Fracture Management Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

MARCH FRACTURE-PIED FORCE Developed Reactions to These Test Products and to Witte Peptone at Least As Severe As Those Shown by Our by Anaphylactic Case
FEB. 24, 1940 ANAPHYLAXIS AFTER TETANUS TOXOID MERCALTSORHL 95 erythema than similar dilutions of the extracts, and that within a few minutes of injection many persons MARCH FRACTURE-PIED FORCE developed reactions to these test products and to Witte peptone at least as severe as those shown by our BY anaphylactic case. Further investigations are in progress which it is hoped will be the subject of another paper. F. A. R. STAMMERS, Ch.M., F.R.C.S. Our observations throw considerable doubt on the value Major R.A.M.C., Surgical Specialist of scratch and intradermal tests as usually interpreted on the basis of early readings. Nevertheless, our patient Army medical officers everywhere have been asked to see was the only subject who developed mild anaphylactic all sorts of foot troubles precipitated by military training. symptoms-itching of the nose and tongue, slight swelling More often than not these are due to pre-existing con- of the lower lip, smarting of the eyes, and flushing of the ditions such as hallux rigidus, hallux valgus, hammer-toe, face-soon after 1 in 1,000 dilutions of Witte peptone and or pes planus, which, though formerly symptomless, break two other beef fibrin digests had been injected intra- down under the strain of route-marching, physical train- dermally; and she alone showed areas of redness, 50 to ing, and the general extra footwork the soldier- is called 60 mm. in diameter, swelling, and induration (" like upon to do in heavy army boots. Even a seemingly those occurring after staphylococcus toxoid ") about two normal foot may develop trouble under such circum- hours later at the sites of injection of these products. -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -

BSUH VFC Initial Management Guidelines Dec 2014
BSUH VFC initial management guidelines Dec 2014 Contents Page Elbow injuries: Radial head / Radial neck fractures 3 Elbow dislocations 3 Shoulder Injuries: Shoulder dislocation 4 ACJ dislocation 4 Proximal Humerus fractures 5 Greater Tuberosity fractures 5 Midshaft Humerus 6 Mid-shaft clavicle fractures 7 Lateral 1/3 Clavicle fractures 8 Medial 1/3 clavicle fractures 9 Soft tissue injury shoulder 11 Calcific tendinitis 11 Common lower limb injuries Foot injuries: 5th Metatarsal fracture 12 Stress fractures 12 5th Midshaft fractures 12 Single Metatarsal fractures 12 Single phalanx fractures 12 Multiple Metatarsal fractures 13 Mid-foot fractures 13 Calcaneal fractures 14 Ankle injuries: Page 1 of 18 Weber A ankle fractures 15 Weber B 15 Weber C 15 Medial malleolus / and Posterior malleolus fractures 15 Bi-tri malleolus fractures 16 Soft tissue ankle injury / Avulsion lateral malleolus 16 TA ruptures 16 Knee injuries Locked Knee 17 Soft tissue knee injury 17 Patella Dislocation 17 Patella fractures 17 Possible Tumours 18 Page 2 of 18 Upper Limb Injuries Elbow injuries Radial head / neck fractures Mason 1 head / borderline Mason 1-2 protocol BAS for comfort only 2/52 and early gentle ROM DC VFC. Patient to contact VFC at 3/52 post injury if struggling to regain ROM Mason 2 >2mm articular step off discuss case with consultant on hot week likely conservative management if unsure d/w upper limb consultants opinion for 2/52 repeat x-ray and review in VFC Mason 3 head # or >30degrees neck angulation = Urgent Ref to UL clinic (LL or LT) for discussion with regards to surgical management. -

Listen to the Associated Podcast Episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, Available at Theradiologyreview.Com O
MSK: Fractures for Radiology Board Study, Matt Covington, MD Listen to the associated podcast episodes: MSK: Fractures for the ABR Core Exam Parts 1-3, available Listen to associated Podcast episodes: ABR Core Exam, Multisystemic Diseases Parts 1-3, available at at theradiologyreview.com or on your favorite podcast directory. Copyrighted. theradiologyreview.com or on your favorite podcast direcry. Fracture resulting From abnormal stress on normal bone = stress Fracture Fracture From normal stress on abnormal bone = insuFFiciency Fracture Scaphoid Fracture site with highest risk for avascular necrosis (proximal or distal)? Proximal pole scaphoid Fractures are at highest risk For AVN Comminuted Fracture at the base oF the First metacarpal = Rolando Fracture Non-comminuted Fracture at base oF the First metacarpal = Bennett Fracture The pull oF which tendon causes the dorsolateral dislocation in a Bennett fracture? The abductor pollicus longus tendon. Avulsion Fracture at the base oF the proximal phalanx with ulnar collateral ligament disruption = Gamekeeper’s thumb. Same Fracture but adductor tendon becomes caught in torn edge oF the ulnar collateral ligament? Stener’s lesion. IF Stener’s lesion is present this won’t heal on its own so you need surgery. You shouldn’t image a Gamekeeper’s thumb with stress views because you can convert it to a Stener’s lesion. Image with MRI instead. Distal radial Fracture with dorsal angulation = Colle’s Fracture (C to D= Colle’s is Dorsal) Distal radial Fracture with volar angulation = Smith’s Fracture (S -

