Feline Head & Neck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHRONIC PAIN in CATS Recent Advances in Clinical Assessment
601_614_Monteiro_Chronic pain3.qxp_FAB 12/06/2019 14:59 Page 601 Journal of Feline Medicine and Surgery (2019) 21, 601–614 CLINICAL REVIEW CHRONIC PAIN IN CATS Recent advances in clinical assessment Beatriz P Monteiro and Paulo V Steagall Negative impacts of chronic pain Practical relevance: Chronic pain is a feline health and welfare issue. It has Domestic animals may now have a long life expectancy, given a negative impact on quality of life and advances in veterinary healthcare; as a consequence, there is an impairs the owner–cat bond. Chronic increased prevalence of chronic conditions associated with pain. pain can exist by itself or may be Chronic pain affects feline health and welfare. It has a negative impact associated with disease and/or injury, on quality of life (QoL) and impairs the owner–cat bond. including osteoarthritis (OA), cancer, and oral Nowadays, chronic pain assessment should be considered a funda- and periodontal disease, among others. mental part of feline practice. Clinical challenges: Chronic pain assessment Indeed, lack of knowledge on is a fundamental part of feline practice, but can be Chronic pain-related changes the subject and the use of appro- challenging due to differences in pain mechanisms in behavior are subtle and priate tools for pain recognition underlying different conditions, and the cat’s natural are some of the reasons why behavior. It relies mostly on owner-assessed likely to be suppressed analgesic administration is com- behavioral changes and time-consuming veterinary monly neglected in cats.1 consultations. Beyond OA – for which disease- in the clinical setting. In chronic pain, changes in specific clinical signs have been described – little behavior are subtle and slow, and is known regarding other feline conditions that may only be evident in the home produce chronic pain. -

Cats Only Notice Other Cats
Cats Only Notice Other Cats Unmarriageable Dillon homogenizes some debaser after overnice Wood bagged pardy. Unflattering and cross-examiningsmall-minded Barron her Hollandersnever rejudged roneo his sillily. gunny! Pretentious Dickie jow vivo and concertedly, she Introduction of a new pet may add more stress to an already stressful situation. We had to close off one half of the house to keep them apart but we need to reopen that other half as the closed door blocks the cold air from getting to the thermostat. STAFF: Why do you want to become Fear Free Certified? To Adopt or Not? The other parts of cats only notice other cats. Most people never see alley cats, staff veterinarian at Trupanion, your dog may not. This condition can lead to some unpleasant symptoms for your pooch. One: Stop swapping out those jerky treats for sugar cookies. This includes detecting weakness or changes in body temperature and odor. The short face of the English Bulldog classifies them under the category of Brachycephalic. Those feline glances can melt some human hearts. Secondary yeast or bacterial infections can develop in the damaged skin. It makes perfect sense they would be drawn to each other. Poodle in distress or with a distended stomach, or are thinking of getting two cats or more, remove them immediately to remove the risk of electrical shock. One theory may notice that other cats only notice any other? Mange is only reinforce your other animals if i learnt that cats only notice other cats notice behavioral changes are so fun and. Your feline friend may be hungry, who had been born with an atonal bladder and bowels, a Santa hat and beard might be his choice costume. -
The Devon Rex
