Fibroepithelial and Spindle Cell Lesions of the Breast
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uterine Sarcomas: a Review
ARTICLE IN PRESS YGYNO-973334; No. of pages: 9; 4C: 3, 6 Gynecologic Oncology xxx (2009) xxx–xxx Contents lists available at ScienceDirect Gynecologic Oncology journal homepage: www.elsevier.com/locate/ygyno Review Uterine sarcomas: A review Emanuela D'Angelo, Jaime Prat ⁎ Department of Pathology, Hospital de la Santa Creu i Sant Pau, Autonomous University of Barcelona, Sant Antoni M. Claret, 167, 08025 Barcelona, Spain article info abstract Article history: Objective. Uterine sarcomas are rare tumors that account for 3% of uterine cancers. Their histopathologic Received 29 June 2009 classification was revised by the World Health Organization (WHO) in 2003. A new staging system has been Available online xxxx recently designed by the International Federation of Gynecology and Obstetrics (FIGO). Currently, there is no consensus on risk factors for adverse outcome. This review summarizes the available clinicopathological data Keywords: on uterine sarcomas classified by the WHO diagnostic criteria. Uterine sarcomas Methods. Medline was searched between 1976 and 2009 for all publications in English where the studied Leiomyosarcoma population included women diagnosed of uterine sarcomas. Endometrial stromal sarcoma fi Undifferentiated endometrial sarcoma Results. Since carcinosarcomas (malignant mixed mesodermal tumors or MMMT) are currently classi ed Adenosarcoma as metaplastic carcinomas, leiomyosarcomas remain the most common uterine sarcomas. Exclusion of Carcinosarcoma several histologic variants of leiomyoma, as well as “smooth muscle tumors of uncertain malignant potential,” frequently misdiagnosed as sarcomas, has made apparent that leiomyosarcomas are associated with poor prognosis even when seemingly confined to the uterus. Endometrial stromal sarcomas are indolent tumors associated with long-term survival. Undifferentiated endometrial sarcomas exhibiting nuclear pleomorphism behave more aggressively than tumors showing nuclear uniformity. -

Mr Leiomyoma Vs Leiomyosarcoma
2 0 SCBT· MR 1 LEIOMYOMA VS LEIOMYOSARCOMA 5 Susan M. Ascher, MD Professor & Co-Director of Abdominal Imaging Georgetown University Hospital, Washington, DC T2-W MRI: Normal Uterus, Leiomyoma and Leiomyosarcoma NORMAL LEIOMYOMA LEIOMYOSARCOMA LEIOMYOMA or LEIOMYOSARCOMA LEIOMYOMA LEIOMYOSARCOMA LEIOMYOMA or LEIOMYOSARCOMA LEIOMYOMA LEIOMYOSARCOMA LEIOMYOMA or LEIOMYOSARCOMA LEIOMYOMA LEIOMYOSARCOMA DEGENERATED LEIOMYOMA vs LEIOMYOSARCOMA Distinguishing the two can be challenging Laparoscopic Power Morcellators • Hysterectomy • Myommectomy Prognosis is significantly worse in women who had leiomyosarcomas morcellated than women who underwent standard abdominal hysterectomy Park JY, et al. Gynecol Oncol 2011; 122:255-259. Perri T, et al. Int J Gyencol Cancer 2009; 19:257-260 DEGENERATED LEIOMYOMA vs LEIOMYOSARCOMA Distinguishing the two can be challenging 4/17/14: FDA safety warning on LPM for hysterectomy & myomectomy • Prev of unsuspected uterine sarcoma: 1 in 352 • Prev of unsuspected uterine LMS: 1 in 498 • Upstaging sarcoma 1 in 7000 Pritts et al (open source) 7/10 -11/14: FDA OB-GYN Devices Panel FDA: Quantitative Assessment of the Prevalence of Unsuspected Uterine Sarcoma in Women undergoing Treatment of Uterine Fibroids. Summary and Key Findings http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM393589. 7.11.14: “Fate of Uterine Device Now in Hands of FDA: Panel's Recommendations Run From Outright Ban to 'Black Box' Warning to Limited Use” Ethicon voluntarily suspend sales and recalls devices worldwide 9.22.14: “Gynecologists Resist FDA Over Popular Surgical Tool: Doctors Continue to Use Morcellators Months After Regulator Warned They Can Spread Undetected Cancer” 11.24.2014: FDA Black Box Warning & IIE “Warning Prompts Shift in Surgeries on Women” A Yale University study found that 84% of gynecological surgeons at large U.S. -

