Dissertation Khom Sophia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Valerenic Acid Potentiates and Inhibits GABAA Receptors: Molecular Mechanism and Subunit Specificity
ARTICLE IN PRESS + MODEL Neuropharmacology xx (2007) 1e10 www.elsevier.com/locate/neuropharm Valerenic acid potentiates and inhibits GABAA receptors: Molecular mechanism and subunit specificity S. Khom a, I. Baburin a, E. Timin a, A. Hohaus a, G. Trauner b, B. Kopp b, S. Hering a,* a Department of Pharmacology and Toxicology, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria b Department of Pharmacognosy, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria Received 8 December 2006; received in revised form 11 April 2007; accepted 30 April 2007 Abstract Valerian is a commonly used herbal medicinal product for the treatment of anxiety and insomnia. Here we report the stimulation of chloride currents through GABAA receptors (IGABA) by valerenic acid (VA), a constituent of Valerian. To analyse the molecular basis of VA action, we expressed GABAA receptors with 13 different subunit compositions in Xenopus oocytes and measured IGABA using the two-microelectrode voltage-clamp technique. We report a subtype-dependent stimulation of IGABA by VA. Only channels incorporating b2 or b3 subunits were stimulated by VA. Replacing b2/3 by b1 drastically reduced the sensitivity of the resulting GABAA channels. The stimulatory effect of VA on a1b2 receptors was substantially reduced by the point mutation b2N265S (known to inhibit loreclezole action). Mutating the corresponding residue of b1 (b1S290N) induced VA sensitivity in a1b1S290N comparable to a1b2 receptors. Modulation of IGABA was not significantly dependent on incorporation of a1, a2, a3 or a5 subunits. VA displayed a significantly lower efficiency on channels incorporating a4 subunits. IGABA modulation by VA was not g subunit dependent and not inhibited by flumazenil (1 mM). -

Plant-Based Medicines for Anxiety Disorders, Part 2: a Review of Clinical Studies with Supporting Preclinical Evidence
CNS Drugs 2013; 24 (5) Review Article Running Header: Plant-Based Anxiolytic Psychopharmacology Plant-Based Medicines for Anxiety Disorders, Part 2: A Review of Clinical Studies with Supporting Preclinical Evidence Jerome Sarris,1,2 Erica McIntyre3 and David A. Camfield2 1 Department of Psychiatry, Faculty of Medicine, University of Melbourne, Richmond, VIC, Australia 2 The Centre for Human Psychopharmacology, Swinburne University of Technology, Melbourne, VIC, Australia 3 School of Psychology, Charles Sturt University, Wagga Wagga, NSW, Australia Correspondence: Jerome Sarris, Department of Psychiatry and The Melbourne Clinic, University of Melbourne, 2 Salisbury Street, Richmond, VIC 3121, Australia. Email: [email protected], Acknowledgements Dr Jerome Sarris is funded by an Australian National Health & Medical Research Council fellowship (NHMRC funding ID 628875), in a strategic partnership with The University of Melbourne, The Centre for Human Psychopharmacology at the Swinburne University of Technology. Jerome Sarris, Erica McIntyre and David A. Camfield have no conflicts of interest that are directly relevant to the content of this article. 1 Abstract Research in the area of herbal psychopharmacology has revealed a variety of promising medicines that may provide benefit in the treatment of general anxiety and specific anxiety disorders. However, a comprehensive review of plant-based anxiolytics has been absent to date. Thus, our aim was to provide a comprehensive narrative review of plant-based medicines that have clinical and/or preclinical evidence of anxiolytic activity. We present the article in two parts. In part one, we reviewed herbal medicines for which only preclinical investigations for anxiolytic activity have been performed. In this current article (part two), we review herbal medicines for which there have been both preclinical and clinical investigations for anxiolytic activity. -
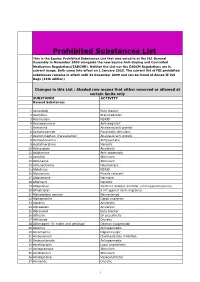
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -

Zebrafish Behavioural Profiling Identifies GABA and Serotonin
ARTICLE https://doi.org/10.1038/s41467-019-11936-w OPEN Zebrafish behavioural profiling identifies GABA and serotonin receptor ligands related to sedation and paradoxical excitation Matthew N. McCarroll1,11, Leo Gendelev1,11, Reid Kinser1, Jack Taylor 1, Giancarlo Bruni 2,3, Douglas Myers-Turnbull 1, Cole Helsell1, Amanda Carbajal4, Capria Rinaldi1, Hye Jin Kang5, Jung Ho Gong6, Jason K. Sello6, Susumu Tomita7, Randall T. Peterson2,10, Michael J. Keiser 1,8 & David Kokel1,9 1234567890():,; Anesthetics are generally associated with sedation, but some anesthetics can also increase brain and motor activity—a phenomenon known as paradoxical excitation. Previous studies have identified GABAA receptors as the primary targets of most anesthetic drugs, but how these compounds produce paradoxical excitation is poorly understood. To identify and understand such compounds, we applied a behavior-based drug profiling approach. Here, we show that a subset of central nervous system depressants cause paradoxical excitation in zebrafish. Using this behavior as a readout, we screened thousands of compounds and identified dozens of hits that caused paradoxical excitation. Many hit compounds modulated human GABAA receptors, while others appeared to modulate different neuronal targets, including the human serotonin-6 receptor. Ligands at these receptors generally decreased neuronal activity, but paradoxically increased activity in the caudal hindbrain. Together, these studies identify ligands, targets, and neurons affecting sedation and paradoxical excitation in vivo in zebrafish. 1 Institute for Neurodegenerative Diseases, University of California, San Francisco, CA 94143, USA. 2 Cardiovascular Research Center and Division of Cardiology, Department of Medicine, Massachusetts General Hospital, Harvard Medical School, Charlestown, MA 02129, USA. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

Updating the Biological Interest of Valeriana Officinalis
ARTICLES Mediterranean Botany ISSNe 2603-9109 https://dx.doi.org/10.5209/mbot.70280 Updating the biological interest of Valeriana officinalis Marta Sánchez1 , Elena González Burgos1 , Irene Iglesias1 & M. Pilar Gómez-Serranillos1 Received: 23 June 2020 / Accepted: 5 August 2020 / Published online: 11 January 2021 Abstract. Valeriana officinalis L. (Caprifoliaceae) has been traditionally used to treat mild nervous tension and sleep problems. The basis of these activities are mainly attributed to valerenic acid through the modulation of the GABA receptor. Moreover, V. officinalis is claimed to have other biological activities such as cardiovascular benefits, anticancer, antimicrobial, and spasmolytic. The current review aims to update the biological and pharmacological studies (in vitro, in vivo, and clinical trials) of V. officinalis and its major secondary metabolites to guide future research. Databases PubMed, Science Direct, and Scopus were used for literature search, including original papers written in English and published between 2014 and 2020. There have been identified 33 articles that met the inclusion criteria. Most of these works were performed withV. officinalis extracts, and only a few papers (in vitro and in vivo studies) evaluated the activity of isolated compounds (valerenic acid and volvalerenal acid K). In vitro studies focused on studying antioxidant and neuroprotective activity. In vivo studies and clinical trials mainly investigated the nervous system activity (anticonvulsant activity, antidepressant, cognitive problems, anxiety, and sleep disorders). Just a few studies were focused on other different activities, highlight effects on symptoms of premenstrual and postmenopausal syndromes. Valeriana officinaliscontinues to be one of the medicinal plants most used by today’s society for its therapeutic properties and whose biological and pharmacological activities continue to arouse great scientific interest, as evidenced in recent publications. -

