Conquest Summer 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2016 Joint Meeting Program
April 15 – 17, 2016 Fairmont Chicago Millennium Park • Chicago, Illinois The AAP/ASCI/APSA conference is jointly provided by Boston University School of Medicine and AAP/ASCI/APSA. Meeting Program and Abstracts www.jointmeeting.org www.jointmeeting.org Special Events at the 2016 AAP/ASCI/APSA Joint Meeting Friday, April 15 Saturday, April 16 ASCI President’s Reception ASCI Food and Science Evening 6:15 – 7:15 p.m. 6:30 – 9:00 p.m. Gold Room The Mid-America Club, Aon Center ASCI Dinner & New Member AAP Member Banquet Induction Ceremony (Ticketed guests only) (Ticketed guests only) 7:00 – 10:00 p.m. 7:30 – 9:45 p.m. Imperial Ballroom, Level B2 Rouge, Lobby Level How to Solve a Scientific Puzzle: Speaker: Clara D. Bloomfield, MD Clues from Stockholm and Broadway The Ohio State University Comprehensive Cancer Center Speaker: Joe Goldstein, MD APSA Welcome Reception & University of Texas Southwestern Medical Center at Dallas Presidential Address APSA Dinner (Ticketed guests only) 9:00 p.m. – Midnight Signature Room, 360 Chicago, 7:30 – 9:00 p.m. John Hancock Center (off-site) Rouge, Lobby Level Speaker: Daniel DelloStritto, APSA President Finding One’s Scientific Niche: Musings from a Clinical Neuroscientist Speaker: Helen Mayberg, MD, Emory University Dessert Reception (open to all attendees) 10:00 p.m. – Midnight Imperial Foyer, Level B2 Sunday, April 17 APSA Future of Medicine and www.jointmeeting.org Residency Luncheon Noon – 2:00 p.m. Rouge, Lobby Level 2 www.jointmeeting.org Program Contents General Program Information 4 Continuing Medical Education Information 5 Faculty and Speaker Disclosures 7 Scientific Program Schedule 9 Speaker Biographies 16 Call for Nominations: 2017 Harrington Prize for Innovation in Medicine 26 AAP/ASCI/APSA Joint Meeting Faculty 27 Award Recipients 29 Call for Nominations: 2017 Harrington Scholar-Innovator Award 31 Call for Nominations: George M. -
Appendix Program Managers/Acknowledgments
Flight Information Appendix Program Managers/Acknowledgments Selected Readings Acronyms Contributors’ Biographies Index Image of a Legac y—The Final Re-entry Appendix 517 Flight Information Approx. Orbiter Enterprise STS Flight No. Orbiter Crew Launch Mission Approach and Landing Test Flights and Crew Patch Name Members Date Days 1 Columbia John Young (Cdr) 4/12/1981 2 Robert Crippen (Plt) Captive-Active Flights— High-speed taxi tests that proved the Shuttle Carrier Aircraft, mated to Enterprise, could steer and brake with the Orbiter perched 2 Columbia Joe Engle (Cdr) 11/12/1981 2 on top of the airframe. These fights featured two-man crews. Richard Truly (Plt) Captive-Active Crew Test Mission Flight No. Members Date Length 1 Fred Haise (Cdr) 6/18/1977 55 min 46 s Gordon Fullerton (Plt) 2 Joseph Engle (Cdr) 6/28/1977 62 min 0 s 3 Columbia Jack Lousma (Cdr) 3/22/1982 8 Richard Truly (Plt) Gordon Fullerton (Plt) 3 Fred Haise (Cdr) 7/26/1977 59 min 53 s Gordon Fullerton (Plt) Free Flights— Flights during which Enterprise separated from the Shuttle Carrier Aircraft and landed at the hands of a two-man crew. 4 Columbia Thomas Mattingly (Cdr) 6/27/1982 7 Free Flight No. Crew Test Mission Henry Hartsfield (Plt) Members Date Length 1 Fred Haise (Cdr) 8/12/1977 5 min 21 s Gordon Fullerton (Plt) 5 Columbia Vance Brand (Cdr) 11/11/1982 5 2 Joseph Engle (Cdr) 9/13/1977 5 min 28 s Robert Overmyer (Plt) Richard Truly (Plt) William Lenoir (MS) 3 Fred Haise (Cdr) 9/23/1977 5 min 34 s Joseph Allen (MS) Gordon Fullerton (Plt) 4 Joseph Engle (Cdr) 10/12/1977 2 min 34 s Richard Truly (Plt) 5 Fred Haise (Cdr) 10/26/1977 2 min 1 s 6 Challenger Paul Weitz (Cdr) 4/4/1983 5 Gordon Fullerton (Plt) Karol Bobko (Plt) Story Musgrave (MS) Donald Peterson (MS) The Space Shuttle Numbering System The first nine Space Shuttle flights were numbered in sequence from STS -1 to STS-9. -

Robert Satcher, MD, Phd Obert L
