Meniere's Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Age-Related Hearing Loss
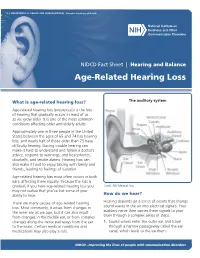
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES ∙ National Institutes of Health NIDCD Fact Sheet | Hearing and Balance Age-Related Hearing Loss What is age-related hearing loss? The auditory system Age-related hearing loss (presbycusis) is the loss of hearing that gradually occurs in most of us as we grow older. It is one of the most common conditions affecting older and elderly adults. Approximately one in three people in the United States between the ages of 65 and 74 has hearing loss, and nearly half of those older than 75 have difficulty hearing. Having trouble hearing can make it hard to understand and follow a doctor’s advice, respond to warnings, and hear phones, doorbells, and smoke alarms. Hearing loss can also make it hard to enjoy talking with family and friends, leading to feelings of isolation. Age-related hearing loss most often occurs in both ears, affecting them equally. Because the loss is gradual, if you have age-related hearing loss you Credit: NIH Medical Arts may not realize that you’ve lost some of your ability to hear. How do we hear? There are many causes of age-related hearing Hearing depends on a series of events that change loss. Most commonly, it arises from changes in sound waves in the air into electrical signals. Your the inner ear as we age, but it can also result auditory nerve then carries these signals to your from changes in the middle ear, or from complex brain through a complex series of steps. changes along the nerve pathways from the ear 1. -

Press Release
Ménière's Society for dizziness and balance disorders NEWS RELEASE Release date: Monday 17 September 2018 Getting help if your world is in a spin Feeling dizzy and losing your balance is an all too common problem for many people but would you know what to do and where to get help if this happened to you? A loss of balance can lead to falls whatever your age. Around 30% of people under the age of 65 suffer from falls with one in ten people of working age seeking medical advice for vertigo which can lead to life changing or life inhibiting symptoms. Balance disorders are notoriously difficult to diagnose accurately. Most people who feel giddy, dizzy, light-headed, woozy, off-balance, faint or fuzzy, have some kind of balance disorder. This week (16-22 September 2018) is Balance Awareness Week. Organised by the Ménière's Society, the only registered charity in the UK dedicated solely to supporting people with inner ear disorders, events up and down the country will aim to raise awareness of how dizziness and balance problems can affect people and direct them to sources where they can find support. This year Balance Awareness Week also sees the launch of the world’s first Balance Disorder Spectrum, enabling for the first time easy reference to the whole range of balance disorders in one easy to use interactive web site. Medical science is continuously updating and revising its understanding of these often distressing and debilitating conditions. The many different symptoms and causes of balance disorders mean that there have been few attempts to show what they have in common, until now. -

How Do I Know If I Have a Balance Disorder?
PO BOX 13305 · PORTLAND, OR 97213 · FAX: (503) 229-8064 · (800) 837-8428 · [email protected] · WWW.VESTIBULAR.ORG How Do I Know if I Have a Balance Disorder? This article is adapted from information provided by the National Institute on Deafness and Other Communications Disorders, (NIDCD). Millions of individuals have disorders of sensation of spatial disorientation or balance they describe as “dizziness.” imbalance. Experts believe that more than four out of ten Americans will experience an Almost everyone experiences a few episode of dizziness significant enough to seconds of dizziness or disequilibrium at send them to a doctor. some point —for example, when a person stands on a train platform and What can be difficult for both a patient momentarily perceives an illusion of and his or her doctor is that the word moving as a train rushes past. However, “dizziness” is a subjective term. This for some people, symptoms can be means that the word can be used by intense and last a long time, affecting a people to describe different sensations person’s independence, ability to work, they are experiencing, but it is hard for and quality of life. anyone but the person experiencing the symptoms to understand or measure Balance disorders can be caused by the nature or severity of the sensations. medications or certain health conditions, In addition, people tend to use different including problems with the inner ear terms to describe the same kind of (vestibular) organs or the brain. problem. “Dizziness,” “vertigo,” and Dizziness, vertigo, and disequilibrium are “disequilibrium” are often used all symptoms that can result from a interchangeably, even though they have peripheral vestibular disorder (a different meanings. -

