Management of Facial Hyperpigmentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

Melasma on the Nape of the Neck in a Man
Letters to the Editor 181 Melasma on the Nape of the Neck in a Man Ann A. Lonsdale-Eccles and J. A. A. Langtry Sunderland Royal Hospital, Kayll Road, Sunderland SR4 7TP, UK. E-mail: [email protected] Accepted July 19, 2004. Sir, sunlight and photosensitizing agents may be more We report a 47-year-old man with light brown macular relevant. pigmentation on the nape of his neck (Fig. 1). It was The differential diagnosis for pigmentation at this site asymptomatic and had developed gradually over 2 years. includes Riehl’s melanosis, Berloque dermatitis and He worked outdoors as a pipe fitter on an oilrig module; poikiloderma of Civatte. Riehl’s melanosis typically however, he denied exposure at this site because he involves the face with a brownish-grey pigmentation; always wore a shirt with a collar that covered the biopsy might be expected to show interface change and affected area. However, on further questioning it liquefaction basal cell degeneration with a moderate transpired that he spent most of the day with his head lymphohistiocytic infiltrate, melanophages and pigmen- bent forward. This reproducibly exposed the area of tary incontinence in the upper dermis. It is usually pigmentation with a sharp cut off inferiorly at the level associated with cosmetic use and may be considered of his collar. He used various shampoos, aftershaves and synonymous with pigmented allergic contact dermatitis shower gels, but none was applied directly to that area. of the face (6, 7). Berloque dermatitis is considered to be His skin was otherwise normal and there was no family caused by a photoirritant reaction to bergapentin; it history of abnormal pigmentation. -

An Unusual Presentation of a Unilateral Asymptomatic Riehl's
ts & C por a e se R S l Michael, Med Rep Case Stud 2018, 3:1 t a u c d i i DOI: 10.4172/2572-5130.1000152 d e s e M + Medical Reports and Case Studies ISSN: 2572-5130 Case Report Open Access An Unusual Presentation of a Unilateral Asymptomatic Riehl’s Melanosis in a 45 Year Old Male Chan Kam Tim Michael* Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong *Corresponding author: Chan Kam Tim Michael, Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong, Tel: +85221282129; E-mail: [email protected] Received Date: Feb 12, 2018; Accepted Date: Mar 12, 2018; Published Date: Mar 21, 2018 Copyright: © 2018 Michael CKT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction but of post-inflammatory hyperpigmentation, Acquired unilateral Nevus (Hori’s Nevus), Riehl’s melanosis, Drug-induced Pigmented contact dermatitis (PCD), also known as Riehl’s hyperpigmentation, Lichenoid dermatitis; as well as Melasma and melanosis, is a rare facial hyperpigmentation usually secondary to Ochronosis. cosmetics. There are few documented reports in the literature, and many cases without proven diagnosis may have been treated with pigment lasers, especially in beauty parlour settings. We report a case referred from a private practitioner who has a special interest in dermatology. The patient was diagnosed subsequently as having Riehl’s melanosis and treated with non-tyrosinase inhibitor bleaching agents, sun avoidance and mandatory abstinence from over-the-counter cosmetic products. -
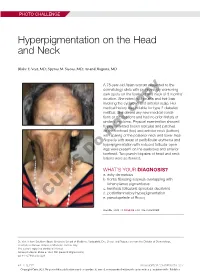
Hyperpigmentation on the Head and Neck
PHOTO CHALLENGE Hyperpigmentation on the Head and Neck Blake E. Vest, MD; Spyros M. Siscos, MD; Anand Rajpara, MD A 78-year-old Asian woman presented to the dermatology clinic with progressively worsening dark spots on the forehead and neck of 3 months’ duration. She noted mild pruritis and hair loss involving the eyebrows and anterior scalp. Her medical history was notable for type 2 diabetes mellitus. She deniedcopy any new medical condi- tions or medications and had no prior history of similar symptoms. Physical examination showed hyperpigmented brown macules and patches on the forehead (top) and anterior neck (bottom) withnot sparing of the posterior neck and lower face. Alopecia with areas of perifollicular erythema and hyperpigmentation with reduced follicular open- ings were present on the eyebrows and anterior Doforehead. Two punch biopsies of head and neck lesions were performed. WHAT’S YOUR DIAGNOSIS? a. ashy dermatosis b. frontal fibrosing alopecia overlapping with lichen planus pigmentosus c. keratosis follicularis spinulosa decalvans d. postinflammatory hyperpigmentation CUTIS e. pseudopelade of Brocq PLEASE TURN TO PAGE E3 FOR THE DIAGNOSIS Dr. Vest is from Southern Illinois University School of Medicine, Springfield. Drs. Siscos and Rajpara are from the Division of Dermatology, University of Kansas School of Medicine, Kansas City. The authors report no conflict of interest. Correspondence: Blake E. Vest, MD ([email protected]). doi:10.12788/cutis.0226 E2 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2021. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Frontal Fibrosing Alopecia Overlapping With Lichen Planus Pigmentosus icroscopic examination revealed focal dermal of the skin have been reported, including the entire pigmentation, papillary fibrosis, and epidermal scalp, eyebrows, and eyelashes. -