Robert Satcher, MD, PhD obert L. Satcher, Jr., MD, PhD is recognized for his varied career interests Orthopaedic Oncology Surgeon, Astronaut and Engineer and notable successes. Born September 22, 1965 in Hampton, Virginia, he rgraduated from Denmark-Olar High School in Denmark, South Carolina in 1982; earned a Bachelor of Science Degree in 1986, a PhD in chemical engineering in 1993 from the Massachusetts Institute of Technology (MIT); and an MD from Harvard Medical School in 1994. Satcher served as an assistant professor of orthopaedic surgery and adjunct professor in Biomedical Engineering at Northwestern University. He was accepted into the astronaut candidate training program by NASA and in 2009 made his first trip to space aboard the space shuttle Atlantis, during which he completed two spacewalks. In 2011, he returned to clinical practice at the M.D. Anderson Cancer Center in Houston, Texas. His work at M.D. Anderson includes a Global Oncology project, with plans to build a Cancer Center in sub-Saharan Africa. He received an AT&T grant to extend M.D. Anderson’s specialized surgical expertise to rural and underserved communities. Satcher co-founded the Telehealth Research Institute, a collaborative endeavor between Rice University, the National Space Biomedical Research Institute, and M.D. Anderson, to create a consortium of physicians with academic and industry researchers to improve access to specialized health care by pairing the latest in research and technology for the remote delivery of medical services. He is a member of several organizations, including the American Academy of Orthopaedic Surgery, Doctors United in Medical Missions, and the National Comprehensive Cancer Network. -

Biographical Description for the Historymakers® Video Oral History with Dr
Biographical Description for The HistoryMakers® Video Oral History with Dr. Robert Satcher, Jr. PERSON Satcher, Robert Lee, Jr., 1965- Alternative Names: Dr. Robert Satcher, Jr.; Bobby Life Dates: September 22, 1965- Place of Birth: Hampton, Virginia, USA Residence: Bellaire, TX Work: Houston, TX Occupations: Orthopedic Surgeon; Chemical Engineer; Astronaut Biographical Note Orthopaedic surgeon, chemical engineer and astronaut Robert Lee Satcher, Jr. was born on September 22, 1965 in Hampton, Virginia to Robert and Marian Satcher. Satcher graduated from Denmark-Olar High School in Denmark, South Carolina, in 1982. He received his B.S. degree in chemical engineering from Massachusetts Institute of Technology (MIT) in 1986; his Ph.D. degree in chemical engineering from MIT in his Ph.D. degree in chemical engineering from MIT in 1993; and his M.D. degree from Harvard Medical School in 1994. Satcher completed his postdoctoral research fellowships at MIT in 1994 and University of California, Berkeley in 1998; internship and residency in orthopaedic surgery at the University of California, San Francisco in 2000; and a fellowship in musculoskeletal oncology at the University of Florida in 2001. From 2001 to 2008, Satcher served as an assistant professor at The Feinberg School of Medicine at Northwestern University, in the Department of Orthopaedic Surgery. He was also an assistant professor of orthopaedic surgery at the Children's Memorial Hospital in Chicago, Illinois from 2001 to 2008, and served as a professor at the Institute for Bionanotechnology in Medicine at Northwestern University Medical Center. In addition, Satcher was an attending physician of orthopaedic oncology at Northwestern Memorial Hospital - Robert H. -

Walking to Olympus: an EVA Chronology, 1997–2011 Volume 2
VOLUME 2 Robert C. Treviño Julie B. Ta MONOGRAPHS AEROSPACE IN HISTORY, 50 NO. AN EVA CHRONOLOGY, 1997–2011 AN CHRONOLOGY, EVA WALKING TO OLYMPUS WALKING WALKING TO OLYMPUS AN EVA CHRONOLOGY, 1997–2011 VOLUME 2 Ta I Treviño NASA SP-2016-4550 WALKING TO OLYMPUS AN EVA CHRONOLOGY, 1997–2011 VOLUME 2 Julie B. Ta Robert C. Treviño MONOGRAPHS IN AEROSPACE HISTORY SERIES #50 APRIL 2016 National Aeronautics and Space Administration NASA History Program Office Public Outreach Division Office of Communications NASA Headquarters Washington, DC 20546 NASA SP-2016-4550 Library of Congress Cataloging-in-Publication Data Ta, Julie B., author. Walking to Olympus: an EVA chronology, 1997–2011 / by Julie B. Ta and Robert C. Treviño. – Second edition. pages cm. – (Monographs in aerospace history series; #50) “April 2016.” Continuation of: Walking to Olympus / David S.F. Portree and Robert C. Treviño. 