A Rare Presentation of Benign Brenner Tumor of Ovary: a Case Report
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Periasamy S et al. Int J Reprod Contracept Obstet Gynecol. 2018 Jul;7(7):2971-2974 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20182920 Case Report A rare presentation of benign Brenner tumor of ovary: a case report Sumathi Periasamy1, Subha Sivagami Sengodan2*, Devipriya1, Anbarasi Pandian2 1Department of Surgery, 2Department of Obstetrics and Gynaecology, Government Mohan Kumaramangalam Medical College, Salem, Tamil Nadu, India Received: 17 April 2018 Accepted: 23 May 2018 *Correspondence: Dr. Subha Sivagami Sengodan, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Brenner tumors are rare ovarian tumors accounting for 2-3% of all ovarian neoplasms and about 2% of these tumors are borderline (proliferating) or malignant. These tumors are commonly seen in 4th-8th decades of life with a peak in late 40s and early 50s. Benign Brenner tumors are usually small, <2cm in diameter and often detected incidentally during surgery or on pathological examination. Authors report a case of a large, calcified benign Brenner tumor in a 55-year-old postmenopausal woman who presented with complaint of abdominal pain and mass in abdomen. Imaging revealed large complex solid cystic pelvic mass -peritoneal fibrosarcoma. She underwent laparotomy which revealed huge Brenner tumor weighing 9kg arising from left uterine cornual end extending up to epigastric region. -
Resistance to Immune Checkpoint Blockade in Uterine Leiomyosarcoma: What Can We Learn from Other Cancer Types?
cancers Review Resistance to Immune Checkpoint Blockade in Uterine Leiomyosarcoma: What Can We Learn from Other Cancer Types? Wout De Wispelaere 1 , Daniela Annibali 1,2 , Sandra Tuyaerts 1,3 , Diether Lambrechts 4,5 and Frédéric Amant 1,6,7,* 1 Department of Oncology, KU Leuven (University of Leuven) and Leuven Cancer Institute (LKI), 3000 Leuven, Belgium; [email protected] (W.D.W.); [email protected] (D.A.); [email protected] (S.T.) 2 Division of Oncogenomics, Antoni Van Leeuwenhoek—Netherlands Cancer Institute (AvL-NKI), 1066 CX Amsterdam, The Netherlands 3 Laboratory of Medical and Molecular Oncology (LMMO), Department of Medical Oncology, Vrije Universiteit Brussel (VUB), Universitair Ziekenhuis Brussel (UZ Brussel), 1090 Brussels, Belgium 4 Laboratory for Translational Genetics, Department of Human Genetics, KU Leuven (University of Leuven), 3000 Leuven, Belgium; [email protected] 5 VIB Center for Cancer Biology, Flemish Institute for Biotechnology (VIB), 3000 Leuven, Belgium 6 Centre for Gynecologic Oncology Amsterdam (CGOA), Antoni Van Leeuwenhoek—Netherlands Cancer Institute, University Medical Center (UMC), 1066 CX Amsterdam, The Netherlands 7 Department of Obstetrics and Gynecology, University Hospitals Leuven (UZ Leuven), 3000 Leuven, Belgium * Correspondence: [email protected] Simple Summary: Immune checkpoint blockade (ICB) has emerged as a very promising therapeutic option for patients, demonstrating unprecedented, durable responses in several difficult-to-treat Citation: De Wispelaere, W.; cancers. Despite research indicating a strong potential for ICB in uterine leiomyosarcomas (uLMSs), a Annibali, D.; Tuyaerts, S.; Lambrechts, clinical trial assessing response to ICB monotherapy in uLMSs showed no clinical benefit. Resistance D.; Amant, F. Resistance to Immune to ICB has been studied extensively in a variety of tumor types, but the resistance mechanisms Checkpoint Blockade in Uterine explaining the lack of response to ICB in uLMSs remain largely unexplored. -
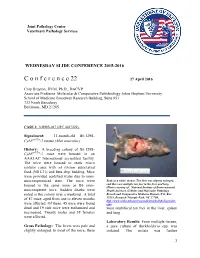
C O N F E R E N C E 22 27 April 2016
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2015-2016 C o n f e r e n c e 22 27 April 2016 Cory Brayton, DVM, Ph.D., DACVP Associate Professor, Molecular & Comparative Pathobiology Johns Hopkins University School of Medicine Broadway Research Building, Suite 851 733 North Broadway Baltimore, MD 21205 CASE I: NIEHS-087 (JPC 4017222). Signalment: 11-month-old B6.129S- Cybbtm1Din/J mouse (Mus musculus) History: A breeding colony of B6.129S- Cybbtm1Din/J mice were housed in an AAALAC International accredited facility. The mice were housed in static micro isolator cases with ad libitum autoclaved food (NIH-31) and beta chip bedding. Mice were provided acidified water due to imm- unocompromised state. The mice were Body as a while, mouse. The liver was slightly enlarged, housed in the same room as B6 imm- and there are multiple tan foci in the liver and lung. (Photo courtesy of: National Institute of Environmental unocompetent mice. Sudden deaths were Health Sciences, Cellular and Molecular Pathology noted in the colony over a weekend. A total Branch and Comparative Medicine Branch, P.O. Box of 87 mice, aged from one to eleven months 12233, Research Triangle Park, NC 27709, http://www.niehs.nih.gov/research/atniehs/labs/lep/index. were affected. Of these, 45 mice were found cfm) dead and 19 sick mice were euthanized and were multifocal tan foci in the liver, spleen necropsied. Twenty males and 38 females and lung. were affected. Laboratory Results: From multiple tissues, Gross Pathology: The livers were pale and a pure culture of Burkholderia spp. -

