A Guide to Prenatal Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pre-Term Pre-Labour Rupture of Membranes and the Role of Amniocentesis
Fetal and Maternal Medicine Review 2010; 21:2 75–88 C Cambridge University Press 2010 doi:10.1017/S096553951000001X First published online 15 March 2010 PRE-TERM PRE-LABOUR RUPTURE OF MEMBRANES AND THE ROLE OF AMNIOCENTESIS 1,2 ANNA P KENYON, 1,2 KHALIL N ABI-NADER AND 2 PRANAV P PANDYA 1Elizabeth Garrett Anderson Institute for Women’s Health, University College London, 86-96 Chenies Mews, London WCIE 6NX. 2Fetal Medicine Unit, University College London Hospitals NHS Foundation Trust, 235 Euston Rd, London NWI 2BU. INTRODUCTION Pre-labour premature rupture of membranes (PPROM) is defined as rupture of membranes more than 1 hour prior to the onset of labour at <37 weeks gestation. PPROM occurs in approximately 3% of pregnancies and is responsible for a third of all preterm births.1 Once membranes are ruptured prolonging the pregnancy has no maternal physical advantage but fetal morbidity and mortality are improved daily at early gestations: 19% of those infants born <25 weeks develop cerebral palsy (CP) and 28% have severe motor disability.2 Those infants born extremely pre term (<28 weeks) cost the public sector £75835 (95% CI £27906–145508) per live birth3 not to mention the emotional cost to the family. To prolong gestation is therefore the suggested goal: however how and why might we delay birth in those at risk? PPROM is one scenario associated with preterm birth and here we discuss the causative mechanisms, sequelae, latency, strategies to prolong gestation (antibiotics) and consider the role of amniocentesis. We will also discuss novel therapies. PATHOPHYSIOLOGY OF MEMBRANE RUPTURE The membranes, which act to protect and isolate the fetus, are composed of two layers. -
Efficacy of Texture and Color Enhancement Imaging In
www.nature.com/scientificreports OPEN Efcacy of Texture and Color Enhancement Imaging in visualizing gastric mucosal atrophy and gastric neoplasms Tsubasa Ishikawa1, Tomoaki Matsumura1*, Kenichiro Okimoto1, Ariki Nagashima1, Wataru Shiratori1, Tatsuya Kaneko1, Hirotaka Oura1, Mamoru Tokunaga1, Naoki Akizue1, Yuki Ohta1, Keiko Saito1, Makoto Arai1,2, Jun Kato1 & Naoya Kato1 In 2020, Olympus Medical Systems Corporation introduced the Texture and Color Enhancement Imaging (TXI) as a new image-enhanced endoscopy. This study aimed to evaluate the visibility of neoplasms and mucosal atrophy in the upper gastrointestinal tract through TXI. We evaluated 72 and 60 images of 12 gastric neoplasms and 20 gastric atrophic/nonatrophic mucosa, respectively. The visibility of gastric mucosal atrophy and gastric neoplasm was assessed by six endoscopists using a previously reported visibility scale (1 = poor to 4 = excellent). Color diferences between gastric mucosal atrophy and nonatrophic mucosa and between gastric neoplasm and adjacent areas were assessed using the International Commission on Illumination L*a*b* color space system. The visibility of mucosal atrophy and gastric neoplasm was signifcantly improved in TXI mode 1 compared with that in white-light imaging (WLI) (visibility score: 3.8 ± 0.5 vs. 2.8 ± 0.9, p < 0.01 for mucosal atrophy; visibility score: 2.8 ± 1.0 vs. 2.0 ± 0.9, p < 0.01 for gastric neoplasm). Regarding gastric atrophic and nonatrophic mucosae, TXI mode 1 had a signifcantly greater color diference than WLI (color diferences: 14.2 ± 8.0 vs. 8.7 ± 4.2, respectively, p < 0.01). TXI may be a useful observation modality in the endoscopic screening of the upper gastrointestinal tract. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Prenatal Testing Options
PRENATAL TESTING OPTIONS There are many types of tests available during pregnancy. No test can detect every possible condition, however there are many tests that can provide more information. Patients may elect or decline any of these tests as they are all optional. NT Ultrasound Detailed Ultrasound SCREENING CA PNS 1st Blood Draw CA PNS 2nd Blood Draw Cell-Free DNA Screening pregnancy week 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 DIAGNOSTIC CVS Amniocentesis SCREENING TESTS Screening tests provide probabilities (odds) of having a baby with certain conditions, however screening tests cannot detect all cases of these conditions. Screening tests are performed through maternal blood and ultrasound, so there is no risk for miscarriage from these tests. Patients will receive either “screen negative” or “screen positive” results from their screening tests. When results are screen negative, these are considered low-risk for that condition, however it is not impossible that the baby has that condition. When results are screen positive, these are considered high-risk for that condition, however most women with screen positive results are carrying a healthy baby! Follow up testing is available to confirm screening results. California Prenatal Screening Program (CA PNS) (also called Sequential Integrated Screening) Combines blood draw(s) and the NT ultrasound with maternal age risk to screen for Down syndrome, trisomy 18, open neural tube defects (example: spina bifida), and Smith-Lemli-Opitz syndrome In a pregnant woman’s blood there are natural -