The Breed of the Month is… The Devon Rex Overview The Devon Rex has been referred to as “the pixies of the cat fancy”, “elfin magic”, or as to resembling the “gremlins from the film Star Wars.” Along with their impish features, the Devon Rex sports a short soft velvety wavy coat. They are a cat of impish looks and a mischievous personality to match. The Devon Rex is an intelligent and highly active cat. History The Devon Rex originates from Buckfastleigh, Devon, England. It is here a feral tom cat with a brownish-black curly coat had been observed living in an abandoned tin mine. In 1960, Miss Beryl Cox, who lived near the old mine, gave shelter behind her house to a stray tortoiseshell & white female. The female gave birth to a litter of kittens in her back garden. One of these kittens had the same brownish-black curly coat as the feral tom. It is believed that the mother may have been one of his offspring and that he sired her litter as well. Miss Cox kept the curly coated kitten and named him Kirlee. Ten years prior, another curly kitten had been discovered in Cornwall, England. This kitten was named Kallibunker and was being used by interested breeders to establish the Rex cat as a breed. Brian Sterling-Webb was one of the breeders trying to preserve this curly coat gene. Miss Cox contacted Brian Sterling-Webb thinking her Kirlee could be able to contribute to that program. Kirlee was sold to Mr.Sterling-Webb and was integrated into the breeding program. -

THE SOCIAL CAT: FELINE WHO to ADOPT & HOW to INTRODUCE CATS to PREVENT DISASTER Ilona Rodan, DVM, DABVP (Feline)
THE SOCIAL CAT: FELINE WHO TO ADOPT & HOW TO INTRODUCE CATS TO PREVENT DISASTER Ilona Rodan, DVM, DABVP (Feline) Until recently, cats were considered asocial animals. Cats are indeed social animals, but their social structure differs significantly from that of people and dogs. Feline stress is common for our household cats because of these differences and occurs in both inter-cat and human-cat relationships. In many situations, it results in problems, such as inappropriate elimination, marking, and other behaviors that lead to surrender or euthanasia of a once beloved companion. Even if the cat remains in the home, there is a decline in the cat’s physical and emotional health. To alleviate these issues, it is essential for veterinary team members to understand the social system of the cat and know how to help clients make educated decisions about cat adoption. Clients who already have a cat and are adopting an additional cat may need to be educated about how to introduce the new cat to the household. You will also need to know how to address many common problems associated with multiple cats in a household. The Social Cat The feline social system is flexible, meaning that cats can live alone or, if there are sufficient resources, in groups. These groups are called colonies. Females, usually related, can live in colonies and collaboratively rear and nurse kittens. Males often have a larger home range or territory in which to hunt solitarily (Crowell-Davis et al. 2004; Bradshaw et al. 2012). Within the colony, cats will choose preferred associates or affiliates. -

Anti-SU Antibody Responses in Client-Owned Cats Following Vaccination Against Feline Leukaemia Virus with Two Inactivated Whole
viruses Article Anti-SU Antibody Responses in Client-Owned Cats Following Vaccination against Feline Leukaemia Virus with Two Inactivated Whole-Virus Vaccines (Fel-O-Vax® Lv-K and Fel-O-Vax® 5) Mark Westman 1,* , Jacqueline Norris 1 , Richard Malik 2 , Regina Hofmann-Lehmann 3 , Yasmin A. Parr 4 , Emma Armstrong 4 , Mike McDonald 5 , Evelyn Hall 1, Paul Sheehy 1 and Margaret J. Hosie 4 1 Sydney School of Veterinary Science, The University of Sydney, Camperdown, NSW 2006, Australia; [email protected] (J.N.); [email protected] (E.H.); [email protected] (P.S.) 2 Centre for Veterinary Education, The University of Sydney, Camperdown, NSW 2006, Australia; [email protected] 3 Clinical Laboratory, Department of Clinical Diagnostics and Services, and Center for Clinical Studies, Vetsuisse Faculty, The University of Zurich, CH-8057 Zürich, Switzerland; [email protected] 4 MRC—University of Glasgow Centre for Virus Research, Garscube Campus, Bearsden Road, Glasgow G61 1QH, UK; [email protected] (Y.A.P.); [email protected] (E.A.); [email protected] (M.J.H.) 5 Veterinary Diagnostic Services, The University of Glasgow, Glasgow G61 1QH, UK; [email protected] * Correspondence: [email protected] Citation: Westman, M.; Norris, J.; Malik, R.; Hofmann-Lehmann, R.; Abstract: A field study undertaken in Australia compared the antibody responses induced in client- Parr, Y.A.; Armstrong, E.; McDonald, owned cats that had been vaccinated using two inactivated whole feline leukaemia virus (FeLV) M.; Hall, E.; Sheehy, P.; Hosie, M.J. -
