Improving Vaccination Initiation and Completion Via Vaccine Indicator and Reminder Bands: a Formative Study in Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Print This Article
European Journal of Social Sciences Studies ISSN: 2501-8590 ISSN-L: 2501-8590 Available on-line at: www.oapub.org/soc doi: 10.5281/zenodo.2070313 Volume 3 │ Issue 4 │ 2018 DISTRIBUTION OF PUBLIC WATER SUPPLY: ANALYSIS OF POPULATION DENSITY AND WATER SUPPLY IN KEBBI STATE, NORTHWESTERN NIGERIA Saadu Umar Wali1, Sheikh Danjuma Abubakar2, Ibrahim Mustapha Dankani2i, Murtala Abubakar Gada2 1Department of Geography, Federal University Birnin-kebbi, P.M.B 1157, Kebbi State, Nigeria 2Department of Geography, Usmanu Dan Fodiyo University Sokoto, P.M.B 2346, Sokoto State, Nigeria Abstract: Development and management of an improved water supply system is a great challenge faced by most developing nations. With rapid population growth and urbanization most, states in Nigeria find it difficult to deliver potable water to a substantial number of people who are in dire need for this resource, especially in the Urban areas. In this study, we attempt to relate public water supply to population density in Kebbi State. An inventory of water supply facilities was taken in 21 Local Government Areas (LGAs) in Kebbi State. Census data was collected from the National Population Commission (NPC), Birnin-kebbi. Results showed that, population density correlates very strongly and positively with handpumps (r=0.95), urban schemes (r=0.88), semi-urban schemes (r=0.69) and village scheme (r=0.74). There was a very weak but positive correlation between population density and boreholes (r=<0.001); population density and tabs (r=<0.001). PCA results showed, that the 21 LGAs cluster nicely across a spectrum of public water supply infrastructure. -

To Assess Tree Species Frequency and Density in Bunza Local Government Area of Kebbi State, Nigeria
International Journal of Advanced Academic Research | Agriculture | ISSN: 2488-9849 Vol. 5, Issue 5 (May 2019) TO ASSESS TREE SPECIES FREQUENCY AND DENSITY IN BUNZA LOCAL GOVERNMENT AREA OF KEBBI STATE, NIGERIA. Umar, I.1; Gwimmi, D.P.1;Abdulrahman, A.2 and Wele, H.K.3 1Kebbi State University of Science and Technology, Aliero, Nigeria. 2College of Agriculture and Animal Science, Bakura, Zamfara State, Nigeria. 3College of Agriculture, Zuru, Kebbi State, Nigeria. Correspondence e-mail: [email protected] ABSTRACT The study considered tree species frequency and density in Bunza Local Government Area of Kebbi State, Nigeria. Four villages in Bunza Local Government Area were proportionately selected in the study area. Four sample plots (50m x 50m) were laid at random within the villages, and tree species found were enumerated, a total of 16 villages were sampled. The data was analysed using descriptive statistics. The results indicated that different tree species were identified in the study area, which include Combretum glutonosumr which recorded the highest (36), followed by Azadirachta indica with (23), while Pillostigma thoningii and Hyphaene thebaic (17), and Gmelina arborea and Ziziphus mauritiana recorded the lowest (1). Combretum glutinosum has the highest density of (144/h) across the study area, followed by Azadirachta indica (92/h) density followed by Adansaonia digitata with (60/h) and the trees with lowest density are Ziziphus mauritiana, Gmelina arborea, both with density of (4). The result further explains that Fabaceae family recorded the highest with (5) followed by the family meliaceae, Arecaceae with (2), and the lowest families are Verbenaceae and Rhamnaceae. -
States and Lcdas Codes.Cdr
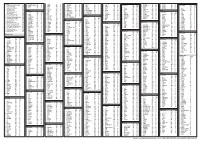
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Increasing Use of Antenatal Care Services Among Women in Kebbi State
Increasing Use of Antenatal Care Services NIGERIA Among Women in Kebbi State The Breakthrough RESEARCH project conducted a behavioral surveillance survey for health among women who had a pregnancy or birth in the previous two years. Survey Findings for Kebbi State The behavioral surveillance survey identified three important factors for improving women’s attendance of antenatal care four or more times (ANC4+) during pregnancy. The percentage in each box below is the median (50th percentile). Half of local government authorities (LGAs) are below (red) and half above this value (green). Women know the benefit of ANC for Women are confident in their ability Women know to attend four or both mother and child to access a health facility for ANC more ANC visits during pregnancy LGAs shaded in LGAs shaded in LGAs shaded in red are below red are below red are below 77% of women 75% of women 34% of women who know the who are who know to benefits of confident in attend four or ANC; green their ability to more ANC areas are access ANC; visits; green above. green areas are areas are above. above. Notes: Lightly shaded areas are immediately below or above the median. Darker shaded areas are further away from the median, below the 25th or above the 75th percentile. LGAs in white were not sampled for the survey and information is not available for these areas. How can this information be used to improve the use of ANC services in Kebbi State? Discussion and inquiry into ANC barriers and facilitators may provide insights on how to enhance efforts in these -

