseases, 274 participants, in whom the heart was structurally (based on Doppler echocar- diography) and functionally (B-type natriuretic peptide <80 pg/mL) normal and the lung (X-ray evaluation) was normal, were eligible for the analysis. RESULTS There was a signifi cant difference in the prevalence of crackles among patients in the low (45-64 years; n = 97; 11%; 95% CI, 5%-18%), medium (65-79 years; n = 121; 34%; 95% CI, 27%-40%), and high (80-95 years; n = 56; 70%; 95% CI, 58%-82%) age-groups (P <.001). The risk for audible crackles increased approximately threefold every 10 years after 45 years of age. During a mean fol- low-up of 11 ± 2.3 months (n = 255), the short-term (≤3 months) reproducibility of crackles was 87%. The occurrence of cardiopulmonary disease during follow-up included cardiovascular disease in 5 patients and pulmonary disease in 6. -

THE DUBLIN MEDICAL SCHOOL and ITS INFLUENCE UPON MEDICINE in AMERICA1 by DAVID RIESMAN, M.D
THE DUBLIN MEDICAL SCHOOL AND ITS INFLUENCE UPON MEDICINE IN AMERICA1 By DAVID RIESMAN, M.D. PROFESSOR OF CLINICAL MEDICINE IN THE UNIVERSITY OF PENNSYLVANIA PHILADELPHIA, PA. HE Irish, a mixture of primitive universal genius like Robert Boyle, Ireland pre-Celtic peoples and of Goidelic did not produce a perpetuating body of Celts coming from the European learned men who made their influence felt T continent, developed in the early beyond the confines of the Green Island. Middle Ages, out of their own resources Of the history of Irish medicine in the and untouched in any marked degree by the Middle Ages, little is known and the all-pervading influence of Rome, a remark subject is largely an untilled field. Norman able indigenous culture. In particular they Moore (St. Barth. Hosp. Rep., 1875, it elaborated a native type of Christianity 145) has resuscitated a few of the original which with characteristic energy and manuscripts in the Irish language. Most wandering spirit they carried to Scotland, of them are translations from the works of to Northern England—to Northumbria—to Bernard de Gordon, especially from his France, to Belgium, and to Switzerland. “Lilium Medicinae”; of John of Gaddes- St. Columba, of Iona, and St. Columbanus, den’s “Rosa Anglica”; of the works of of Luxeuil, stand forth as the great militant Avicenna, of A verroes, of Isaac, and of the missionaries of that first flowering period Salernitan School. Much space is given to of Irish civilization. Although they and their the writings of Isidorus. This Isidorus is successors had to succumb to the greater the famous Spanish churchman, bishop might of Latin Christianity,2 they left of Seville, who not only was a master of dotted over Europe a number of large theology but a writer upon every branch of monasteries which became active centers of knowledge of his day. -

(Charity Hospital), As a Pathologic Rarity, One Or Two Dr
of the great deal of gas and distress, crying most ANOMALIES OF TUBERCULOSIS IN THE and six stools a day, passing green, irritating day HIGHLANDS OF COLOMBIA which, under the microscope, were seen to contain con¬ siderable fat. The mother had considerable gas in the A NEW DIAGNOSTIC SIGN IN INCIPIENT CASES bowels. The analysis showed: fat, 1.4 per cent.; lactose, 8 per cent., and protein, 1.07 per cent. JORGE VARGAS S., M.D. Although no single component was excessively high, Professor of the General Pathologic Clinic, National University of the relative proportions of the fat, lactose and protein Colombia were abnormal. In this instance after weaning, the NEW YORK a of cow's baby straightened out on simple formula of the of observed milk. Physicians early part this century a curious evolution of tuberculosis in the Colom- In another instance a was being fed by a wet- great baby bian These have an elevation of nurse who also gave her own baby the breast after Highlands. highlands about 11,800 feet above sea level, and are inhabited the foster-baby received what it needed. It was by noticed that the wetnurse's an Indo-Spanish race which numbers very few Indians although baby gained and descendants of the it was uncomfortable and a good part of the many pure conquerors. rapidly, The an of time had stools. As time went on the highlands have average temperature undigested from 14 to 16 C. 57.2 to 60.8 with an inex- fosterbaby did not receive enough milk and was given (or F.), all of the wetnurse's milk. -
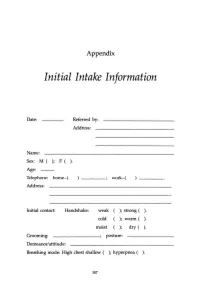
Initial Intake Information
Appendix Initial Intake Information Date: Referred by: Address: Name: Sex: M ( ); F ( ). Age: Telephone: home-( work-( Address: Initial contact: Handshake: weak ); strong ( ). cold ); warm ( ). moist ); dry ( ). Grooming: ________; posture: Demeanor/attitude: Breathing mode: High chest shallow ( ); hyperpnea ( ). 307 308 APPENDIX Sighing: frequent ( ); occasional ( ); absent ( ). Occupation: Contact with: dust ( ); fibers (); paints ( ); solvents ( ); sprays ( ); detergents ( ). Other chemicals or airborne particles: Status: Married ( ); single ( ); divorced ( ); other: children: No. Boys ( ); No. Girls ( ). Physician(s) of record: Last medical examination: _________,199__ Diagnos(e)s: 'Ireatmentts): Medication(s): Do you now have, have you ever had, or has any family member related to you by blood (mother, father, sister, brother, familial grandparents or uncles and aunts) had: ( ) High blood pressure () Heart disease APPENDIX 309 ) Low blood pressure ) Angina ) Diabetes (insulin-dependent) ) Anemia ) Diabetes (non-insulin- ) Allergies dependent) ) Dermatitis ) Colitis ) Muscle spasms ) Gastritis ) Tingling in hands and/or feet ) Ulcer ) Fainting (syncope) ) Shortness of breath ) Dizziness (vertigo) ) Asthma ) Stroke ) Emphysema ) Headache ) Hyperventilation ) TMJlbruxism ) Mitral valve prolapse ) Chronic low backache ) Other heart murmur ) EB virus (mononucl.) ) Heart arrhythmia ) PMS ) Chronic vaginal yeast ) Chronic tiredness ) Cystitis ) Menstrual irregul. ) Raynaud's disease ) Tinnitus ) Chronic pain ) Hyperthyroid ) Eating disorder -

