Eye on the Border
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Aafp Fmx 2020
10/7/2020 Common Acute Eye Presentations Dr. Ahmed Mian HonBSc, BEd, MD CCFP (EM) Staff ER Consultant Department of Emergency Medicine, Humber River Hospital and University Health Network Medical Director and Chair, Medical Education HRH ED Investigative Coroner, Province of Ontario Faculty DFCM/EM University of Toronto and DFM Queens' University 1 ACTIVITY DISCLAIMER The material presented here is being made available by the American Academy of Family Physicians for educational purposes only. Please note that medical information is constantly changing; the information contained in this activity was accurate at the time of publication. This material is not intended to represent the only, nor necessarily best, methods or procedures appropriate for the medical situations discussed. Rather, it is intended to present an approach, view, statement, or opinion of the faculty, which may be helpful to others who face similar situations. The AAFP disclaims any and all liability for injury or other damages resulting to any individual using this material and for all claims that might arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by a physician or any other person. Physicians may care to check specific details such as drug doses and contraindications, etc., in standard sources prior to clinical application. This material might contain recommendations/guidelines developed by other organizations. Please note that although these guidelines might be included, this does not necessarily imply the endorsement by the AAFP. 2 2 1 10/7/2020 Disclosure It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/invitation of participation. -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Chalazion Treatment
Chalazion Treatment This material will help you understand treatments for chalazion. What is a chalazion? A chalazion is a red, tender lump in the eyelid. It is also known as a stye. The swelling occurs because one of the oil glands that is next to each eyelash can get backed up and become inflamed. This is very similar to a pimple. How is a chalazion treated? In many cases, chalazia resolve on their own without treatment. Applying a warm compress over your eye for 5- 10 minutes two to four times a day can soften the oil that is backed up. This helps the chalazion heal. If the chalazion does not heal after one month of using warm compresses, your doctor may suggest surgical removal or injection with medications to help it heal faster. How is a chalazion surgically removed? Surgical removal of a chalazion is an outpatient procedure. Before the procedure, your doctor will give you a local anesthetic to numb the area around the chalazion. Next, your doctor will place a clamp to help hold your eyelid in place for the procedure. That way, you will not need to worry about keeping your eyelid open for the procedure. The doctor will then make a small incision in the eyelid and remove the chalazion with a special instrument. The location of the incision (front or back of the eyelid) depends on the size of the chalazion. Small chalazia can be removed by making an incision on the inside of the eyelid. If your chalazion is large, the doctor may make an incision on the front of the eyelid and close it with dissolvable stitches. -

Dry Eye in Patient with Clinical History of Chronic Blepharitis and Chalaziosis Edited by Dr
year 10 num b e r 2 4 e y e d o c t o r m a r ch- a p r i l 2018 CLINICAL CASES OF LUCIO BURATTO Dry eye in patient with clinical history of chronic blepharitis and chalaziosis edited by Dr. Maria Luisa Verbelli, Dr.Alessia Bottoni Observation and 1 anamnesis Arrives at our observation at CIOS, Italian Center for Dry Eye at CAMO, a 56-year-old patient with blepharitis, redness, ocular burning and abundant mucous secretion present in both eyes. Furthermore, an enlarged lymph node is seen in the right laterocervical site. At ocular anamnesis the patient reports chronic blepharitis from the juvenile age, multiple chalazion in both eyes, an operation for right Fig. 1 Handpiece for the application of the pulsed light of the Eye-Light instrument upper eyelid chalaziosis in 2006 (4 upper eyelid chalazion , 3 in the lower); negative anamnesis for these pathologies in the family. The patient is shortsighted since adolescence, has not had any other eye operations and has no ocular allergies. The general anamnesis does not report major systemic diseases or medication intake. On objective examination of the anterior segment we find bilaterally: reduced lacrimal meniscus, posterior blepharitis, obstruction of all the Meibomian glands of the upper and lower eyelids, conjunctival hyperemia with dry spots, transparent cornea, transparent crystalline. The no contact tonometry is 15 mmHg in RE, 16 mmHg in LE. The OCT of the macula does not show changes in both eyes. The BUT is 4.9 seconds in RE, and 15.6 seconds in LE. -