WHO Manual of Diagnostic Imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System
The WHO manual of diagnostic imaging Radiographic Anatomy and Interpretation of the Musculoskeletal System Editors Harald Ostensen M.D. Holger Pettersson M.D. Authors A. Mark Davies M.D. Holger Pettersson M.D. In collaboration with F. Arredondo M.D., M.R. El Meligi M.D., R. Guenther M.D., G.K. Ikundu M.D., L. Leong M.D., P. Palmer M.D., P. Scally M.D. Published by the World Health Organization in collaboration with the International Society of Radiology WHO Library Cataloguing-in-Publication Data Davies, A. Mark Radiography of the musculoskeletal system / authors : A. Mark Davies, Holger Pettersson; in collaboration with F. Arredondo . [et al.] WHO manuals of diagnostic imaging / editors : Harald Ostensen, Holger Pettersson; vol. 2 Published by the World Health Organization in collaboration with the International Society of Radiology 1.Musculoskeletal system – radiography 2.Musculoskeletal diseases – radiography 3.Musculoskeletal abnormalities – radiography 4.Manuals I.Pettersson, Holger II.Arredondo, F. III.Series editor: Ostensen, Harald ISBN 92 4 154555 0 (NLM Classification: WE 141) The World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and enquiries should be addressed to the Office of Publications, World Health Organization, CH-1211 Geneva 27, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2002 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. -

Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015
1 Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015 2 Lunchtime Drop-in Sessions The Library and Information Service provides free specialist information skills training for all UHBristol staff and students. To book a place, email: [email protected] If you’re unable to attend we also provide one-to-one or small group sessions. Contact library@ or katie.barnard@ to arrange a session. Literature Searching October (12pm) An in -depth guide on how to search Thurs 8th Statistics the evidence base, including an introduction to UpToDate and Fri 16th Literature Searching Anatomy.tv. Mon 19th Understanding articles Tues 27th Statistics Useful for anybody who wants to find the best and quickest way to source articles. November (1pm) Weds 4th Literature Searching Thurs 12th Understanding articles How to understand an article Fri 20th Statistics How to assess the strengths and Mon 23rd Literature Searching weaknesses of published articles. Examining bias and validity. December (12pm) Tues 1st Understanding articles Weds 9th Statistics Medi cal Statistics Thurs 17th Literature Searching A basic introduction to the key statistics in medical articles. Giving an overview of statistics that compare risk, test confidence, analyse clinical investigations, and test difference. 3 Contents Contents .................................................................................................................................................. 3 New from Cochrane Database of Systematic Reviews .......................................................................... -

Radial Head Fractures Treated with Open Reduction and Internal Fixation
Moghaddam et al. Trauma Cases Rev 2016, 2:028 Volume 2 | Issue 1 ISSN: 2469-5777 Trauma Cases and Reviews Research Article: Open Access Radial Head Fractures Treated with Open Reduction and Internal Fixation Moghaddam A1*, Raven TF1, Kaghazian P1, Studier-Fischer S2, Swing T1, Grützner PA2 and Biglari B2 1Trauma & Reconstructive Surgery, University hospital Heidelberg, Germany 2BG Unfallklinik, Ludwigshafen, Germany *Corresponding author: Prof. Dr. med. Arash Moghaddam, Consultant Orthopaedic & Trauma Surgeon Center of Trauma, Orthopaedics & Paraplegiology, Division of Trauma & Reconstructive Surgery, University hospital Heidelberg, Schlierbacher Landstraße 200a, 69118 Heidelberg, Germany, Tel: 0049-6221-5626263, Fax: 0049- 6221-26298, E-mail: [email protected] to a high percentage of associated injuries [6]. The combination of a Abstract dislocated fracture and unstable joint makes operative treatment as Background: Radial head fractures are responsible for 2 to 5% of well as early mobilization difficult. Other treatment options include adult fractures. Especially problematic is the treatment of dislocated the implantation of a radial head prosthesis and resection of the and unstable fractures which often have a worst prognosis. The radial head. The radial head prosthesis has become established as the purpose of this study was to evaluate the results of open reduction choice of treatment for multi-fragmented radial head fractures with and internal fixation (ORIF) in the treatment of radial head fractures. associated injuries, while resection of the radial head has increasingly Materials and Methods: Between June 2001 and January 2006, fallen out of use and is now reserved for isolated fractures of the 41 reconstructive surgical procedures were executed. Thirty-seven radial head without associated injuries [7]. -