Facts About Noise-Induced Hearing Loss Over 85 Db
Facts about Noise-Induced Hearing Loss over 85 dB. Sound loudness is measured in Approximately 40 million American adults may have units called decibels (dB). hearing loss resulting from noise exposure.1 Noise- 60 dB Normal conversations, induced hearing loss is caused by damage to the dishwashers hair cells found in the inner ear. Hair cells are small 80 dB Alarm clocks sensory cells that convert the sounds we hear 90 dB Hair dryers, blenders, (sound energy) into electrical signals that travel to lawnmowers the brain. Once damaged, our hair cells cannot 100 dB MP3 players at full volume grow back, which results in permanent hearing loss. 110 dB Concerts (any music genre), car racing, sporting events Hearing protection decreases the intensity, or 120 dB Jet planes at take off loudness, of noise and helps preserve your hearing. 130 dB Ambulance, fire engine sirens 140 dB Gun shots, fireworks, custom car Harmful sounds are those that are too loud and last stereos at full volume too long or are very loud and sudden. For example, exposure to a one-time intense “impulse” sound Protect your hearing: such as an explosion, or continuous exposure to • Wear hearing protection when around loud sounds over an extended period of time such sounds louder than 85 dB. There are as at a concert may be harmful. The louder the different types of hearing protection such as sound, the shorter the amount of time you can foam earplugs, earmuffs, and custom safely be around it. hearing protection devices • Contact your local audiologist for custom You may encounter harmful sounds at work, at hearing protection devices. -

Migraine Associated Vertigo
Headache: The Journal of Head and Face Pain VC 2015 American Headache Society Published by JohnWiley & Sons, Inc. doi: 10.1111/head.12704 Headache Toolbox Migraine Associated Vertigo Between 30 and 50% of migraineurs will sometimes times a condition similar to benign positional vertigo experience dizziness, a sense of spinning, or feeling like called vestibular neuronitis (or vestibular neuritis/labyrinthi- their balance is off in the midst of their headaches. This is tis) is triggered by a viral infection of the inner ear, result- now termed vestibular migraine, but is also called ing in constant vertigo or unsteadiness. Symptoms can migraine associated vertigo. Sometimes migraineurs last for a few days to a few weeks and then go away as experience these symptoms before the headache, but mysteriously as they came on. Vestibular migraine, by they can occur during the headache, or even without any definition, should have migraine symptoms in at least head pain. In children, vertigo may be a precursor to 50% of the vertigo episodes, and these include head migraines developing in the teens or adulthood. Migraine pain, light and noise sensitivity, and nausea. associated vertigo may be more common in those with There are red flags, which are warning signs that ver- motion sickness. tigo is not part of a migraine. Sudden hearing loss can be For some patients this vertiginous sensation resem- the sign of an infection that needs treatment. Loss of bal- bles migraine aura, which is a reversible, relatively short- ance alone, or accompanied by weakness can be the lived neurologic symptom associated with their migraines. -

Balance Disorder Spectrum Technical Report: January 2018
Balance Disorder Spectrum Technical Report: January 2018 Professor Andrew Hugill Professor Peter Rea College of Science and Engineering The Leicester Balance Centre University of Leicester Department of ENT Leicester, UK Leicester Royal Infirmary [email protected] Leicester, UK Abstract—This paper outlines the technical aspects of the first version of a new spectrum of balance disorders. It describes the II. BALANCE DISORDER SPECTRUM implementation of the spectrum in an interactive web page and proposes some avenues for future research and development. A. Rationale Balance disorders are often both unclear and difficult to Keywords—balance, disorder, spectrum diagnose, so the notion of a spectrum may well prove useful as an introduction to the field. Thanks to existing spectrums (e.g. I. INTRODUCTION autism), the general public is now familiar with the idea of a This project seeks to create an interactive diagnostic tool collection of related disorders ranging across a field that might for the identification of balance disorders, to be used by be anything from mild to severe. The importance of balance clnicians and GPs as well as the wider public. There are three disorders is generally underestimated. The field has suffered main layers to the project: from a fragmented nomenclature and conflicting medical opinions, resulting from a general uncertainty and even • the establishment of the concept of a spectrum of confusion about both symptoms and causes. Terms such as: balance disorders; dizzy, light-headed, floating, woozy, giddy, off-balance, • the creation of an interactive web page providing feeling faint, helpless, or fuzzy, are used loosely and access to the spectrum and its underlying medical interchangeably, consolidating the impression that this is a information; vague collection of ailments. -