1997. “NASA SP-2015-4550.” Includes bibliographical references and index. 1. Extravehicular activity (Manned space flight)–History–Chronology. I. Treviño, Robert C., author. II. Title. TL1096.P67 2015 629.45’84–dc23 2015030907 ON THE COVER Astronaut Steve Robinson, anchored to a foot restraint on the International Space Station’s Canadarm2, participates in the STS-114 mission’s third spacewalk. Robinson holds a digital still camera, updated for use on spacewalks, in his left hand. (NASA S114e6651) This publication is available as a free download at http://www.nasa.gov/ebooks. CONTENTS Foreword . v Introduction . .vii The Chronology . 1 1997 1 1998 7 1999 15 2000 21 2001 29 2002 41 2003 55 2004 57 2005 61 2006 67 2007 77 2008 93 2009 107 2010 121 2011 133 Acronyms and Abbreviations . -

Bulletin April 2010
APRIL 2010 Volume 95, Number 4 FEATURES Stephen J. Regnier Surgical lifestyles: An orthopaedic surgeon in space: Editor An interview with Robert Satcher, MD, PhD 11 Linn Meyer Tony Peregrin Director, Division of Rural surgeons—We must grow our own 16 Integrated Communications Paul J. Huffstutter, MD, FACS Tony Peregrin Associate Editor Rural surgeons—We must grown our own: A response 19 Joseph B. Cofer, MD, FACS Diane S. Schneidman Contributing Editor Medicare physician reimbursement: Is the SGR’s end in sight? 20 Tina Woelke Shawn Friesen Graphic Design Specialist Alden H. Harken, Is the generalist surgeon obsolete? The impact of the general surgeon shortage on global health 24 MD, FACS Jeremy Hedges, MD, MPH; Kimberly A. Ruscher, MD, MPH; Charles D. Mabry, and Kathryn Chu, MD, MPH MD, FACS Jack W. McAninch, MD, FACS Editorial Advisors DEPARTMENTS Tina Woelke Front cover design Looking forward 4 Editorial by David B. Hoyt, MD, FACS, ACS Executive Director Future meetings What surgeons should know about... 6 Clinical Congress PQRI reporting in 2010 2010 Washington, DC, Caitlin Burley October 3-7 Advocacy advisor 27 2011 San Francisco, CA, Lobbyists—Who needs them? October 23-27 Melinda Baker 2012 Chicago, IL, September 30– October 4 Letters to the Editor should be sent with the writer’s name, address, e-mail ad- dress, and daytime tele- phone number via e-mail to [email protected], or via mail to Stephen J. Regnier, Editor, Bulletin, American College of Surgeons, 633 N. Saint Clair St., Chicago, IL 60611. Letters may be edited for length or On the cover: Last year, Robert Satcher, MD, PhD, became the first orthopaedic clarity. -

Space Reporter's Handbook Mission Supplement
CBS News Space Reporter's Handbook - Mission Supplement! Page 1 The CBS News Space Reporter's Handbook Mission Supplement Shuttle Mission STS-129/ISS-ULF 3: Spares for the International Space Station Written and Produced By William G. Harwood CBS News Space Analyst [email protected] CBS News!!! 11/12/09 Page 2 ! CBS News Space Reporter's Handbook - Mission Supplement Revision History Editor's Note Mission-specific sections of the Space Reporter's Handbook are posted as flight data becomes available. Readers should check the CBS News "Space Place" web site in the weeks before a launch to download the latest edition: http://www.cbsnews.com/network/news/space/current.html DATE RELEASE NOTES 11/12/09 Initial STS-129 release Introduction This document is an outgrowth of my original UPI Space Reporter's Handbook, prepared prior to STS-26 for United Press International and updated for several flights thereafter due to popular demand. The current version is prepared for CBS News. As with the original, the goal here is to provide useful information on U.S. and Russian space flights so reporters and producers will not be forced to rely on government or industry public affairs officers at times when it might be difficult to get timely responses. All of these data are available elsewhere, of course, but not necessarily in one place. The STS-129 version of the CBS News Space Reporter's Handbook was compiled from NASA news releases, JSC flight plans, the Shuttle Flight Data and In-Flight Anomaly List, NASA Public Affairs and the Flight Dynamics office (abort boundaries) at the Johnson Space Center in Houston. -