Feed the Future Innovation Lab for Food Security Policy Research Paper 118 September 2018
Feed the Future Innovation Lab for Food Security Policy Research Paper 118 September 2018 Nigeria Agricultural Policy Project THE RAPID TRANSFORMATION OF THE FISH VALUE CHAIN IN NIGERIA: EVIDENCE FROM KEBBI STATE By Ayuba Gona, Gwoni Woji, Sunday Norbert, Hajaru Muhammad, Lenis S. O. Liverpool-Tasie, Thomas Reardon, Ben Belton Food Security Policy Research Papers This Research Paper series is designed to timely disseminate research and policy analytical outputs generated by the USAID funded Feed the Future Innovation Lab for Food Security Policy (FSP) and its Associate Awards. The FSP project is managed by the Food Security Group (FSG) of the Department of Agricultural, Food, and Resource Economics (AFRE) at Michigan State University (MSU), and implemented in partnership with the International Food Policy Research Institute (IFPRI) and the University of Pretoria (UP). Together, the MSU-IFPRI-UP consortium works with governments, researchers and private sector stakeholders in Feed the Future focus countries in Africa and Asia to increase agricultural productivity, improve dietary diversity and build greater resilience to challenges like climate change that affect livelihoods. The papers are aimed at researchers, policy makers, donor agencies, educators, and international development practitioners. Selected papers will be translated into French, Portuguese, or other languages. Copies of all FSP Research Papers and Policy Briefs are freely downloadable in pdf format from the following Web site: www.foodsecuritylab.msu.edu Copies of all FSP -

Alh. Umaru Hakimi Fcfa, Cfa, Cna Auditor General for Local Government Kebbi State
OFFICE OF THE AUDITOR GENERAL FOR LOCAL GOVERNMENTS BIRNIN-KEBBI, KEBBI STATE ANNUAL AUDIT REPORT FOR THE YEAR ENDED 31ST DECEMBER, 2018 IN RESPECT OF THE 21 LOCAL GOVERNMENT COUNCILS IN KEBBI STATE BY ALH. UMARU HAKIMI FCFA, CFA, CNA AUDITOR GENERAL FOR LOCAL GOVERNMENT KEBBI STATE. 1 AUDITOR GENERAL’S OPINION AND CERTIFICATION In compliance with the provision of Section 125(2) of the Constitution of the Federal Republic of Nigeria 1999 and the provision of Section 146 and sub-Section 1-4 of the Kebbi State Local Government Administration Law of 2008. I have obtained all the information and explanations which I considered necessary and therefore certify as result of our audit. In my opinion the Financial Statements and the supporting document have been drawn up so as to show a true and fair view of the state of affairs as at 31st December, 2018 and the transactions for the fiscal year ended on that date as stated above. Therefore, the financial statement has been certified subject to the observations and comments contained in this report. Finally, in my opinion the financial statements and the other related accounts as presented to us give a “True and Fair View” of the state of Affairs of the twenty one (21) Local Governemnt Councils of Kebbi State as at 31st December, 2018. Alh. Umaru Hakimi, FCFA,CFA,CNA. Auditor General for Local Governments Kebbi State. 2 TABLE OF CONTENT 1. Title Page - - - - - - - - 1 2. Auditors General’s opinion and Certification - - 2 3. Table of contents - - - - - - 3 - 4 4. Introduction - - - - - - - 5 - 12 5. -

