Review Search Strategy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
USOO9498481 B2 (12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao et al. (45) Date of Patent: *Nov. 22, 2016 (54) CYCLOPROPYL MODULATORS OF P2Y12 WO WO95/26325 10, 1995 RECEPTOR WO WO99/O5142 2, 1999 WO WOOO/34283 6, 2000 WO WO O1/92262 12/2001 (71) Applicant: Apharaceuticals. Inc., La WO WO O1/922.63 12/2001 olla, CA (US) WO WO 2011/O17108 2, 2011 (72) Inventors: Tadimeti Rao, San Diego, CA (US); Chengzhi Zhang, San Diego, CA (US) OTHER PUBLICATIONS Drugs of the Future 32(10), 845-853 (2007).* (73) Assignee: Auspex Pharmaceuticals, Inc., LaJolla, Tantry et al. in Expert Opin. Invest. Drugs (2007) 16(2):225-229.* CA (US) Wallentin et al. in the New England Journal of Medicine, 361 (11), 1045-1057 (2009).* (*) Notice: Subject to any disclaimer, the term of this Husted et al. in The European Heart Journal 27, 1038-1047 (2006).* patent is extended or adjusted under 35 Auspex in www.businesswire.com/news/home/20081023005201/ U.S.C. 154(b) by Od en/Auspex-Pharmaceuticals-Announces-Positive-Results-Clinical M YW- (b) by ayS. Study (published: Oct. 23, 2008).* This patent is Subject to a terminal dis- Concert In www.concertpharma. com/news/ claimer ConcertPresentsPreclinicalResultsNAMS.htm (published: Sep. 25. 2008).* Concert2 in Expert Rev. Anti Infect. Ther. 6(6), 782 (2008).* (21) Appl. No.: 14/977,056 Springthorpe et al. in Bioorganic & Medicinal Chemistry Letters 17. 6013-6018 (2007).* (22) Filed: Dec. 21, 2015 Leis et al. in Current Organic Chemistry 2, 131-144 (1998).* Angiolillo et al., Pharmacology of emerging novel platelet inhibi (65) Prior Publication Data tors, American Heart Journal, 2008, 156(2) Supp. -

Specifications of Approved Drug Compound Library
Annexure-I : Specifications of Approved drug compound library The compounds should be structurally diverse, medicinally active, and cell permeable Compounds should have rich documentation with structure, Target, Activity and IC50 should be known Compounds which are supplied should have been validated by NMR and HPLC to ensure high purity Each compound should be supplied as 10mM solution in DMSO and at least 100µl of each compound should be supplied. Compounds should be supplied in screw capped vial arranged as 96 well plate format. -

Emerging Drug List PARECOXIB SODIUM
Emerging Drug List PARECOXIB SODIUM NO. 10 MAY 2001 Generic (Trade Name): Parecoxib sodium Manufacturer: Pharmacia & Upjohn Inc. Indication: For peri-operative pain relief Current Regulatory Parecoxib is currently under review at Health Canada and the Food and Drug Status: Administration in the U.S. They are expecting approval in the fourth quarter of 2001. It is not marketed in any country at this time Description: Parecoxib is the first parenteral cyclooxygenase-2 (COX-2) selective inhibitor to be developed. It is a water-soluble prodrug that is rapidly hydrolyzed to valdecoxib (the active COX-2 inhibitor). Valdecoxib's affinity for COX-2 versus COX-1 is 90 times greater than celecoxib and 34,000 times greater than ketorolac. Once injected, peak concentrations of valdecoxib are attained in 10 to 20 minutes. Valdecoxib has a half-life of eight to 10 hours. Current Treatment: Currently, the only other nonsteroidal anti-inflammatory agent that is available as an injection is ketorolac. Ketorolac is used in some centres for peri-operative pain management, however opioids are the main class of agents used for this indication. Ketorolac has been associated with a relatively high incidence of gastrointestinal (GI) side effects, including severe cases of hemorrhage. Cost: There is no information available on the cost of parecoxib. Evidence: Parecoxib has been compared to ketorolac and morphine in clinical trials. Parecoxib at a dose of 20 and 40 mg/day IV, were compared to ketorolac, 30 mg/day IV and morphine, 4 mg/day or placebo in 202 women undergoing hysterectomy. Both doses of parecoxib were comparable to ketorolac for relieving postoperative pain. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Use of Aspirin and Nsaids to Prevent Colorectal Cancer