Auscultation 4
Post-Acute COVID-19 Exercise & Rehabilitation (PACER) Project Cardiovascular and Pulmonary Examination By: Morgan Johanson, PT, MSPT, Board Certified Cardiovascular and Pulmonary Specialist Disclaimer • This course is intended for educational purposes and does not replace mentorship or consultation with more experienced cardiopulmonary colleagues. • This content is current at time of dissemination, however, realize that evidence and science on COVID19 is revolving rapidly and information is subject to change. Introduction and Disclosures • Morgan Johanson has no conflicts of interest or financial gains to disclose for this continuing education course • Course faculty: Morgan Johanson, PT, MSPT, Board Certified Cardiovascular and Pulmonary Specialist – President of Good Heart Education, a continuing education company providing live and online Cardiovascular and Pulmonary Therapy and Rehabilitation training and mentoring services for Physical Therapist studying for the ABPTS Cardiovascular and Pulmonary Specialty (CCS) Examination. – Adjunct Faculty Member, University of Toledo, Ohio – Practicing at Grand Traverse Pavilions SNF in Traverse City, MI – Professional Development Chair, CVP Section of the APTA Disclosures • Any pictures contained in the course that are not owned by Morgan Johanson were obtained via Google internet search engine and are references on the corresponding slide. Morgan Johanson does not claim ownership or rights to this material, it is being used for education purposes only and will not be reprinted or copied (so -

Johns Hopkins School of Nursing BURPS List
1 Welcome to the School of Nursing at the Johns Hopkins University! As a faculty who coordinates one of your first semester courses I am making available to you some helpful and useful information. I have included it below for your reading pleasure! There are two documents: the “B.U.R.P.S.” list (Building and Understanding Roots, Prefixes and Suffixes) and Talk like a Nurse. This document lists many (not all) of the medical terms used in your first semester classes and I believe will ease your transition into a new way of speaking. THE B.U.R.P.S LIST Purpose: To become proficient in Building and Understanding Roots, Prefixes and Suffixes Rationale: Building and understanding medical terminology is simpler when the words are broken down into roots, prefixes and suffixes. Steps: Review the B.U.R.P.S. tables and try to determine the definitions of the examples Notice the overlap among the three groups of roots, prefixes and suffixes Make new words by changing one part of the word. For example, if an appendectomy is the removal of the appendix, then a nephrectomy is the removal of a kidney. Tachycardia is a fast heart rate and tachypnea is a fast respiration rate. Helpful Note: R/T means “related to” TALK LIKE A NURSE Purpose: To become familiar with acronyms commonly used by health care providers Rationale: Different professions have unique languages; medicine and nursing are no exceptions. The acronyms below are used in verbal and written communication in health care settings. Steps: Review the attached list of acronyms (then you can start to critique shows like “House” and “Gray’s Anatomy” for accuracy!) Notice that some acronyms have two different meanings; e.g., ROM stands for “range of motion” and “rupture of membranes” - be careful when using abbreviations Take the Self Assessment after reading the approved terms, found in Blackboard NOTE: All institutions have a list of accepted and “do not use” abbreviations. -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department