Telemetry As a Tool to Measure Sedative Effects of a Valerian Root Extract and Its Single Constituents in Mice
Original Papers 795 Telemetry as a Tool to Measure Sedative Effects of a Valerian Root Extract and Its Single Constituents in Mice Authors Nicholas K. Chow1, Michael Fretz 2, Matthias Hamburger2, Veronika Butterweck1 Affiliations 1 Department of Pharmaceutics, College of Pharmacy, University of Florida, Gainesville, FL, USA 2 Institute of Pharmaceutical Biology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland Key words Abstract showed a mild short-term sedative effect with re- l" Valeriana officinalis L. ! duced locomotor activity between 66–78 min l" Valerianaceae Valeriana officinalis L. is a popular herbal treat- minutes after administration. Paradoxically, an l" linarin ment for mild sleep disorders. Clinical and non- increased activity was observed after 150 min- l" valerenic acid clinical studies found contradictory results for va- utes after gavage. A dose of 1 mg/kg valerenic acid l" apigenin l" telemetry lerian extracts and single constituents regarding produced an intermittent stimulation of activity. the influence on sleep parameters. It was the aim However, a mild short-term sedative effect was of this study to investigate the sedative effects of a found for linarin at 12 mg/kg and apigenin at valerian root extract. Therefore, locomotor activ- 1.5 mg/kg. Considering the cumulative locomotor ity and core body temperature were recorded in activity over the observation period of 180 min, it male mice using radiotelemetry. A 70% ethanolic is concluded that neither the extract nor one of extract prepared from the roots of V. officinalis the compounds had considerable sedative effects. (s.l.) and some of its single constituents, valerenic More precisely, the observed short-term changes acid, linarin, and apigenin, were tested for effects in activity pattern indicate that valerian extract on locomotion and body temperature over 180 as well as the flavonoids linarin and apigenin are minutes after oral administration. -

Root Culture of Valeriana Officinalis by Elicitation
Cent. Eur. J. Biol. • 9(9) • 2014 • 853-863 DOI: 10.2478/s11535-014-0320-3 Central European Journal of Biology Enhanced production of valerenic acid in hairy root culture of Valeriana officinalis by elicitation Research Article Mohammad Reza Dini Torkamani1, Morad Jafari2,3*, Nasser Abbaspour1, Reza Heidary1, Naser Safaie4 1Department of Biology, Faculty of Science, University of Urmia, P.O. Box 165, Urmia, Iran 2 Department of Plant Breeding and Biotechnology, Faculty of Agriculture, University of Urmia, P.O. Box 165, Urmia, Iran 3Department of Agricultural Biotechnology, Institute of Biotechnology, University of Urmia, P.O. Box 165, Urmia, Iran 4Department of Plant Pathology, Faculty of Agriculture, Tarbiat Modares University, Tehran, Iran Received 29 November 2013; Accepted 03 April 2014 Abstract: Valerenic acid (VA) is a pharmacologically-active sesquiterpene found in valerian (Valeriana officinalis L., Valerianaceae) roots and rhizomes. The plant produces only small amounts of this metabolite naturally. So, induction of hairy roots as well as elicitation can be useful to increase its commercial production. In this study, Wild-type strain ‘A13’ of Agrobacterium rhizogenes was used to induce hairy roots in valerian. The influence of three different elicitors including Fusarium graminearum extract (FE), methyl jasmonate (MJ) and salicylic acid (SA) on VA production in the selected hairy root line ‘LeVa-C4’ was also investigated. The 23-day-old cultures were treated with different concentrations of the elicitors at exposure time of 3 and 7 days. FE (1%) and MJ (100 µM L-1) highly promoted VA production at 7 days after elicitation, to a level of 12.31- and 6-fold higher than that of non-elicited controls, respectively, and FE did not exert any negative effects on biomass yield of hairy root. -

March 2017, Q2/ 2017 April – June 2017
March, 2017 Table of Contents Reference Standards Highlights USP Publication Highlights USP Education USP 40–NF 35 Find Courses New Reference Standards New Food Chemicals Codex Sign Up for USP Education Now Available (FCC) Online Platform Information Items with New Lots 2015 Dietary Supplements Previously Out-of-Stock Compendium Compendial Highlights Items Now Available USP–NF Archive New Official Text Backorder Availability Compendial Notices Estimates, March 7, 2017, Recently Released Stimuli Articles Items with New Package Size or USP 40–NF 35 Description Tip of the Month RS Lots That Are No Longer Valid Showcasing Sign up to Receive the Reference Dietary Supplements Verification Standards App Program Website Launch Question of the Month Event Highlights USP User Forums Workshops Click on Click on links to go to sections. For all the latest information, visit www.usp.org USP Catalog Reference Standards Highlights Below are several Tables with the latest Reference Standard information including out-of-stock items now available; new Reference Standards released in the last month; backordered items with estimated availability dates; items that have a new price and/or have a new package size; items with lots that are (or soon will be) no longer valid; and items with new lots since the last email notice. Please contact your USP Customer Service Representative to place an order at +1-301-881-0666 or 1-800-227-8772. European customers can call 00-800-4875-5555. You can also order online at www.usp.org/products. The Reference Standards Release Notification Service can be used to notify you when a new never-before- released Reference Standard becomes available. -