Evidence Synthesis Number 45 Use of Aspirin and NSAIDs to Prevent Colorectal Cancer Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-02-0021 Prepared by: University of Ottawa Evidence-based Practice Center at The University of Ottawa, Ottawa Canada David Moher, PhD Director Investigators Alaa Rostom, MD, MSc, FRCPC Catherine Dube, MD, MSc, FRCPC Gabriela Lewin, MD Alexander Tsertsvadze, MD Msc Nicholas Barrowman, PhD Catherine Code, MD, FRCPC Margaret Sampson, MILS David Moher, PhD AHRQ Publication No. 07-0596-EF-1 March 2007 This report is based on research conducted by the University of Ottawa Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-02-0021). Funding was provided by the Centers for Disease Control and Prevention. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This document is in the public domain and may be used and reprinted without permission except those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. -
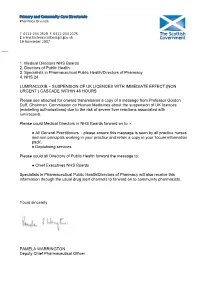
Lumiracoxib: Suspension of UK Licences with Immediate Effect (Non
Primary and Community Care Directorate Pharmacy Division T: 0131-244 2528 F: 0131-244 2375 E: [email protected] abcdefghijklmnopqrstu 19 November 2007 ___ 1. Medical Directors NHS Boards 2. Directors of Public Health 3. Specialists in Pharmaceutical Public Health/Directors of Pharmacy 4. NHS 24 LUMIRACOXIB – SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT (NON URGENT ) CASCADE WITHIN 48 HOURS Please see attached for onward transmission a copy of a message from Professor Gordon Duff, Chairman, Commission on Human Medicines about the suspension of UK licences (marketing authorisations) due to the risk of severe liver reactions associated with lumiracoxib. Please could Medical Directors in NHS Boards forward on to :- ● All General Practitioners - please ensure this message is seen by all practice nurses and non principals working in your practice and retain a copy in your ‘locum information pack’. ● Deptutising services Please could all Directors of Public Health forward the message to: ● Chief Executives NHS Boards Specialists in Pharmaceutical Public Health/Directors of Pharmacy will also receive this information through the usual drug alert channels to forward on to community pharmacists. Yours sincerely PAMELA WARRINGTON Deputy Chief Pharmaceutical Officer St Andrew’s House, Regent Road, Edinburgh EH1 3DG www.scotland.gov.uk abcde abc a Ref: EL(07)A/21 LUMIRACOXIB - SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT 19 November 2007 Dear Colleague, I am writing to inform you that the UK licences (marketing authorisations) for lumiracoxib have been suspended and stocks are being withdrawn from pharmacies, on the basis of advice from the Commission on Human Medicines (CHM). -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Studies in Laboratory Animals to Assess the Safety of Anti-Inflammatory Agents in Acute Porphyria
Ann Rheum Dis: first published as 10.1136/ard.46.7.540 on 1 July 1987. Downloaded from Annals of the Rheumatic Diseases, 1987; 46, 540-542 Studies in laboratory animals to assess the safety of anti-inflammatory agents in acute porphyria KENNETH E L McCOLL, GEORGE G THOMPSON, AND MICHAEL R MOORE From the University Department of Medicine, Western Infirmary, Glasgow SUMMARY The safety of various anti-inflammatory drugs in acute porphyria was assessed by examining their effect on rat hepatic haem synthesis. Azapropazone, chloroquine, and gold increased 6-aminolaevulinic acid (ALA) synthase activity, indicating that they are liable to precipitate porphyric crises. Aspirin, ibuprofen, indomethacin, ketoprofen, flurbiprofen, phenylbutazone, naproxen, prednisolone, and penicillamine did not increase ALA synthase activity and should be safe in porphyria. Though these animal studies can be used as a guide to prescribing in patients with acute porphyria, some caution is still required as species may vary in their response to inducing agents. Key words: chloroquine, azapropazone, gold, b-aminolaevulinic acid synthase. copyright. The acute hepatic porphyrias which comprise acute controlling enzyme of haem biosynthesis 6- intermittent porphyria, hereditary coproporphyria, aminolaevulinic acid (ALA) synthase in rat hepatic and variegate porphyria are examples of pharma- tissue. To confirm the reliability of the animal cogenetic disease. They are the result of deficien- model, phenobarbitone was also tested. For each cies of individual enzymes in the pathway of haem drug examined six male Sprague-Dawley rats re- biosynthesis and are inherited in an autosomal ceived the test drug and six control rats received the dominant fashion.2 Subjects with the genetic trait appropriate placebo solution. -