An Evaluation of the Suitability of Ceramic Raw Materials in Kebbi State for the Production of Tableware for Small Scale Industry
AN EVALUATION OF THE SUITABILITY OF CERAMIC RAW MATERIALS IN KEBBI STATE FOR THE PRODUCTION OF TABLEWARE FOR SMALL SCALE INDUSTRY BY ZAURO, TUKUR DIKKO MUHAMMAD A DISSERTATION SUBMITTED TO THE POSTGRADUATE SCHOOL IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE AWARD OF THE DEGREE OF DOCTOR OF PHILOSOPHY IN INDUSTRIAL DESIGN DEPARTMENT OF INDUSTRIAL DESIGN FACULTY OF ENVIRONMENTAL DESIGN AHMADU BELLO UNIVERSITY ZARIA NIGERIA. DECEMBER, 2007 i DECLARATION I declare that the work in the dissertaton entitled “An evaluation of the Suitability of Ceramic Raw Materials in Kebbi State for the Production of Tableware for Small Scale Industry” has been performed by me in the Department of Industrial Design under the supervision of Professor A. M. Ahuwan, Professor B.A. Kparevzua and Dr. Salihu Maiwada. The information derived from the literature has been duly acknowledged in the text and a list of references provided. No part of this dissertation was previously presented for another degree or diploma at any university. ____________________________ _______________ Zauro, Tukur Dikko Muhammad Date ii CERTIFICATION This dissertation entitled “AN EVALUATION OF THE SUITABILITY OF CERAMIC RAW MATERIALS IN KEBBI STATE FOR THE PRODUCTION OF TABLEWARE FOR SMALL SCALE INDUSTRY” by Zauro, Tukur Dikko Muhammad meets the regulations governing the award of the degree of Doctor of Philosophy in Industrial Design of Ahmadu Bello University, Zaria and is approved for its contribution to knowledge and literary presentation ________________________ __________________ Professor A. M. Ahuwan Date Chairman, Supervisory Committee ________________________ __________________ Professor B. A. Kparevzua Date Member, Supervisory Committee ________________________ __________________ Dr. Salihu Maiwada Date Member, Supervisory Committee ________________________ __________________ Dr. -

Increasing Use of Antenatal Care Services Among Women in Kebbi State
Population Council Knowledge Commons Reproductive Health Social and Behavioral Science Research (SBSR) 11-1-2020 Increasing use of antenatal care services among women in Kebbi State Breakthrough RESEARCH Follow this and additional works at: https://knowledgecommons.popcouncil.org/departments_sbsr-rh How does access to this work benefit ou?y Let us know! Recommended Citation Breakthrough RESEARCH. 2020. "Increasing use of antenatal care services among women in Kebbi State," infographic. Washington, DC: Population Council. This Brief is brought to you for free and open access by the Population Council. Increasing Use of Antenatal Care Services NIGERIA Among Women in Kebbi State The Breakthrough RESEARCH project conducted a behavioral surveillance survey for health among women who had a pregnancy or birth in the previous two years. Survey Findings for Kebbi State The behavioral surveillance survey identified three important factors for improving women’s attendance of antenatal care four or more times (ANC4+) during pregnancy. The percentage in each box below is the median (50th percentile). Half of local government authorities (LGAs) are below (red) and half above this value (green). Women know the benefit of ANC for Women are confident in their ability Women know to attend four or both mother and child to access a health facility for ANC more ANC visits during pregnancy LGAs shaded in LGAs shaded in LGAs shaded in red are below red are below red are below 77% of women 75% of women 34% of women who know the who are who know to benefits of confident in attend four or ANC; green their ability to more ANC areas are access ANC; visits; green above. -