Space Shuttle Missions Summary - Book 2 Sts- 97 Through Sts-131 Revision T Pcn-5 June 2010
SPACE SHUTTLE MISSIONS SUMMARY - BOOK 2 STS- 97 THROUGH STS-131 REVISION T PCN-5 JUNE 2010 Authors: DA8/Robert D. Legler & DA8/Floyd V. Bennett Book Manager: DA8/Mary C. Thomas 281-483-9018 Typist: DA8/Karen.J. Chisholm 281-483-1091 281-483-5988 IN MEMORIAM Bob Legler April 4, 1927 - March 16, 2007 Bob Legler, the originator of this Space Shuttle Missions Summary Book, was born a natural Corn Husker and lived a full life. His true love was serving his country in the US Coast Guard, Merchant Marines, United Nations, US Army, and the NASA Space Programs as an aerospace engineer. As one of a handful of people to ever support the Mercury, Gemini, Apollo, Skylab, Space Shuttle, and International Space Station missions, Bob was an icon to his peers. He spent 44 years in this noble endeavor called manned space flight. In the memorial service for Bob, Milt Heflin provided the following insight: “Bob was about making things happen, no matter what his position or rank, in whatever the enterprise was at that time…it might have been dodging bullets and bombs while establishing communication systems for United Nations outposts in crazy places…it might have been while riding the Coastal Sentry Quebec Tracking ship in the Indian Ocean…watching over the Lunar Module electrical power system or the operation of the Apollo Telescope Mount…serving as a SPAN Manager in the MCC (where a lot of really good stories were told during crew sleep)…or even while serving as the Chairman of the Annual FOD Chili Cook-off or his beloved Chairmanship of the Apollo Flight -

Finding Aid to the Historymakers ® Video Oral History with Dr. Robert Satcher, Jr
Finding Aid to The HistoryMakers ® Video Oral History with Dr. Robert Satcher, Jr. Overview of the Collection Repository: The HistoryMakers®1900 S. Michigan Avenue Chicago, Illinois 60616 [email protected] www.thehistorymakers.com Creator: Satcher, Robert Lee, Jr., 1965- Title: The HistoryMakers® Video Oral History Interview with Dr. Robert Satcher, Jr., Dates: March 3, 2014 and May 7, 2014 Bulk Dates: 2014 Physical 8 uncompressed MOV digital video files (3:52:16). Description: Abstract: Orthopedic surgeon, chemical engineer, and astronaut Dr. Robert Satcher, Jr. (1965 - ) was a surgical oncologist and assistant professor at the University of Texas MD Anderson Cancer Center. He became the first orthopedic surgeon in space during NASA’s STS-129 mission. Satcher was interviewed by The HistoryMakers® on March 3, 2014 and May 7, 2014, in Houston, Texas. This collection is comprised of the original video footage of the interview. Identification: A2014_047 Language: The interview and records are in English. Biographical Note by The HistoryMakers® Orthopaedic surgeon, chemical engineer and astronaut Robert Lee Satcher, Jr. was born on September 22, 1965 in Hampton, Virginia to Robert and Marian Satcher. Satcher graduated from Denmark-Olar High School in Denmark, South Carolina, in 1982. He received his B.S. degree in chemical engineering from Massachusetts Institute of Technology (MIT) in 1986; his Ph.D. degree in chemical engineering from MIT in 1993; and his M.D. degree from Harvard Medical School in 1994. Satcher completed his postdoctoral research fellowships at MIT in 1994 and Satcher completed his postdoctoral research fellowships at MIT in 1994 and University of California, Berkeley in 1998; internship and residency in orthopaedic surgery at the University of California, San Francisco in 2000; and a fellowship in musculoskeletal oncology at the University of Florida in 2001. -
Facts a SA N