Acemetacin.Pdf
Methods and Findings in Experimental and Clinical Pharmacology 2010, 32(2): ???-??? THOMSON REUTERS Copyright © 2010 Prous Science, S.A.U. or its licensors. All rights reserved. CCC: 0379-0355/2010 DOI: 10.1358/mf.2010.32.2.1423883 ORIGINAL ARTICLE ACEMETACIN ANTINOCICEPTIVE MECHANISM IS NOT RELATED TO NO OR K+ CHANNEL PATHWAYS. M. Gil-Flores1, M.I. Ortiz2, G. Castañeda-Hernández1 and A.E. Chávez-Piña1 1Departamento de Farmacología, Centro de Investigación y de Estudios Avanzados del Instituto Politécnico Nacional, México, D.F., México. 2Área Académica de Medicina del Instituto de Ciencias de la Salud, Universidad Autónoma del Estado de Hidalgo, Pachuca, Hidalgo, México SUMMARY Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used for the treatment of acute gout and inflammation. However, its use is limited due to side effects. Acemetacin is a prodrug of indomethacin that exhibits better gastric tolerability in preclinical and clinical tri- als. The aim of this study was to examine if the systemic administration of acemetacin involved the sequential participation of nitric oxide (NO) or K+ channel pathways to confer its antinociceptive effect, as compared to indomethacin. The antinociceptive effect of both drugs was studied with the formalin test. Equimolar doses of acemetacin or indomethacin were administered orally. The intraplantar administra- tion of either L-NAME, glibenclamide, apamin or charybdotoxin plus indomethacin or acemetacin was studied using the formalin test and the anti-inflammatory and antihyperalgesic effects were measured. The antinociceptive effect of acemetacin or indomethacin was not sig- nificantly different when pretreatment with L-NAME, glibenclamide, apamin or charybdotoxin was done. The antihyperalgesic and anti- inflammatory effects were also similar for both indomethacin and acemetacin. -

Binding of Nonsteroidal Anti-Inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects
4132 Langmuir 2008, 24, 4132-4139 Binding of Nonsteroidal Anti-inflammatory Drugs to DPPC: Structure and Thermodynamic Aspects Marlene Lu´cio,*,†,⊥ Frank Bringezu,‡,|,⊥ Salette Reis,† Jose´ L. F. C. Lima,† and Gerald Brezesinski§,⊥ REQUIMTE, Faculdade de Farma´cia, UniVersidade do Porto, Rua Anı´bal Cunha, 4099-030 Porto, Portugal, Institute of Medical Physics and Biophysics, UniVersity of Leipzig, Ha¨rtelstrasse 16, D-04103 Leipzig, Germany, and Max-Planck Institute of Colloids and Interfaces, Research Campus Golm, Am Mu¨hlenberg 1, D-14476 Potsdam, Germany ReceiVed NoVember 16, 2007. In Final Form: January 8, 2008 The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on the phase transition and phase properties of 1,2-dipalmitoylphosphatidylcholine (DPPC) has been investigated in both 2D (monolayers at the air/water interface) and 3D (multilayers in lipid/water dispersions) model systems. The 2D membrane models have been characterized by means of pressure-area isotherms and grazing incidence X-ray diffraction (GIXD) measurements. Differential scanning calorimetry (DSC) and simultaneous small- and wide-angle X-ray diffraction have been applied to lipid aqueous dispersions. All NSAIDs studied altered the main transition temperature of the gel to liquid-crystalline phase transition, with the arylacetic acid derivatives (acemetacin and indomethacin) showing the largest effects. A comparison of the results reveals distinct structural features of the membrane models after interaction with the NSAID. All drugs induced perturbations in the lipid liquid-crystalline phase, suggesting a major change in the hydration behavior of DPPC. Again, the largest effects on the structural parameters are found for the arylacetic acid derivatives. The results obtained in the different model systems give indications of the role of the membrane/NSAID interactions that might also be important for NSAID gastric injury. -