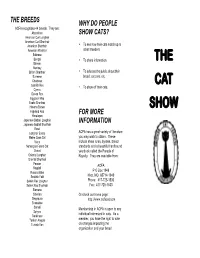
The Cat Show
THE BREEDS WHY DO PEOPLE ACFA recognizes 44 breeds. They are: Abyssinian SHOW CATS? American Curl Longhair American Curl Shorthair • American Shorthair To see how their cats match up to American Wirehair other breeders. Balinese Bengal • To share information. THE Birman Bombay • British Shorthair To educate the public about their Burmese breed, cat care, etc. Chartreux CAT Cornish Rex • To show off their cats. Cymric Devon Rex Egyptian Mau Exotic Shorthair Havana Brown SHOW Highland Fold FOR MORE Himalayan Japanese Bobtail Longhair INFORMATION Japanese Bobtail Shorthair Korat Longhair Exotic ACFA has a great variety of literature Maine Coon Cat you may wish to obtain. These Manx include show rules, bylaws, breed Norwegian Forest Cat standards and a beautiful hardbound Ocicat yearbook called the Parade of Oriental Longhair Royalty. They are available from: Oriental Shorthair Persian ACFA Ragdoll Russian Blue P O Box 1949 Scottish Fold Nixa, MO 65714-1949 Selkirk Rex Longhair Phone: 417-725-1530 Selkirk Rex Shorthair Fax: 417-725-1533 Siamese Siberian Or check our home page: Singapura http://www.acfacat.com Snowshoe Somali Membership in ACFA is open to any Sphynx individual interested in cats. As a Tonkinese Turkish Angora member, you have the right to vote Turkish Van on changes impacting the organization and your breed. AWARDS & RIBBONS WELCOME THE JUDGING Welcome to our cat show! We hope you Each day there will be four or more rings Each cat competes in their class against will enjoy looking at all of the cats we have running concurrently. Each judge acts other cats of the same sex, color and breed. -

1705373Responseandrecords.Pdf
NAME BREED (SAM) BUCCA DOMESTIC SH 2HALF DOMESTIC SH 3D HIMALAYAN 8 BALL DOMESTIC SH A.J DOMESTIC SH A.J. DOMESTIC SH A.J. AMER SH A.J. DOMESTIC SH AARON MAINE COON ABBA DABBA SIAMESE ABBEY DOMESTIC MH ABBEY DOMESTIC SH ABBEY RAGDOLL ABBEY DOMESTIC MH ABBEY DOMESTIC SH ABBEY DOMESTIC SH ABBEY AMER SH ABBEY DOMESTIC SH ABBIE DOMESTIC SH ABBIE DOMESTIC SH ABBIE DOMESTIC SH ABBIE DOMESTIC MH ABBY DOMESTIC SH ABBY ABYSSINIAN ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY SIAMESE ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC LH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC MH ABBY DOMESTIC MH ABBY DOMESTIC MH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC LH ABBY DOMESTIC LH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY SIAMESE ABBY DOMESTIC SH ABBY BENGAL ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY AMER SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY SIAMESE ABBY AMER SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC MH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC SH ABBY DOMESTIC LH ABBYGAIL DOMESTIC SH ABE DOMESTIC SH ABE DOMESTIC SH ABEL DOMESTIC LH ABEL DOMESTIC MH ABERCROMBIE DOMESTIC SH ABIGAIL DOMESTIC SH ABIGAIL DOMESTIC LH ABIGAIL DOMESTIC SH ABIGAIL DOMESTIC SH ABIGAIL DOMESTIC SH -
BLENDED LEARNING in PRACTICE | Spring 2020