Chorionic Villus Sample CVS Brochure
CVS C Chorionic Villus Sampling G A A T GENETICS LABORATORIES GENETICS LABORATORIES GENETICS LABORATORIES 3/2015 ou are being asked to consider prena- tal diagnosis in your current pregnancy. Y Chorionic villus sampling (CVS) is available as a method of prenatal testing for women who are less than 13 weeks pregnant. This test can be performed earlier than amniocentesis, which is usually performed between 15 and 20 weeks, thereby offering results earlier in the pregnancy. This brochure is to provide you with some basic information on CVS. A separate brochure is avail- able which describes amniocentesis. Who should consider CVS? CVS should be considered by women age 35 or older at the time of delivery, individuals who have had a child with a chromosome abnormality, individuals who have a chromosome translocation, and couples at risk for a prenatally diagnosable genetic disease (e.g., hemophilia or sickle cell disease). CVS is not appropriate for individuals with a family history of neural tube defects (spina bifida or anencephaly). When is CVS performed? CVS is traditionally performed between 10 - 13 weeks after a woman’s last menstrual period (during the first trimester). How is CVS performed? There are two methods for obtaining chorionic villi. For many women, either method can be safely per- formed. First, an ultrasound evaluation is performed to locate the developing placenta and to date the pregnancy. Often, the placental location determines which method of CVS is more appropriate. There are certain other obstetrical considerations which may make one method preferable, including uterine anatomy and vaginal infections. TRANSCERVICAL CVS: A thin catheter (hollow tube) is inserted into the vagina and through the cervix. -
Spinal Muscular Atrophy Testing
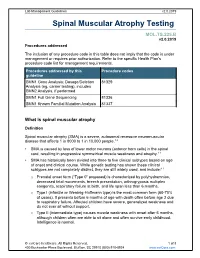
Lab Management Guidelines v2.0.2019 Spinal Muscular Atrophy Testing MOL.TS.225.B v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline SMN1 Gene Analysis; Dosage/Deletion 81329 Analysis (eg, carrier testing), includes SMN2 Analysis, if performed SMN1 Full Gene Sequencing 81336 SMN1 Known Familial Mutation Analysis 81337 What is spinal muscular atrophy Definition Spinal muscular atrophy (SMA) is a severe, autosomal recessive neuromuscular disease that affects 1 in 8000 to 1 in 10,000 people.1,2 SMA is caused by loss of lower motor neurons (anterior horn cells) in the spinal cord, resulting in progressive symmetrical muscle weakness and atrophy.1-3 SMA has historically been divided into three to five clinical subtypes based on age of onset and clinical course. While genetic testing has shown these clinical subtypes are not completely distinct, they are still widely used, and include:1-3 o Prenatal onset form (“Type 0” proposed) is characterized by polyhydramnios, decreased fetal movements, breech presentation, arthrogryposis multiplex congenita, respiratory failure at birth, and life span less than 6 months. o Type I (infantile or Werdnig-Hoffmann type) is the most common form (60-70% of cases). It presents before 6 months of age with death often before age 2 due to respiratory failure. Affected children have severe, generalized weakness and do not ever sit without support. -

Evolution of Oviductal Gestation in Amphibians MARVALEE H
THE JOURNAL OF EXPERIMENTAL ZOOLOGY 266394-413 (1993) Evolution of Oviductal Gestation in Amphibians MARVALEE H. WAKE Department of Integrative Biology and Museum of Vertebrate Zoology, University of California,Berkeley, California 94720 ABSTRACT Oviductal retention of developing embryos, with provision for maternal nutrition after yolk is exhausted (viviparity) and maintenance through metamorphosis, has evolved indepen- dently in each of the three living orders of amphibians, the Anura (frogs and toads), the Urodela (salamanders and newts), and the Gymnophiona (caecilians). In anurans and urodeles obligate vivi- parity is very rare (less than 1%of species); a few additional species retain the developing young, but nutrition is yolk-dependent (ovoviviparity) and, at least in salamanders, the young may be born be- fore metamorphosis is complete. However, in caecilians probably the majority of the approximately 170 species are viviparous, and none are ovoviviparous. All of the amphibians that