Nigeria Security Situation
Nigeria Security situation Country of Origin Information Report June 2021 More information on the European Union is available on the Internet (http://europa.eu) PDF ISBN978-92-9465-082-5 doi: 10.2847/433197 BZ-08-21-089-EN-N © European Asylum Support Office, 2021 Reproduction is authorised provided the source is acknowledged. For any use or reproduction of photos or other material that is not under the EASO copyright, permission must be sought directly from the copyright holders. Cover photo@ EU Civil Protection and Humanitarian Aid - Left with nothing: Boko Haram's displaced @ EU/ECHO/Isabel Coello (CC BY-NC-ND 2.0), 16 June 2015 ‘Families staying in the back of this church in Yola are from Michika, Madagali and Gwosa, some of the areas worst hit by Boko Haram attacks in Adamawa and Borno states. Living conditions for them are extremely harsh. They have received the most basic emergency assistance, provided by our partner International Rescue Committee (IRC) with EU funds. “We got mattresses, blankets, kitchen pots, tarpaulins…” they said.’ Country of origin information report | Nigeria: Security situation Acknowledgements EASO would like to acknowledge Stephanie Huber, Founder and Director of the Asylum Research Centre (ARC) as the co-drafter of this report. The following departments and organisations have reviewed the report together with EASO: The Netherlands, Ministry of Justice and Security, Office for Country Information and Language Analysis Austria, Federal Office for Immigration and Asylum, Country of Origin Information Department (B/III), Africa Desk Austrian Centre for Country of Origin and Asylum Research and Documentation (ACCORD) It must be noted that the drafting and review carried out by the mentioned departments, experts or organisations contributes to the overall quality of the report, but does not necessarily imply their formal endorsement of the final report, which is the full responsibility of EASO. -
Constitution of the Federal Republic of Nigeria 1999 Chapter I Chapter II
Constitution of the Federal Republic of Nigeria 1999 Arrangement of sections Chapter I General Provisions Part I Federal Republic of Nigeria 1. Supremacy of constitution. 2 The Federal Republic of 3 States of the Federation and the Nigeria. Federal Capital Territory, Abuja. Part II Powers of the Federal Republic of Nigeria 4. Legislative powers. 5 Executive powers. 6 Judicial powers 7. Local government system. 8 New states and boundary 9 Mode of altering provisions of the adjustment, etc. constitution 10. Prohibition of State Religion. 11 Public order and public security. 12 Implementation of treaties. Chapter II Fundamental Objectives and directive Principles of State Policy 13. Fundamental obligations of the 14 The Government and the people 15 Political objectives. Government. 16. Economic objectives. 17 Social objectives. 18 Educational objectives. 19. Foreign policy objectives. 20. Environmental objectives. 21. Directive on Nigeria cultures 22. Obligation of the mass media 23. National ethics. 24. Duties of the citizen. Chapter III Citizenship 25. Citizenship by birth. 26 Citizenship by registration. 27 Citizenship by naturalisation. 28. Dual citizenship. 29 Renunciation of citizenship. 30 Deprivation of citizenship. 31. Persons deemed to be Nigerian 32 Power to make regulations. citizens. Chapter IV Fundamental Rights 33. Right to life. 34 Right to dignity of human 35 Right to personal liberty. persons. 36. Right to fair hearing. 37 Right to private and family life. 38 Right to freedom of thought, conscience and religion 39. Right to freedom of expression 40 Right to peaceful assembly and 41 Right to freedom of movement. and the press. association. 42 Right to freedom from 43 Right to acquire and own 44 Compulsory acquisition of property. -

NIGERIA-Sokotostate
For Humanitarian Purposes Only LOGISTICS ACCESS NIGERIA - Sokoto State Production date : 17 Feb 2021 AND SECURITY PLANNING MAPAs of February 2021 WURNO Sokoto State KWARE SOKOTO NORTH Niger Sokoto SOKOTO SOUTH WAMAKO Rafinduma Salo DANGE-SHUNI Zenge Dan Gode Gidan Kiriya Lafani Hill Sokoto City Hasamawa Gidan Kwanni 0 2.5 5km Djima-Djimi Roga Lungusi Gaya BODINGA Manja Illela Danboka Gada Gidan Fako Gidan Gidi Gobir Munwadata ILLELA Koringo GADA Labau Gardau Tozai Hill Gidan Fulani Sadura Masalawan Kuruhi Maradi, Duchi Madawal Tudumasana Native Goulbi m- Awulkite Kamdan Dantudu Area* Horgoma Hills Rangandawa Tungan Zango Kaideji Gidan Gwayo Gwadi Mulawa Makina Fadama Kiri Badarawa Tambuje Dakura Magagindoke Wayage Tunga Ilo Dumaji TANGAZA Damba Diko Sabon Birni Tajaye Sudiundu, Gingu Gidan Shibkau Gidan Rahi Gidan Barau Takau Buwadi River Dangkusot Gohono Jebba Gidan Kaukau Madugu Gidan MallamTsitse Darbabiya Gauro Yerimawa Gidan Busel SABON BIRNI Balle Bamana, River Birjingo Tungan-Dulu Kure Kolo Nadindu Sinkafatu, Dambagi Tungan Haruna Kojio Beriberi Saina Raka Birni River Goronyo Mahalba GUDU Tunga Madugu Dabwasa Gabare Goronyo Bilingawa Meli Bachaka Boto Ere GWADABAWA Kue Hill GORONYO Madarari Yalao Tangaza Gadon Mata Alela Gwadabawa Gidan-Alamu Bierda Makwia Kangiye Dimbisu Ihi Tungan Yusufu Gonyel Tungan Ibru Saraku Tunga-Yusufu Malamawa Wurno Arba Koliyal Rumbuki Kalanjene Lukwa Jingini WURNO Mallamawa Karfe Binji Kiriya Maburgami Tunga-Dankemo Masama Rujin Tsamia Native Kabawa Toidi Zaidi Kulhi Sidingu Kware Dabagi Bum ISA Rikaka