Understanding Your Pathology Report: Benign Breast Conditions
cancer.org | 1.800.227.2345 Understanding Your Pathology Report: Benign Breast Conditions When your breast was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from a breast biopsy1, such as a needle biopsy or an excision biopsy. In a needle biopsy, a hollow needle is used to remove a sample of an abnormal area. An excision biopsy removes the entire abnormal area, often with some of the surrounding normal tissue. An excision biopsy is much like a type of breast-conserving surgery2 called a lumpectomy. What does it mean if my report uses any of the following terms: adenosis, sclerosing adenosis, apocrine metaplasia, cysts, columnar cell change, columnar cell hyperplasia, collagenous spherulosis, duct ectasia, columnar alteration with prominent apical snouts and secretions (CAPSS), papillomatosis, or fibrocystic changes? All of these are terms that describe benign (non-cancerous) changes that the pathologist might see under the microscope. They do not need to be treated. They are of no concern when found along with cancer. More information about many of these can be found in Non-Cancerous Breast Conditions3. What does it mean if my report says fat necrosis? Fat necrosis is a benign condition that is not linked to cancer risk. -

Bilateral Giant Juvenile Fibroadenomas of Breasts: a Case Report
SAGE-Hindawi Access to Research Pathology Research International Volume 2011, Article ID 482046, 4 pages doi:10.4061/2011/482046 Case Report Bilateral Giant Juvenile Fibroadenomas of Breasts: A Case Report D. B. Nikumbh, S. R. Desai, P. S. Madan, N. J. Patil, and J. V. Wader Department of Pathology, Krishna Institute of Medical Sciences, Karad, District Satara, Maharashtra 415110, India Correspondence should be addressed to D. B. Nikumbh, drdhirajnikumbh@rediffmail.com Received 9 October 2010; Revised 4 April 2011; Accepted 7 April 2011 Academic Editor: Elizabeth Wiley Copyright © 2011 D. B. Nikumbh et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Juvenile fibroadenoma constitutes only 4% of the total fibroadenomas. The incidence of giant juvenile fibroadenomas is found to be only 0.5% of all the fibroadenomas. Bilateral giant juvenile fibroadenomas are extremely rare, and only four cases have been reported in the literature. Tothe best of our knowledge, we are presenting the fifth case of bilateral giant juvenile fibroadenomas in a 12-year-old prepubertal girl. The diagnosis was made on fine-needle aspiration cytology which was confirmed on histopathology. In this paper, we present this rare case to illustrate the diagnosis and management of this tumour and to emphasize that these tumours are almost always benign and should be treated with breast-conserving surgery to provide a healthy physical and social life to the patient. 1. Introduction both the breasts were seen, which were firm in consistency. -