Mal De Debarquement Syndrome (Mdds)?
What is Mal de Debarquement Syndrome (MdDS)? MdDS is a rare and life-altering balance disorder that most commonly develops after an ocean cruise or other type of water travel. MdDS is also known as disembarkment disease or persistent landsickness. MdDS also occurs following air/train travel or other motion experiences or spontaneously/in the absence of a motion event. MdDS is a syndrome because it often includes a diverse array of symptoms. The characteristic symptom of MdDS is a persistent sensation of motion such as rocking, swaying and/or bobbing. Other MdDS Symptoms: MAL de • Disequilibrium - a sensation of unsteadiness DEBARQUEMENT or loss of balance • Fatigue; extreme, unusual SYNDROME • Cognitive impairment - difficulty concentrating, confusion, memory loss …a persistent • Anxiety, depression motion and imbalance disorder… • Ataxia – unsteady, staggering gait • Sensitivity to flickering lights, loud or sudden noises, fast or sudden movements, enclosed areas or busy patterns Do you know a person who has • Headaches, including migraine headaches • Heaviness - sensation of gravitational pull of returned from an ocean cruise and the head, body or feet feels like they are still on the boat – • Dizziness months/years later? • Ear pain and/or fullness • Tinnitus – ringing in the ears Perhaps they returned from a • Nausea plane, train or lengthy car ride, and Most MdDS patients feel relief while driving/ it now feels like they are on a ship riding in an auto, airplane, train or other at sea. motion activities. However, the abnormal sensation of motion returns as soon as the They may be suffering from Mal de motion activity is suspended. This is a Debarquement Syndrome (MdDS), helpful feature in the diagnosis of MdDS. -

Vestibular Neuritis and Labyrinthitis
Vestibular Neuritis and DISORDERS Labyrinthitis: Infections of the Inner Ear By Charlotte L. Shupert, PhD with contributions from Bridget Kulick, PT and the Vestibular Disorders Association INFECTIONS Result in damage to inner ear and/or nerve. ARTICLE 079 DID THIS ARTICLE HELP YOU? SUPPORT VEDA @ VESTIBULAR.ORG Vestibular neuritis and labyrinthitis are disorders resulting from an 5018 NE 15th Ave. infection that inflames the inner ear or the nerves connecting the inner Portland, OR 97211 ear to the brain. This inflammation disrupts the transmission of sensory 1-800-837-8428 information from the ear to the brain. Vertigo, dizziness, and difficulties [email protected] with balance, vision, or hearing may result. vestibular.org Infections of the inner ear are usually viral; less commonly, the cause is bacterial. Such inner ear infections are not the same as middle ear infections, which are the type of bacterial infections common in childhood affecting the area around the eardrum. VESTIBULAR.ORG :: 079 / DISORDERS 1 INNER EAR STRUCTURE AND FUNCTION The inner ear consists of a system of fluid-filled DEFINITIONS tubes and sacs called the labyrinth. The labyrinth serves two functions: hearing and balance. Neuritis Inflamation of the nerve. The hearing function involves the cochlea, a snail- shaped tube filled with fluid and sensitive nerve Labyrinthitis Inflamation of the labyrinth. endings that transmit sound signals to the brain. Bacterial infection where The balance function involves the vestibular bacteria infect the middle organs. Fluid and hair cells in the three loop-shaped ear or the bone surrounding semicircular canals and the sac-shaped utricle and Serous the inner ear produce toxins saccule provide the brain with information about Labyrinthitis that invade the inner ear via head movement. -

Vestibular Neuritis, Labyrinthitis, and a Few Comments Regarding Sudden Sensorineural Hearing Loss Marcello Cherchi
Vestibular neuritis, labyrinthitis, and a few comments regarding sudden sensorineural hearing loss Marcello Cherchi §1: What are these diseases, how are they related, and what is their cause? §1.1: What is vestibular neuritis? Vestibular neuritis, also called vestibular neuronitis, was originally described by Margaret Ruth Dix and Charles Skinner Hallpike in 1952 (Dix and Hallpike 1952). It is currently suspected to be an inflammatory-mediated insult (damage) to the balance-related nerve (vestibular nerve) between the ear and the brain that manifests with abrupt-onset, severe dizziness that lasts days to weeks, and occasionally recurs. Although vestibular neuritis is usually regarded as a process affecting the vestibular nerve itself, damage restricted to the vestibule (balance components of the inner ear) would manifest clinically in a similar way, and might be termed “vestibulitis,” although that term is seldom applied (Izraeli, Rachmel et al. 1989). Thus, distinguishing between “vestibular neuritis” (inflammation of the vestibular nerve) and “vestibulitis” (inflammation of the balance-related components of the inner ear) would be difficult. §1.2: What is labyrinthitis? Labyrinthitis is currently suspected to be due to an inflammatory-mediated insult (damage) to both the “hearing component” (the cochlea) and the “balance component” (the semicircular canals and otolith organs) of the inner ear (labyrinth) itself. Labyrinthitis is sometimes also termed “vertigo with sudden hearing loss” (Pogson, Taylor et al. 2016, Kim, Choi et al. 2018) – and we will discuss sudden hearing loss further in a moment. Labyrinthitis usually manifests with severe dizziness (similar to vestibular neuritis) accompanied by ear symptoms on one side (typically hearing loss and tinnitus). -