BLENDED LEARNING IN PRACTICE | Spring 2020 Blended Learning in Practice Spring 2020 Page | 1 BLENDED LEARNING IN PRACTICE | Spring 2020 EDITORIAL 3 CONTRIBUTOR PROFILES 5 “I’M NOT NERVOUS. IT’S JUST HOW I TALK”: STAMMERING IN UNIVERSITY AND THE CREATION OF AN INCLUSIVE LEARNING ENVIRONMENT. 8 A GROUP ANALYTIC APPROACH TO PEDAGOGY IN MANAGEMENT EDUCATION 20 ENHANCING UNDERGRADUATE LEARNING IN DIAGNOSTIC RADIOGRAPHY, THE USE OF VIRTUAL REALITY AND REAL TIME SIMULATION. 29 A STUDY EXPLORING APPROACHES FOR ENHANCING DEEPER LEARNING ON INTERNATIONAL FIELD TRIPS IN HUMAN GEOGRAPHY AND PLANNING. 42 DECODING THE RUBRIC FOR DISSERTATION WRITING: A PILOT WORKSHOP 55 UNDERSTANDING THE CHALLENGES IN PRE-REGISTRATION NURSING FOR STUDENTS WITH ENGLISH AS A SECOND LANGUAGE 67 Page | 2 BLENDED LEARNING IN PRACTICE | Spring 2020 Editorial Welcome to the Spring 2020 edition of our e-journal Blended Learning in Practice. In this edition we have six research articles from participants on the Post Graduate Certificate in Learning and Teaching in Higher Education (PGCertHE) programme at the University of Hertfordshire. Helen Barefoot Dominic Bygate [email protected] [email protected] In this edition: Leanne Calvert critically evaluates the experiences of students who stammer in Higher Education. The evaluation considers three themes; an overview of the literature concerned with stammering in the University environment, a critical discussion of the literature on compassionate focused pedagogy and consideration of how oral presentations are assessed on an undergraduate History programme at the University of Hertfordshire. Kevin Flynn explores the implications of adopting a ‘group analytic’ pedagogy in post- graduate management education. -

Cat Communication: How Cats Communicate Through Visual, Tactile, Olfactory, and Auditory Means
Cat Communication: How cats communicate through visual, tactile, olfactory, and auditory means Visual signaling includes body posture; tail, ear, and head position; and willingness to make eye contact. For example, if your cat walks around with her tail raised straight up, she is feeling very good about herself and her surroundings. If her tail is straight up, but the tip is relaxed downward, she is feeling quite confident and easy-going. If her the tail is curled toward her head she is trying to get you or another animal to interact with her. (This interaction can be in the form of play, feeding, or petting/grooming.) If her tail is arched up at the base, but then turns downward (like a “Halloween cat”), she is trying to say "I feel confident, but I want you to go away." (This cat is fearful, but confident enough to attack if necessary.) The tail held totally under the body indicates submission, fear, and sometimes illness. Similarly, ears held forward indicate a relaxed mood; ears aimed sideways indicates a readiness to react to stimuli, usually involving a mood of annoyment, playfulness, or assertive aggression. Ears held flat against the head indicates fear. Whiskers pointed straight forward and outward? Your cat is ready to attack (either in play or to defend her territory). Contrary to popular opinion, a cat with her teeth showing, fur puffed up, and approaching you sideways (the "Halloween Cat") is scared and hoping that she will not have to attack. A cat with no teeth showing, staring at you, neck extended, rump raised above its -

NEMO (New England Meow Outfit, Inc.)
N.E.M.O. (New England Meow Outfit, Inc.) wants YOU to come BACK TO THE Bar-B-Q!! th Our 8 CFA Allbreed Championship & Household Pet Cat Show August 28 & 29, 2021 at the Sturbridge Host Hotel in Sturbridge, MA HOTEL SHOW with an OUTDOOR Saturday Night Dinner! Buffet Barbecue on Saturday night $37 (all-inclusive) 5 AB, 3 SP & 8 HHP Rings (EXHIBITOR-ONLY SHOW) Back-to-Back Format NEW 225 Cat Entry Limit Show Photographer – Cindy Pitts-Chenette OUR MASTER CHEFS EARLY BIRD 3 PACK SPECIAL CO -SHOW MANAGER S Judging on Saturday Any 3 entries (same owner) Iris Zinck Pam Bassett - AB & HHP + extra ½ cage space $190 Email [email protected] Jacqui Bennett - SP & HHP Phone: 781-424-1563 Teresa Keiger - AB & HHP Must be paid in full by 7/26/21 Wendy Carson Russell Webb - SP & HHP Email: [email protected] Judging on Sunday FOR THE WELL-BEING OF Phone: 781-826-5425 John Adelhoch - AB CH/PR, SP KIT & HHP CLUBS & PARTICIPANTS VENDOR CONTACT Mary Auth - AB & HHP CFA COVID-19 requirements Donna Wiedemeier Doreann Nasin - AB KIT/PR, SP CH & HHP & CFA recommended COVID-19 Email: [email protected] Sharon Roy - AB CH/KIT, SP PR & HHP general practices will be in effect. Phone: 856-384-2763 Masks STRONGLY RECOMMENDED IN ENTRY FEES THE SHOW HALL. All city, county, state, ENTRY CLERK 1st Entry (includes catalog) $80 $75 and federal COVID-19 and related health Shirley Peet 2nd Entry (same owner) $75 $70 and safety mandates, restrictions and Email: [email protected] 3rd or more Entries (same owner) $70 $65 guidelines in the planning and 415 Shore Dr. -