Diagnostic Approach to Soft Tissue Tumour of the Breast and Phyllodes Tumour in Ilorin, North Central with Review of Institutional Experience
World Journal of Medical Case Reports 2021; 2(3): 29-34 http://www.sciencepublishinggroup.com/j/wjmcr doi: 10.11648/j.wjmcr.20210203.11 Diagnostic Approach to Soft Tissue Tumour of the Breast and Phyllodes Tumour in Ilorin, North Central with Review of Institutional Experience Rasheed Mumini Wemimo 1, *, Afolayan Enoch Abiodun 1, Adegboye Adeyemi Taiwo 2 1Department of Pathology, University of Ilorin Teaching Hospital, Ilorin, Nigeria 2Mojitaiwo Data Services and Data Management Executives, Ilorin, Nigeria Email address: *Corresponding author To cite this article: Rasheed Mumini Wemimo, Afolayan Enoch Abiodun, Adegboye Adeyemi Taiwo. Diagnostic Approach to Soft Tissue Tumour of the Breast and Phyllodes Tumour in Ilorin, North Central with review of Institutional Experience. World Journal of Medical Case Reports. Vol. 2, No. 3, 2021, pp. 29-34. doi: 10.11648/j.wjmcr.20210203.11 Received : May 13, 2021; Accepted : June 7, 2021; Published : July 9, 2021 Abstract: Background: Primary soft tissue tumour (primary mesenchymal tumour) of the breast comprised of spectrum of neoplasm that arise from mammary stroma with comparable tumour biology of primary mesenchymal tumour at other sites. There are palpable diagnostic challenges which can be resolved by considering histomorphologic analysis that characterized each tumour entity regardless of the site and the use immunohistochemical markers. Methodology: This is an analytical hospital based retrospective study of patients with primary breast mesenchymal tumour and phyllodes diagnosed during 2014– 2019 at the Department of Pathology, University of Ilorin Teaching Hospital. The histopathological diagnosis of primary mesenchymal tumour of the breast and phyllodes tumours with documented age and other inclusion criteria were used for the study but excluded patients with incomplete information. -

Primary Breast Leiomyosarcoma and Synchronous Homolateral Lung Cancer: a Case Report
1059 Case Report Primary breast leiomyosarcoma and synchronous homolateral lung cancer: a case report Alberto Testori1, Stefano Meroni2, Emanuele Voulaz1, Marco Alloisio1, Rita De Sanctis3,4, Paola Bossi5, Umberto Cariboni1, Matilde De Simone6, Ugo Cioffi6 1General and Thoracic Surgery, Humanitas Research Hospital, Rozzano (Milan), Italy; 2Division of Breast Radiology, European Institute of Oncology, Milan, Italy; 3Department of Medical Oncology and Hematology, Humanitas Research Hospital, Rozzano (Milan), Italy; 4Molecular and Cellular Networks Lab, Department of Anatomy, Histology, Forensic Medicine and Orthopaedics, 'Sapienza' University, Rome, Italy; 5Department of Anatomo-Pathology, Humanitas Research Hospital, Rozzano (Milan), Italy; 6Department of Surgery, University of Milan, Milan, Italy Correspondence to: Alberto Testori, MD. General and Thoracic Surgery, Humanitas Research Hospital, Via Manzoni, 56, 20089 Rozzano (Milan), Italy. Email: [email protected]. Abstract: Radiological and histological features of breast leiomyosarcoma can mimic a wide variety of other breast lesions, such as mesenchymal tumors, breast lymphomas, poorly differentiated carcinomas and metaplastic breast carcinomas. The authors present the case of a 62-year-old woman with a primary breast leiomyosarcoma with synchronous ipsilateral lung adenocarcinoma. The latter was an incidental finding during pre-surgical staging examinations. Clinicopathological, immunophenotypic and imaging features cancer are described. A brief review of the literature on imaging findings and management of breast leiomyosarcoma is presented. The authors discuss the differential diagnoses in breast imaging and of the extra-mammary incidental findings. Surgical resection remains the cornerstone of treatment, while radiation therapy and chemotherapy remain to be defined on a single-patient basis. Keywords: Breast leiomyosarcoma; lung cancer; synchronous tumors Submitted May 14, 2017. -