Bedside Neuro-Otological Examination and Interpretation of Commonly
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.054478 on 24 November 2004. Downloaded from BEDSIDE NEURO-OTOLOGICAL EXAMINATION AND INTERPRETATION iv32 OF COMMONLY USED INVESTIGATIONS RDavies J Neurol Neurosurg Psychiatry 2004;75(Suppl IV):iv32–iv44. doi: 10.1136/jnnp.2004.054478 he assessment of the patient with a neuro-otological problem is not a complex task if approached in a logical manner. It is best addressed by taking a comprehensive history, by a Tphysical examination that is directed towards detecting abnormalities of eye movements and abnormalities of gait, and also towards identifying any associated otological or neurological problems. This examination needs to be mindful of the factors that can compromise the value of the signs elicited, and the range of investigative techniques available. The majority of patients that present with neuro-otological symptoms do not have a space occupying lesion and the over reliance on imaging techniques is likely to miss more common conditions, such as benign paroxysmal positional vertigo (BPPV), or the failure to compensate following an acute unilateral labyrinthine event. The role of the neuro-otologist is to identify the site of the lesion, gather information that may lead to an aetiological diagnosis, and from there, to formulate a management plan. c BACKGROUND Balance is maintained through the integration at the brainstem level of information from the vestibular end organs, and the visual and proprioceptive sensory modalities. This processing takes place in the vestibular nuclei, with modulating influences from higher centres including the cerebellum, the extrapyramidal system, the cerebral cortex, and the contiguous reticular formation (fig 1). -

Hearing Loss, Vertigo and Tinnitus
HEARING LOSS, VERTIGO AND TINNITUS Jonathan Lara, DO April 29, 2012 Hearing Loss Facts S Men are more likely to experience hearing loss than women. S Approximately 17 percent (36 million) of American adults report some degree of hearing loss. S About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. S Nine out of every 10 children who are born deaf are born to parents who can hear. Hearing Loss Facts S The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities. S Only 1 out of 5 people who could benefit from a hearing aid actually wears one. S Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old. Hearing Loss Facts S There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing impairment. S Roughly 25 million Americans have experienced tinnitus. S Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing Loss Facts S Approximately 615,000 individuals have been diagnosed with Ménière's disease in the United States. Another 45,500 are newly diagnosed each year. S One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma). -

Hearing Loss
Randal W. Swenson, M.D. Joshua G. Yorgason, M.D. David K. Palmer, M.D. Wesley R. Brown, M.D. John E. Butler, M.D. Nancy J. Stevenson, PA-C Justin D. Gull, M.D. ENT SPECIALISTS Kristin G. Hoopes, PA-C www.entslc.com Hearing Loss Approximately one in ten persons in the United may result from blockage of the ear canal (wax), States has some degree of hearing loss. Hearing is from a perforation (hole) in the ear drum, or from measured in decibels (dB), and a hearing level of 0- infection or disease of any of the three middle ear 25 dB is considered normal hearing. Your level is: bones. With a conductive loss only, the patient will never go deaf, but will always be able to hear, either Right ear _______ dB Left ear _______dB with reconstructive ear surgery or by use of a properly fitted hearing aid. Some patients who are Hearing Severity / % Loss not candidates for surgery, may benefit from a new 25 dB (normal).….0% 65dB(Severe)……...60% technology, the Baha (bone-anchored hearing aid). 35 dB (mild)……..15% 75dB(Severe)……...75% When there is a problem with the inner ear or 45 dB (moderate)..30% >85dB (Profound)..>90% nerve of hearing, a sensori-neural hearing loss occurs. This is most commonly from normal aging, Normal speech discrimination is 88-100%. Yours is: is usually worse in high frequencies, and can progress to total deafness. Noise exposure is another Right ear _______ % Left ear_______% common cause of high frequency hearing loss. Patients with sensori-neural hearing loss usually complain of difficulty hearing in loud environments.