Del Vecchio Upper Extremity Injury
UPPER EXTREMITY INJURIES Jeff Del Vecchio MPAS, PA-C, DFAAPA Mercy Clinic Orthopedics Springfield, Missouri OBJECTIVES IDENTIFY COMMON UPPER EXTREMITY INJURIES AND FRACTURES REVIEW EXAMINATION TECHNIQUES FOR COMMON UPPER EXTREMITY INJURIES DISCUSS AND REVIEW RADIOGRAPHIC FINDINGS OF UPPER EXTREMITY FRACTURES DISCUSS AND REVIEW TREATMENT OPTIONS FOR COMMON UPPER EXTREMITY INJURIES LATERAL EPICONDYLITIS Tennis elbow Definition Pain about lateral aspect of elbow Involves extensor musculature Rotation of arm and wrist extension Secondary to repetitive overuse or injury Microtears to tendon⇒ inflammation⇒fibrosis⇒degeneration Affects pt’s 30-60 yrs Clinical symptoms Outside elbow and back of upper forearm pain Pain lifting with palm facing down Holding lightweight objects difficult Physical Examination Lateral epicondylar area tender to palpation Tennis elbow test- elbow 90 deg, extend wrist against resistance. +pain at lateral epicondaylar area Radiographs Obtain to rule out osteoarthritis or calcifications Treatment NSAID’s (10-14 days) Avoid activities causing pain Heat or ice Corticosteroid injection Stretching and gradual strengthening program Tennis elbow strap MEDIAL EPICONDYLITIS Golfer’s elbow Definition Inflammation of flexor-pronator’s Less common than lateral epicondylitis Clinical Symptoms Medial elbow pain Physical Examination Pain with palpation over medial condyle Pain with flexion and pronation of wrist against resistance Rule out ulnar neuropathy Treatment Same as lateral epicondylitis CLAVICLE FRACTURE Most common bone injury -
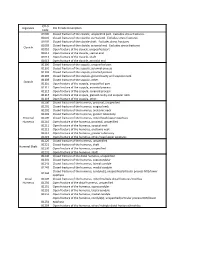
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,Fracture,Of,The,Clavicle,,Unspecified,Part.,,Excludes,Stress,Fractures
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,fracture,of,the,clavicle,,unspecified,part.,,Excludes,stress,fractures. 81001 Closed,fracture,of,the,clavicle,,sternal,end.,,Excludes,stress,fractures. 81002 Closed,fracture,of,the,clavicle,shaft.,,Excludes,stress,fractures. 81003 Closed,fracture,of,the,clavicle,,acromial,end.,,Excludes,stress,fractures. Clavicle 81010 Open,fracture,of,the,clavicle,,unspecified,part 81011 Open,fracture,of,the,clavicle,,sternal,end 81012 Open,fracture,of,the,clavicle,,shaft 81013 Open,fracture,of,the,clavicle,,acromial,end 81100 Closed,fracture,of,the,scapula,,unspecified,part 81101 Closed,fracture,of,the,scapula,,acromial,process 81102 Closed,fracture,of,the,scapula,,coracoid,process 81103 Closed,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81109 Closed,fracture,of,the,scapula,,other. Scapula 81110 Open,fracture,of,the,scapula,,unspecified,part 81111 Open,fracture,of,the,scapula,,acromial,process 81112 Open,fracture,of,the,scapula,,coracoid,process 81113 Open,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81119 Open,fracture,of,the,scapula,,other. 81200 Closed,fracture,of,the,humerus,,proximal,,unspecified 81201 Closed,fracture,of,the,humerus,,surgical,neck 81202 Closed,fracture,of,the,humerus,,anatomic,neck 81203 Closed,fracture,of,the,humerus,,greater,tuberosity Proximal, 81209 Closed,fracture,of,the,humerus,,other/head/upper,epiphysis Humerus 81210 Open,fracture,of,the,humerus,,proximal,,unspecified 81211 Open,fracture,of,the,humerus,,surgical,neck 81212 Open,fracture,of,the,humerus,,anatomic,neck -
Radial Head Fracture Repair and Rehabilitation
1 Radial Head Fracture Repair and Rehabilitation Surgical Indications and Considerations Anatomical Considerations: The elbow is a complex joint due to its intricate functional anatomy. The ulna, radius and humerus articulate in such a way as to form four distinctive joints. Surrounding the osseous structures are the ulnar collateral ligament complex, the lateral collateral ligament complex and the joint capsule. Four main muscle groups provide movement: the elbow flexors, the elbow extensors, the flexor-pronator group, and the extensor-supinator groups. Different types of radial head fractures can occur each of which has separate surgical indications and considerations. Fractures of the proximal one-third of the radius normally occur in the head region in adults and in neck region in children. The most recognized and used standard for assessing radial head fractures is the 4-part Mason classification system. It is used for both treatment and prognosis. Classification: Type I fracture A fissure or marginal fracture without displacement. Type II fracture Marginal fractures with displacement involving greater than 2 mm displacement. Type III fracture Comminuted fractures of the whole radial head. Type IV fracture (variation) A comminuted fracture, with an associated dislocation, ligament injury, coronoid fracture, or Monteggia lesion. Pathogenesis: Severe comminuted fractures or fracture dislocations of the head of the radius often occur as the result of a fall on an outstretched arm with the distal forearm angled laterally, or a valgus stress on the elbow. Fractures can also occur from a direct blow or force to the elbow (e.g. MVA). Chronic synovitis and mild deterioration of the articular surfaces associated with arthritis (e.g.