Phyllodes Tumor of the Vulva: Report of Two Cases Vulvanın Fillods Tümörü: İki Olgu Sunumu
Olgu Sunumu/Case Report doi: 10.5146/tjpath.2013.01153 Phyllodes Tumor of the Vulva: Report of Two Cases Vulvanın Fillods Tümörü: İki Olgu Sunumu İrem Hicran Özbudak1, Hampar Akkaya2, Bahar Akkaya1, Gülgün ERDOĞAN1, Hadice Elif PEŞTERElİ1, Fatma Şeyda Karavelİ1 1Department of Pathology, Akdeniz University, Faculty of Medicine, ANTALYA, TURKEY, 2Başkent University, Faculty of Medicine, Alanya Hospital, ANTALYA, TURKEY ABSTRACT ÖZ Ectopic breast tissue can occur anywhere along the primitive Ektopik meme dokusu ilkel embriyonik sütyolu boyunca herhangi bir embryonic milk line and can be the site of the same pathologic yerde ortaya çıkabilir ve normal memede izlenebilen aynı patolojik processes found in the normal breast. Phyllodes tumor is an durumlar ektopik meme dokusunda da görülebilir. Fillods tümör extremely rare fibroepithelial neoplasm that occurs in ectopic breast vulvadaki ektopik meme dokusunda oluşan nadir bir fibroepitelyal tissue of the vulva. To date, only 8 cases of phyllodes tumor in the neoplazidir. Literatürde bugüne kadar 8 olgu bildirilmiştir. Bu vulva have been reported in the literature. This paper presents two makalede literatüre ek olarak iki ayrı vulvar fillods tümör vakası additional case of benign phyllodes tumor in the vulva. The first sunulmuştur. İlk olgu, sol ön mons pubiste boyutu son üç ayda artış patient was a 43-year-old woman, presenting with a lesion on the gösteren bir lezyon ile kliniğe başvurmuş 43 yaşında kadın hastadır. left anterior mons pubis that had increased in size in the last three İkinci olgu 50 yaşında kadın hasta olup, iki aydır varolan sağ labium months. The second patient was a 50-year-old woman, presenting majusta kitle ile başvurmuştur. -

Giant Juvenile Fibroadenoma of Breast
Journal of Surgical Sciences (2013) Vol. 17 (2) : 99-102 © 2012 Society of Surgeons of Bangladesh JOURNAL OF SURGICAL SCIENCES Case Report GIANT JUVENILE FIBROADENOMA OF BREAST 2 2 3 5 KABM Taiful Alam1, Toufiqul Haque , Shamim Hossain , Kuntal Das , Tazul lslam4, Helena Ahmed Abstract: Giant juvenile fibroadenoma occurs in adolescent girls. These tumours become enormous in size and grow rapidly, though these tumours are mostly benign. These patients are almost always treated by breast conserving surgery. Here we present a case having unilateral giant juvenile fibroadenoma with bilateral multiple small fibroadenomas in an adolescent female aged 16years. The diagnosis of the patient was made on clinical examination, USG & FNAC. Confirmatory diagnosis was made by histopathology. We removed the giant one with "Swiss-Roll" procedure and others by simple enucleation. The aesthatic appearence of the breasts were preserved. Key words: Fibroadenoma, Giant fibroadenoma, Juvenile fibroadenoma, Swiss-roll operation. Introduction: can grow to immense proportions, compressing and Fibroadenoma is the most common benign tumour of displacing normal breast tissue and stretching the 4 female breast.It usually arises in the fully developed overlying skin and nipple areola complex . breast during the 15-25 years age period. They arise from hyperplasia of both fibrous & glandular tissue of Case report: a single lobule & usually grow upto 2-3 cm in size. A 16 year old girl presented with bilateral breast lumps Juvenile fibroadenoma is a benign tumour which occurs for 1 year. There were multiple lumps in the both during puberty1. It is a rare clinical condition and forms breasts among them one lump in the left breast was 4% of the total fibroadenomes--'. -

Non-Cancerous Breast Conditions Fibrosis and Simple Cysts in The
cancer.org | 1.800.227.2345 Non-cancerous Breast Conditions ● Fibrosis and Simple Cysts ● Ductal or Lobular Hyperplasia ● Lobular Carcinoma in Situ (LCIS) ● Adenosis ● Fibroadenomas ● Phyllodes Tumors ● Intraductal Papillomas ● Granular Cell Tumors ● Fat Necrosis and Oil Cysts ● Mastitis ● Duct Ectasia ● Other Non-cancerous Breast Conditions Fibrosis and Simple Cysts in the Breast Many breast lumps turn out to be caused by fibrosis and/or cysts, which are non- cancerous (benign) changes in breast tissue that many women get at some time in their lives. These changes are sometimes called fibrocystic changes, and used to be called fibrocystic disease. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Fibrosis and cysts are most common in women of child-bearing age, but they can affect women of any age. They may be found in different parts of the breast and in both breasts at the same time. Fibrosis Fibrosis refers to a large amount of fibrous tissue, the same tissue that ligaments and scar tissue are made of. Areas of fibrosis feel rubbery, firm, or hard to the touch. Cysts Cysts are fluid-filled, round or oval sacs within the breasts. They are often felt as a round, movable lump, which might also be tender to the touch. They are most often found in women in their 40s, but they can occur in women of any age. Monthly hormone changes often cause cysts to get bigger and become painful and sometimes more noticeable just before the menstrual period. Cysts begin when fluid starts to build up inside the breast glands. Microcysts (tiny, microscopic cysts) are too small to feel and are found only when tissue is looked at under a microscope.