Topographic Outcomes After Corneal Collagen Crosslinking In
ORIGINAL ARTICLE Topographic outcomes after corneal collagen crosslinking in progressive keratoconus: 1-year follow-up Resultados topográficos após crosslinking de colágeno corneano em ceratocone progressivo: 1 ano de seguimento MAURO C. TIVERON JR.1,2, CAMILA RIBEIRO KOCH PENA1, RICHARD YUDI HIDA1,3, LUCIANE BUGMANN MOREIRA4,5, FELIPE ROBERTO EXTERHOTTER BRANCO2, NEWTON KARA-JUNIOR1 ABSTRACT RESUMO Purpose: We aimed to report and analyze topographic and refractive outcomes Objetivos: Relatar e analisar os resultados topográficos e refracionais após cross- following corneal collagen crosslinking (CXL) in patients with progressive kera- linking de colágeno corneano (CXL) em pacientes com ceratocone (KC) progressivo. toconus (KC). Métodos: Estudo retrospectivo analítico e observacional incluindo 100 olhos de Methods: We performed a retrospective, analytical, and observational study of 74 pacientes com KC progressivo submetidos a CXL no Hospital de Olhos do Pa- 100 eyes from 74 progressive KC patients who underwent CXL at the Eye Hospital raná. Valores ceratométricos foram analisados no pré-operatório, 3 e 12 meses de of Paraná. Keratometric values were analyzed preoperatively as well as 3 and 12 pós-operatório. months postoperatively. Resultados: Em um total de 100 olhos, 68 eram do sexo masculino. A idade média Results: For a total of 100 eyes, 68 belonged to male patients. The mean age foi de 19,9 ± 5,61. As médias de parâmetros topográficos e acuidade visual em geral, of our study population was 19.9 ± 5.61 years. The average visual acuity and tiveram estabilidade após 1 ano de follow-up (p<0,05). Após 3 meses, a ceratometria topographic parameters overall were stable after 1 year (p<0.05). -

STYES and CHALAZION
TRE ATM ENT TRE ATM ENT FOR STYES FOR CHALAZION While most styes will drain on their The primary treatment for chalazion is own, the application of a hot or warm application of warm compresses for 10 compress are the most effective to 20 minutes at least 4 times a day. means of accelerating This may soften the hardened oils STYES drainage. The blocking the duct and promote drain- warmth and damp- age and healing. ness encourages the stye to drain. Just like any infection try not to touch it with your fingers. A Chalazion may be treated with compress can be made by putting hot any one or a combination of (not boiling) water on a wash cloth, or antibiotic or steroid drops pre- by using room temperature water and scribed by your healthcare a plastic heat pack. Warm compress- provider. es should be applied for 10—20 and minutes, four (4) times a day. There are occasions when sur- There is also a specialized topical gical drainage is required. ointment for styes, that may be pre- scribed. “Do not use eye makeup Styes may also cause a bruised feel- or wear contact lenses ing around the eye which is treated by application of a warm cloth to the eye. until the stye or chalazion CHALAZION With treatment, styes typically resolve have healed.” within one week. Lancing of a stye is not recommended. Revised: August 2011 WHAT ARE THEY? Signs and Symptoms Signs & Symptoms O f S t ye s of Chalazions The first signs of a stye are: A stye is an infection of the The symptoms of chalazions differ from tenderness, sebaceous glands at the base of the styes as they are usually painless. -

Tissue-Engineered Models for Glaucoma Research
micromachines Review Tissue-Engineered Models for Glaucoma Research Renhao Lu 1 , Paul A. Soden 2 and Esak Lee 1,* 1 Nancy E. and Peter C. Meinig School of Biomedical Engineering, Cornell University, Ithaca, NY 14853, USA; [email protected] 2 College of Human Ecology, Cornell University, Ithaca, NY 14853, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-607-255-8491 Received: 5 June 2020; Accepted: 22 June 2020; Published: 24 June 2020 Abstract: Glaucoma is a group of optic neuropathies characterized by the progressive degeneration of retinal ganglion cells (RGCs). Patients with glaucoma generally experience elevations in intraocular pressure (IOP), followed by RGC death, peripheral vision loss and eventually blindness. However, despite the substantial economic and health-related impact of glaucoma-related morbidity worldwide, the surgical and pharmacological management of glaucoma is still limited to maintaining IOP within a normal range. This is in large part because the underlying molecular and biophysical mechanisms by which glaucomatous changes occur are still unclear. In the present review article, we describe current tissue-engineered models of the intraocular space that aim to advance the state of glaucoma research. Specifically, we critically evaluate and compare both 2D and 3D-culture models of the trabecular meshwork and nerve fiber layer, both of which are key players in glaucoma pathophysiology. Finally, we point out the need for novel organ-on-a-chip models of glaucoma that functionally integrate currently available 3D models of the retina and the trabecular outflow pathway. Keywords: glaucoma; tissue engineering; trabecular meshwork; Schlemm’s canal; retinal ganglion cell; intraocular pressure; optic nerve head; electrospinning; soft lithography; 3D scaffold; 3D bioprinting 1. -