retain their young oviductally practice internal fertilization; the mechanism is cloaca1 apposition in frogs, spermato- phore reception in salamanders, and intromission in caecilians. Internal fertilization is a necessary but not sufficient exaptation (sensu Gould and Vrba: Paleobiology 8:4-15, ’82) for viviparity. The sala- manders and all but one of the frogs that are oviductal developers live at high altitudes and are subject to rigorous climatic variables; hence, it has been suggested that cold might be a “selection pressure” for the evolution of egg retention. However, one frog and all the live-bearing caecilians are tropical low to middle elevation inhabitants, so factors other than cold are implicated in the evolu- tion of live-bearing. -

Management of Neonates Born at ≤34 6/7 Weeks' Gestation with Suspected Or Proven Early-Onset Bacterial Sepsis Karen M
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care ≤ ’ Management of Neonates Born at 34 Karen M. Puopolo, MD, PhD, FAAP, a, b William E. Benitz, MD, FAAP, c Theoklis E. Zaoutis, MD, MSCE, FAAP, a, d 6/7COMMITTEE ONWeeks FETUS AND NEWBORN, GestationCOMMITTEE ON INFECTIOUS DISEASES With Suspected or Proven Early-Onset Bacterial Sepsis Early-onset sepsis (EOS) remains a serious and often fatal illness among abstract infants born preterm, particularly among newborn infants of the lowest gestational age. Currently, most preterm infants with very low birth weight are treated empirically with antibiotics for risk of EOS, often for prolonged aDepartment of Pediatrics, Perelman School of Medicine, University periods, in the absence of a culture-confirmed infection. Retrospective of Pennsylvania, Philadelphia, Pennsylvania; bChildren’s Hospital of studies have revealed that antibiotic exposures after birth are associated Philadelphia, and dRoberts Center for Pediatric Research, Philadelphia, Pennsylvania; and cDivision of Neonatal and Developmental Medicine, with multiple subsequent poor outcomes among preterm infants, making the Department of Pediatrics, School of Medicine, Stanford University, Palo risk/benefit balance of these antibiotic treatments uncertain. Gestational Alto, California age is the strongest single predictor of EOS, and the majority of preterm This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have births occur in the setting of other factors associated with risk of EOS, filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process making it difficult to apply risk stratification strategies to preterm infants. -

Prenatal and Preimplantation Genetic Diagnosis for Mps and Related Diseases
PRENATAL AND PREIMPLANTATION GENETIC DIAGNOSIS FOR MPS AND RELATED DISEASES Donna Bernstein, MS Amy Fisher, MS Joyce Fox, MD Families who are concerned about passing on genetic conditions to their children have several options. Two of those options are using prenatal diagnosis and preimplantation genetic diagnosis. Prenatal diagnosis is a method of testing a pregnancy to learn if it is affected with a genetic condition. Preimplantation genetic diagnosis, also called PGD, is a newer technology used to test a fertilized embryo before a pregnancy is established, utilizing in vitro fertilization (IVF). Both methods provide additional reproductive options to parents who are concerned about having a child with a genetic condition. There are two types of prenatal diagnosis; one is called amniocentesis, and the other is called CVS (chorionic villus sampling). Amniocentesis is usually performed between the fifteenth and eighteenth weeks of pregnancy. Amniocentesis involves inserting a fine needle into the uterus through the mother's abdomen and extracting a few tablespoons of amniotic fluid. Skin cells from the fetus are found in the amniotic fluid. These cells contain DNA, which can be tested to see if the fetus carries the same alterations in the genes (called mutations) that cause a genetic condition in an affected family member. If the specific mutation in the affected individual is unknown, it is possible to test the enzyme activity in the cells of the fetus. Although these methods are effective at determining whether a pregnancy is affected or not, they do not generally give information regarding the severity or the course of the condition. -

Prenatal Screening Tests: Options for Women 35 Or Older