National Aeronautics and Space Administration Remaining Space Shuttle Missions elow are the approved target dates for the launches Mission: Deliver the Multi-Purpose Logistics Module Bremaining in the Space Shuttle Program. and the Lightweight Multi-Purpose Experiment Support Structure. STS-127 Launch Target: July 11, 2009 Info: STS-128 is the 30th shuttle mission to the at 7:39 p.m. EDT International Space Station. Shuttle: Endeavour Duration: 16 days STS-129 Crew: Launch Target: Nov. 12, 2009 facts Commander Mark Polansky at 4:22 p.m. EST Pilot Doug Hurley Shuttle: Atlantis Mission Specialists Christopher Cassidy, Tom Marshburn, Duration: 11 days ASAN Dave Wolf, Julie Payette/Canadian Space Agency, and Tim Kopra Crew: Mission: Deliver and install the Kibo-Japanese Experiment Commander Charles Hobaugh Module Exposed Facility, or JEM-EF; the Kibo-Japanese Pilot Barry Wilmore Experiment Logistics Module-Exposed Section, or ELM- Mission Specialists Robert Satcher, Michael Foreman, ES; and the Integrated Cargo Carrier. Randy Bresnik and Leland Melvin Deliver EXPRESS Logistics Carriers 1 and 2 Info: The JEM-EF facility will provide a type of “porch” for Mission: experiments in the exposed environment, and a robotic arm that will be attached to the Kibo Pressurized Module to Info: The carriers hold two spare gyroscopes, two nitrogen position experiments outside the station. Endeavour’s crew tank assemblies, two pump modules, an ammonia tank will make five spacewalks and deliver six new batteries for assembly, a spare latching end effector for the station’s the P6 truss, a spare drive unit for the Mobile Transporter robotic arm, a spare trailing umbilical system for the and a spare boom assembly for the Ku-band antenna. -
2009 Newsletters
In This Issue: MIT CLUB OF SOUTH TEXAS 2009 LEAP. Page I lWEY 2009 Membership Pagc I Sponsoring Activities for MIT South Texas Alumnae and Alumni Mentoring Program Page 2 ffluht Asslstrng MIT in Recruiting Students and Promoting its Reputation - Science Fair Judging Page 2 Promoting Engineering, Science, and Math Education in Our Local Area South InterClub Happy Hour Page 2 Texas February 2009 MIT Diversity Convocation Page 2 www.mithouston.org Do You Know A Science or Math Teacher That Would Like to Attend a One Week Summer Session at MIT? 2009 Leadership in Education (LEAP) department heads and distriot coordinators are also welcome Competition for Teachers to apply. Each application should be accompanied by (l) a completed application form for the MIT Application Deadline is March 1, 2009 slrmmer program (available in the brochure) and (2) a letter of recommendation from someone who The MIT Club of South Texas through its Leadership in can speak to the selection criteria noted above. Education Award Program (LEAP) has an ongoing interest in encouraging students interested. in science and mathematics In order to be considered for a scholarship and travel expenses and in helping to elevate the level of technical literacy in our for the MIT summer program, *applications should be sent to community. We would like to recognize key science and math Ed Rinehart, 13722 Ashley Run, Houston TX 71017 -15 I 1, to teachers who are making a ditference and to support their , be received by March 1. 2009. lf you have any questions or ongoing commitment to educating our youth in science and comments, call 28 I -61 9 -l 608. -
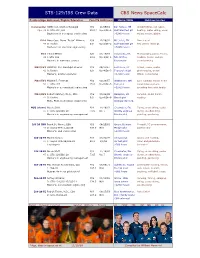
CBS News Spacecalc STS-129/ISS Crew Data
STS-129/ISS Crew Data CBS News SpaceCalc Position/Age Astronaut/Flights/Education Fam/TS DOB/Seat Home/BKG Hobbies/notes Commander USMC Col. Charles Hobaugh M/4 11/05/61 Bar Harbor, ME Weight lifting, volleyball, Age: 48 2: STS-104,118 25.5 * Up-1/Dn-1 Gulf War/test plt boating, water skiing, snow Bachelor's in aerospace engineering >5,000 hours skiing, soccor, biking Pilot Navy Capt. Barry "Butch" Wilmore M/0 12/29/62 Mt. Juliet, TN None listed 46 0: Rookie 0.0 Up-2/Dn-2 Gulf War/test plt 663 carrier landings Bachelor's in electrical engineering >5,900 hours MS1 Leland Melvin S/0 02/15/64 Lynchburg, VA Photography, piano, tennis, 45 1:STS-122 12.8 Up-3/Dn-4 NFL draftee reading, music, cycling, Master's in materials science Researcher snow boarding MS2/EV3 USMC Lt. Col. Randolph Bresnik M/1 09/11/67 Fort Knox, KY Travel, music, scuba, 42 0: Rookie 0.0 Up-4/Dn-3 Topgun/test plt photography, weight Master's, aviation systems >4,500 hours lifting, motorcycles MS3/EV1 Michael J. Foreman M/3 03/29/57 Wadsworth, OH Golf, running, skiing, home 52 1: STS-123 15.8 Up-5/Dn-5 Test pilot repair/improvement, Master's in aeronautical engineering >5,000 hours spending time with family MS4/EV2 Robert Satcher, Ph.D., M.D. M/2 09/22/65 Hampton, VA Running, scuba diving, 44 0: Rookie 0.0 Up-6/Dn-6 Oncologist reading M.D., Ph.D.