Strabismus: a Decision Making Approach
Strabismus A Decision Making Approach Gunter K. von Noorden, M.D. Eugene M. Helveston, M.D. Strabismus: A Decision Making Approach Gunter K. von Noorden, M.D. Emeritus Professor of Ophthalmology and Pediatrics Baylor College of Medicine Houston, Texas Eugene M. Helveston, M.D. Emeritus Professor of Ophthalmology Indiana University School of Medicine Indianapolis, Indiana Published originally in English under the title: Strabismus: A Decision Making Approach. By Gunter K. von Noorden and Eugene M. Helveston Published in 1994 by Mosby-Year Book, Inc., St. Louis, MO Copyright held by Gunter K. von Noorden and Eugene M. Helveston All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without prior written permission from the authors. Copyright © 2010 Table of Contents Foreword Preface 1.01 Equipment for Examination of the Patient with Strabismus 1.02 History 1.03 Inspection of Patient 1.04 Sequence of Motility Examination 1.05 Does This Baby See? 1.06 Visual Acuity – Methods of Examination 1.07 Visual Acuity Testing in Infants 1.08 Primary versus Secondary Deviation 1.09 Evaluation of Monocular Movements – Ductions 1.10 Evaluation of Binocular Movements – Versions 1.11 Unilaterally Reduced Vision Associated with Orthotropia 1.12 Unilateral Decrease of Visual Acuity Associated with Heterotropia 1.13 Decentered Corneal Light Reflex 1.14 Strabismus – Generic Classification 1.15 Is Latent Strabismus -
Visual Impairment Age-Related Macular
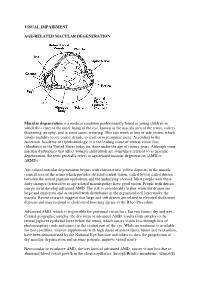
VISUAL IMPAIRMENT AGE-RELATED MACULAR DEGENERATION Macular degeneration is a medical condition predominantly found in young children in which the center of the inner lining of the eye, known as the macula area of the retina, suffers thickening, atrophy, and in some cases, watering. This can result in loss of side vision, which entails inability to see coarse details, to read, or to recognize faces. According to the American Academy of Ophthalmology, it is the leading cause of central vision loss (blindness) in the United States today for those under the age of twenty years. Although some macular dystrophies that affect younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD). Age-related macular degeneration begins with characteristic yellow deposits in the macula (central area of the retina which provides detailed central vision, called fovea) called drusen between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is considerably higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Recent research suggests that large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol lowering agents or the Rheo Procedure. Advanced AMD, which is responsible for profound vision loss, has two forms: dry and wet. Central geographic atrophy, the dry form of advanced AMD, results from atrophy to the retinal pigment epithelial layer below the retina, which causes vision loss through loss of photoreceptors (rods and cones) in the central part of the eye. -

1 42. Ophthalmology Daniel G Vaughan Ocular Emergencies It Is
42. Ophthalmology Daniel G Vaughan Ocular emergencies It is not necessary to refer every patient with an eye disease to an ophthalmologist for treatment. In general, sties, bacterial conjunctivitis, superficial trauma to the lids, corneas, and conjunctiva, and superficial corneal foreign bodies can be treated just as effectively by the surgeon or primary physician as by the ophthalmologist. More serious eye disease such as the following should be referred as soon as possible for specialized care: iritis, acute glaucoma, retinal detachment, strabismus, contusion of the globe, and severe corneal trauma or infection. In the management of acute ocular disorders, it is most important to establish a definitive diagnosis before prescribing treatment. The maxim "All red eyes are not pinkeye" is a useful one, and the physician must be alert for the more serious iritis, keratitis, or glaucoma. The common practice of prescribing "shotgun" topical antibiotic combinations containing corticosteroids is to be discouraged, because inappropriate use of steroids can lead to complications. This chapter attempts to summarize the basic principles and technics of diagnosis and management of common ocular problems, with special emphasis on emergencies, particularly those caused by trauma. Ocular emergencies may be classified as true emergencies or urgent cases. A true emergency is one in which the patient is suffering severe pain or in which a few hours' delay in treatment can lead to permanent ocular damage. An urgent case is one in which treatment should be started as soon as possible but in which a delay of a few days can be tolerated. Foreign Bodies If a patient complains of "something in my eye" and gives a consistent history, a foreign body is usually present even though it may not be readily visible. -