Natural Stress Reliever for High Anxiety Dogs Or Tense Situations Our Calm Supplement Is an Herbal Formulation Proven to Be As Effective As Pharmaceutical Sedatives
Calm Natural stress reliever for high anxiety dogs or tense situations Our Calm supplement is an herbal formulation proven to be as effective as pharmaceutical sedatives. Benefits include: • Natural sedative • Non-narcotic, proven effective • Can be used on its own, or as an adjunct to conventional therapies • High-grade, human-quality supplement SUPPLEMENT OVERVIEW Anxiety and phobias in dogs are relatively common; fireworks, thunderstorms, sirens, and other sudden loud noises are triggers for dogs’ keen sense of sound. Other triggers include trips to the veterinarian, separation anxiety, and disruptions in their normal routine. JFFD Calm uses a proven combination of botanical herbal remedies shown to work very similarly to prescription medications, but without the tendency to cause over-sedation or other unwanted side effects. The plants in Calm, valerian root and passionflower, work by enhancing and increasing the function of GABA receptors in the brain, allowing for a more natural calming effect.1,2 The chemistry of Passiflora incarnata (passionflower) is well documented; pharmacological effects are mediated via modulation of the GABA system including affinity to GABAA and GABAB receptors, and effects on GABA uptake. Valerian root extracts bind on GABAA receptors and enhance the brain’s response to GABA. GABA is one of the brain’s most important inhibitory (calming) neurotransmitter. SUPPLEMENT INDICATIONS JFFD Calm can be safely used daily in dogs prone to anxiety from separation or other chronic causes. Likewise, it can be used only when needed in times of high stress like those associated with noise from fireworks and thunderstorms. In these cases if the noises are anticipated ahead of time, it works best if given beginning five days before the stressful events. -

Assessment Report on Valeriana Officinalis L., Radix and Valeriana Officinalis L., Aetheroleum Final
02 February 2016 EMA/HMPC/150846/2015 Committee on Herbal Medicinal Products (HMPC) Assessment report on Valeriana officinalis L., radix and Valeriana officinalis L., aetheroleum Final Based on Article 10a of Directive 2001/83/EC as amended (well-established use) Based on Article 16d(1), Article 16f and Article 16h of Directive 2001/83/EC as amended (traditional use) Herbal substance(s) (binomial scientific Valeriana officinalis L., radix name of the plant, including plant part) Herbal preparation(s) Well-established use Dry extract (DER 3-7.4:1), extraction solvent: ethanol 40-70% (V/V) Traditional use a) Comminuted herbal substance b) Powdered herbal substance c) Expressed juice from fresh root (1:0.60-0.85) d) Dry extract (DER 4-6.1), extraction solvent: water e) Liquid extract (DER 1:4-6), extraction solvent: water f) Dry extract (DER 4-7:1), extraction solvent: methanol 45% (V/V) g) Dry extract (DER 5.3-6.6:1), extraction solvent: methanol 45% (m/m) h) Liquid extract (DER 1:7-9), extraction solvent: sweet vine i) Liquid extract (DER 1:1), extraction solvent: ethanol 60% (V/V) j) Tincture (ratio of herbal substance to extraction solvent 1:8), extraction solvent: ethanol 60% (V/V) k) Tincture (ratio of herbal substance to extraction solvent 1:10), extraction solvent: ethanol 56% l) Tincture (ratio of herbal substance to extraction solvent 1:5), extraction solvent: ethanol 70% (V/V) 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2016.