Women who will be 35 or older on their due date are at higher risk for a group of birth defects called chromosome disorders. A screening test can give you more information about your chance to have a Prenatal Screening Tests baby with this type of birth defect. If you want a Options for women screening test during pregnancy, you can decide 35 or older which one seems right for you. How risk There are two main screening tests that look for birth defects: "State changes with age screening" and "NIPT". Either test can indicate if your pregnancy has a high or low chance for the baby to have a common chromosome disorder. Most Chance for Down syndrome pregnancies with Down syndrome and trisomy 18 can be found by starting with a screening test; however, screening tests occasionally miss these 25 year old 1 in 1250 30 year old 1 in 900 conditions. 35 year old 1 in 365 For women who will be 35 or older: 40 year old 1 in 100 • State screening detects 91-94% of babies with Down syndrome and trisomy 18 45 year old 1 in 30 • NIPT detects 98-99% of babies with Down syndrome and trisomy 18 State Screening NIPT State Screening is a more general test for birth NIPT is a more targeted screening test that looks for defects. This test estimates the risk for Down common chromosome disorders. This test estimates syndrome and trisomy 18, and can help find the risk for Down syndrome, trisomy 18, trisomy 13 pregnancies with certain physical birth defects. -

Short Course 10 Metaplasia in The
0 3: 436-446 Rev Esp Patot 1999; Vol. 32, N © Prous Science, SA. © Sociedad Espajiola de Anatomia Patot6gica Short Course 10 © Sociedad Espafiola de Citologia Metaplasia in the gut Chairperson: NA. Wright, UK. Co-chairpersons: G. Coggi, Italy and C. Cuvelier, Belgium. Overview of gastrointestinal metaplasias only in esophagus but also in the duodenum, intestine, gallbladder and even in the pancreas. Well established is columnar metaplasia J. Stachura of esophageal squamous epithelium. Its association with increased risk of esophageal cancer is widely recognized. Recent develop- Dept. of Pathomorphology, Jagiellonian University ments have suggested, however, that only the intestinal type of Faculty of Medicine, Krakdw, Poland. metaplastic epithelium (classic Barrett’s esophagus) predisposes to cancer. Another field of studies is metaplasia in the short seg- ment at the esophago-cardiac junction, its association with Metaplasia is a reversible change in which one aduit cell type is Helicobacter pylon infection and/or reflux disease and intestinal replaced by another. It is always associated with some abnormal metaplasia in the cardiac and fundic areas. stimulation of tissue growth, tissue regeneration or excessive hor- Studies on gastric mucosa metaplasia could be divided into monal stimulation. Heterotopia, on the other hand, takes place dur- those concerned with pathogenesis and detailed structural/func- ing embryogenesis and is usually supposed not to be associated tional features and those concerned with clinical significance. with tissue damage. Pancreatic acinar cell clusters in pediatric gas- We know now that gastric mucosa may show not only complete tric mucosa form another example of aberrant cell differentiation. and incomplete intestinal metaplasia but also others such as ciliary Metaplasia is usually divided into epithelial and connective tis- and pancreatic metaplasia. -

Hyperplasia (Growth Factors
Adaptations Robbins Basic Pathology Robbins Basic Pathology Robbins Basic Pathology Coagulation Robbins Basic Pathology Robbins Basic Pathology Homeostasis • Maintenance of a steady state Adaptations • Reversible functional and structural responses to physiologic stress and some pathogenic stimuli • New altered “steady state” is achieved Adaptive responses • Hypertrophy • Altered demand (muscle . hyper = above, more activity) . trophe = nourishment, food • Altered stimulation • Hyperplasia (growth factors, . plastein = (v.) to form, to shape; hormones) (n.) growth, development • Altered nutrition • Dysplasia (including gas exchange) . dys = bad or disordered • Metaplasia . meta = change or beyond • Hypoplasia . hypo = below, less • Atrophy, Aplasia, Agenesis . a = without . nourishment, form, begining Robbins Basic Pathology Cell death, the end result of progressive cell injury, is one of the most crucial events in the evolution of disease in any tissue or organ. It results from diverse causes, including ischemia (reduced blood flow), infection, and toxins. Cell death is also a normal and essential process in embryogenesis, the development of organs, and the maintenance of homeostasis. Two principal pathways of cell death, necrosis and apoptosis. Nutrient deprivation triggers an adaptive cellular response called autophagy that may also culminate in cell death. Adaptations • Hypertrophy • Hyperplasia • Atrophy • Metaplasia HYPERTROPHY Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ No new cells, just larger cells. The increased size of the cells is due to the synthesis of more structural components of the cells usually proteins. Cells capable of division may respond to stress by undergoing both hyperrtophy and hyperplasia Non-dividing cell increased tissue mass is due to hypertrophy.