Strabismus Developing After Unilateral and Bilateral Cataract Surgery in Children
Eye (2016) 30, 1210–1214 © 2016 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/16 www.nature.com/eye CLINICAL STUDY Strabismus developing R David, J Davelman, H Mechoulam, E Cohen, I Karshai and I Anteby after unilateral and bilateral cataract surgery in children Abstract Purpose To evaluate the prevalence and common in children with poor final visual risk factors of strabismus in children acuity. undergoing surgery for unilateral or bilateral Eye (2016) 30, 1210–1214; doi:10.1038/eye.2016.162; cataract with or without intraocular lens published online 29 July 2016 implantation. Methods Medical records of pediatric Introduction patients were evaluated from 2000 to 2011. Children undergoing surgery for unilateral The rate of strabismus associated with cataract or bilateral cataract with at least 1 year of in children has been reported to range from follow-up were included. Children with 20.5 to 86%.1 Strabismus is more prevalent in ocular trauma, prematurity, or co-existing children who have been operated for cataract systemic disorders were excluded. The than in the general pediatric population.2–8 following data were evaluated: strabismus Moreover, it occurs more frequently in patients pre- and post-operation; age at surgery; with unilateral than bilateral cataract.1 The post-operative aphakia or pseudophakia; association between timing of surgery or the use and visual acuity. of intra ocular lens (IOL) with development of Results Ninety patients were included, 40% strabismus is still not fully understood. had unilateral and 60% had bilateral cataracts. The main purpose of this study is to evaluate Follow-up was on average 51 months (range: the prevalence and risk factors of strabismus 12–130 months). -

Adult Strabismus Overview Common Types Esotropia Exotropia
Gregory Ostrow, M.D. Scripps Clinic/Scripps Green Hospital Grand Rounds Wednesday, Mar. 18, 2009 Overview • Common Types of Strabismus • Indications for Strabismus Surgery • Common Procedures Adult Strabismus • Psychosocial Benefits Gregory Ostrow M.D Pediatric Ophthalmology and Adult Strabismus Scripps Clinic Medical Group 3811 Valley Centre Drive San Diego, CA 92130 Esotropia Common Types Exotropia www.scripps.org/clinicrss Scripps Conference Services & CME www.scripps.org/conferenceservices 1 P: (858) 652-5400 E: [email protected] Gregory Ostrow, M.D. Scripps Clinic/Scripps Green Hospital Grand Rounds Wednesday, Mar. 18, 2009 • There are many different Indications for Strabismus presentations of strabismus Surgery • Most can be corrected surgically Classically Taught Benefits of Other Benefits Strabismus Surgery • Develop binocular vision • Improve visual • Restore binocular vision field • Eliminate diplopia • Eliminate torticollis www.scripps.org/clinicrss Scripps Conference Services & CME www.scripps.org/conferenceservices 2 P: (858) 652-5400 E: [email protected] Gregory Ostrow, M.D. Scripps Clinic/Scripps Green Hospital Grand Rounds Wednesday, Mar. 18, 2009 Insurance accepted indications Surgical Procedures for strabismus surgery •Diplopia • Weaken (recession) • Asthenopia (eye strain) • Strengthen (resection or tuck) • Any misalignment of the eyes that • Alter vector forces (transposition) cannot be corrected non-surgically – this is where some prodding is occasionally required Recession (weakening) www.scripps.org/clinicrss Scripps Conference Services & CME www.scripps.org/conferenceservices 3 P: (858) 652-5400 E: [email protected] Gregory Ostrow, M.D. Scripps Clinic/Scripps Green Hospital Grand Rounds Wednesday, Mar. 18, 2009 Resection (tightening) Psychosocial Benefits of Strabismus Surgery www.scripps.org/clinicrss Scripps Conference Services & CME www.scripps.org/conferenceservices 4 P: (858) 652-5400 E: [email protected] Gregory Ostrow, M.D.