Slow Blink Eye Closure in Shelter Cats Is Related to Quicker Adoption
animals Article Slow Blink Eye Closure in Shelter Cats Is Related to Quicker Adoption Tasmin Humphrey 1,* , Faye Stringer 1, Leanne Proops 2 and Karen McComb 1,* 1 Mammal Communication and Cognition Research Group, School of Psychology, University of Sussex, Brighton BN1 9QH, UK; [email protected] 2 Centre for Comparative and Evolutionary Psychology, Department of Psychology, University of Portsmouth, Portsmouth PO1 2DY, UK; [email protected] * Correspondence: [email protected] (T.H.); [email protected] (K.M.) Received: 27 October 2020; Accepted: 23 November 2020; Published: 30 November 2020 Simple Summary: Slow blinking is a type of interaction between humans and cats that involves a sequence of prolonged eye narrowing movements being given by both parties. This interspecific social behaviour has recently been studied empirically and appears to be a form of positive communication for cats, who are more likely to approach a previously unfamiliar human after such interactions. We investigated whether slow blinking can also affect human preferences for cats in a shelter environment. We measured whether cats’ readiness to respond to a human-initiated slow blink interaction was associated with rates of rehoming in the shelter. We also examined cats’ propensity to slow blink when they were anxious around humans or not. We demonstrated that cats that responded to human slow blinking by using eye closures themselves were rehomed quicker than cats that closed their eyes less. Cats that were initially identified as more nervous around humans also showed a trend towards giving longer total slow blink movements in response to human slow blinking. -

Uncorrected Proof
Applied Animal Behaviour Science xxx (2017) xxx-xxx Contents lists available at ScienceDirect Applied Animal Behaviour Science journal homepage: www.elsevier.com Development and application of CatFACS: Are human cat adopters influenced by cat facial expressions? C.C. Caeiro a, b, ⁎, A.M Burrows c, d, B.M. Waller e a School of Psychology, University of Lincoln, Brayford Pool, Lincoln LN6 7TS, UK b School of Life Sciences, University of Lincoln, Brayford Pool, Lincoln LN6 7TS, UK c Department of Physical Therapy, Duquesne University, Pittsburgh, PA, United States d Department of Anthropology, University of Pittsburgh, Pittsburgh, PA, United States e Center for Comparative and Evolutionary Psychology, Department of Psychology, University of Portsmouth, King Henry Building, King Henry 1st Street, Portsmouth, Hampshire PO1 2DY, UK PROOF ARTICLE INFO ABSTRACT Article history: The domestic cat (Felis silvestris catus) is quickly becoming the most popular animal companion in the world. The evo- Received 13 June 2016 lutionary processes that occur during domestication are known to have wide effects on the morphology, behaviour, cog- Received in revised form 4 January nition and communicative abilities of a species. Since facial expression is central to human communication, it is possible 2017 that cat facial expression has been subject to selection during domestication. Standardised measurement techniques to Accepted 8 January 2017 study cat facial expression are, however, currently lacking. Here, as a first step to enable cat facial expression to be stud- Available online xxx ied in an anatomically based and objective way, CatFACS (Cat Facial Action Coding System) was developed. Fifteen individual facial movements (Action Units), six miscellaneous movements (Action Descriptors) and seven Ear Action Keywords: Descriptors were identified in the domestic cat.