The Effectiveness of Patches Containing Loxoprofen Sodium
22 Japanese Journal of Comprehensive Rehabilitation Science (2013) Original Article The effectiveness of patches containing Loxoprofen Sodium Hydrate (LX-P) in the conservative therapy of muscular back pain – Clinical results using the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) Toyoko Asami, MD, PhD,1 Naoya Yamanouchi, MD,1 Akihiko Asami, MD, PhD,2 Hisato Tanaka, MD,3 PhD, Norihiko Nogami, MD, PhD4 1Department of Rehabilitation Medicine, Saga University Hospital, Saga, Japan. 2Saga Social Insurance Hospital, Saga, Japan. 3Tanaka Hospital (Anju Medical Corporation), Saga, Japan. 4Wakakusu Ryoikuen, Tosu, Saga, Japan. ABSTRACT life disability. The rate of effectiveness of LX-P against Asami T, Yamanouchi N, Asami A, Tanaka H, Nogami pain-related disabilities in the fourth week was 62.2%. N. The effectiveness of patches containing Loxoprofen Conclusion: LX-P showed satisfactory analgesic Sodium Hydrate (LX-P) in the conservative therapy of effect and QOL improvement. We believe it is effective muscular back pain - Clinical results using the Japanese for clinical practice. Orthopaedic Association Back Pain Evaluation Keywords: loxoprofen sodium, JOABPEQ, VAS, Questionnaire (JOABPEQ). Jpn J Compr Rehabil Sci QOL, muscular back pain 2013; 4: 22-29. Objectives: We investigated the analgesic effect, Introduction degree of patient satisfaction, and QOL improvement provided by patches containing loxoprofen sodium According to the Ministry of Health, Labour and hydrate (LX-P) using a questionnaire based on the Welfare’s Comprehensive Survey of Living Conditions evaluation criteria of the Japanese Orthopaedic (several surveys conducted in fiscal 2004, 2007, 2010), Association Back Pain Evaluation Questionnaire pain in the locomotive organs, including “lower back (JOABPEQ). pain,” “stiff shoulders,” and “joint pain,” is one of the Methods: In this study of 53 patients (18 men, 35 most common subjective symptoms reported. -

Efficacy and Safety of Postoperative Intravenous Parecoxib Sodium
Open Access Protocol BMJ Open: first published as 10.1136/bmjopen-2016-011732 on 8 September 2016. Downloaded from Efficacy and safety of Postoperative Intravenous Parecoxib sodium Followed by ORal CElecoxib (PIPFORCE) post- total knee arthroplasty in patients with osteoarthritis: a study protocol for a multicentre, double-blind, parallel- group trial Qianyu Zhuang,1 Yanyan Bian,1 Wei Wang,1 Jingmei Jiang,2 Bin Feng,1 Tiezheng Sun,3 Jianhao Lin,3 Miaofeng Zhang,4 Shigui Yan,4 Bin Shen,5 Fuxing Pei,5 Xisheng Weng1 To cite: Zhuang Q, Bian Y, ABSTRACT Strengths and limitations of this study Wang W, et al. Efficacy and Introduction: Total knee arthroplasty (TKA) has been safety of Postoperative regarded as a most painful orthopaedic surgery. ▪ Intravenous Parecoxib This is the first study to investigate the efficacy Although many surgeons sequentially use parecoxib sodium Followed by ORal and safety of the sequential analgesia regimen of CElecoxib (PIPFORCE) post- and celecoxib as a routine strategy for postoperative intravenous parecoxib followed by oral celecoxib total knee arthroplasty in pain control after TKA, high quality evidence is still after total knee arthroplasty surgery. patients with osteoarthritis: a lacking to prove the effect of this sequential regimen, ▪ This study will explore the benefits of prolonged study protocol for a especially at the medium-term follow-up. The purpose sequential treatment of parecoxib and celecoxib multicentre, double-blind, of this study, therefore, is to evaluate efficacy and in medium-term function recovery. parallel-group trial. BMJ safety of postoperative intravenous parecoxib sodium ▪ The results will promote the non-steroidal Open 2016;6:e011732.