Phytophotodermatitis
PHYTOPHOTODERMATITIS http://www.aocd.org Phytophotodermatitis (PPD) is a cutaneous phototoxic reaction that occurs following contact with certain plants. The reaction is stimulated by skin exposure to light sensitizing botanical substances known as furanocoumarins followed by exposure to long wave ultraviolet light in sunlight. Furanocoumarins are present in plants such as, lemons, limes, mangos, parsley and many weeds. Psoralen is the active particle in furanocoumarins. Upon UVA radiation exposure from sunlight, psoralens within the skin react with molecular oxygen and form reactive oxygen species that induce destruction of skin cells and cause an inflammatory reaction. PPD is most common in the spring and summer, as psoralen concentrations are the highest and outdoor activities under the sun are increased. Exposure to plants or solutions such as lemon or lime juice, lead to bizarre patterns of distribution. Streaks may be present from brushing against a plant or haphazard lines from juice. Common presentations are on the upper lip from drinking citrus beverages, from spilled beverages, or even from wiping juice onto exposed skin to dry the hands. This is often referred to as “Margarita Rash”. The rash begins within 24 hours and can peak at 72 hours. The distribution of skin reactions is sharply limited to areas exposed to sun. Skin findings can consist of non-pruritic reactions, mild redness with or without erosions, to severe blistering. Redness can persist for weeks to months. Hyperpigmentation appears 1-2 weeks later and can last up to months. The distribution to sun exposed areas and pattern aid in diagnosis. History and a high index of suspicion is key to diagnosing PPD. -

Actinic Cheilitis
ACTINIC CHEILITIS http://www.aocd.org Actinic cheilitis, also known as solar cheilosis, farmer’s lip, or sailor’s lip, is a reaction to long-term sun exposure on the lips, primarily the lower lip. The lip is especially susceptible to UV radiation because it has a thinner epithelium and less pigment. Some believe actinic cheilitis represents a type of actinic keratosis and is therefore premalignant. Others believe it is a form of in-situ squamous cell carcinoma. Regardless, the literature is in agreement that its presence indicates an increased risk for invasive squamous cell carcinoma. Risk factors for actinic cheilitis include fair complexion, everted lips, male sex, advanced age, living at high altitudes, living close to the equator, outdoor working, history of non-melanoma skin cancer, and any condition that increases photosensitivity. Clinically, patients commonly have other signs of sun damage such as poikiloderma of Civatte, solar lentigines, actinic keratoses, Favre-Racouchot Syndrome, cutis rhomboidalis nuchae, and solar elastosis. Patients often complain of persistent chapped lips or lip tightness. Early changes include atrophy and blurring of the vermilion border. The lips become scaly and rough; erosions or fissures may occasionally present. When palpated, it can have a sandpaper-like texture. Differential diagnosis can include chronic lip licking, granulomatous cheilitis, drug-induced cheilitis, contact dermatitis, cheilitis glandularis, lupus erythematosus, and lichen planus. An appropriate history can help elicit the proper diagnosis, such as inquiring about new medications or lip balms, lip-licking habits, and cumulative sun exposure. When actinic cheilitis is suspected, one must determine whether a biopsy is appropriate. -

Treatment of Poikiloderma of Civatte with Ablative Fractional Laser Resurfacing: Prospective Study and Review of the Literature Emily P
JUNE 2009 527 Vo l u m e 8 • Is s u e 6 CO P YR IGHT © 2009 ORIGINAL ARTICLES JOURN A L OF DRUGS IN DER MA TOLOGY Treatment of Poikiloderma of Civatte With Ablative Fractional Laser Resurfacing: Prospective Study and Review of the Literature emily P. Tierney MD and C. William Hanke MD MPH Laser and Skin Surgery Center of Indiana, Carmel, IN ABSTRACT Background: Previous laser treatments for Poikiloderma of Civatte (PC) (i.e., Pulsed dye, Intense Pulsed Light, KTP and Argon) are limited by side effect profiles and/or efficacy. Given the high degree of safety and efficacy of ablative fractional photothermolysis (AFP) for photoaging, we set out to assess the efficacy of PC with AFP. Design: A prospective pilot study for PC in 10 subjects with a series of 1−3 treatment sessions. Treatment sessions were adminis- tered at 6−8 week intervals with blinded physician photographic analysis of improvement at 2 months post-treatment. Evaluation was performed of five clinical indicators, erythema/telangiecatasia, dyschromia, skin texture, skin laxity and cosmetic outcome. Results: The number of treatments required for improvement of PC ranged from 1 to 3, with an average of 1.4. For erythema/te- langiecatasia, the mean score improved 65.0% (95% CI: 60.7%, 69.3%) dyschromia, 66.7% (95% CI: 61.8%, 71.6%), skin texture, 51.7% (95% CI: 48.3%, 55.1%) and skin laxity, 52.5% (95% CI: 49.6%, 55.4%). For cosmetic outcome, the mean score improved 66.7% (95% CI: 62.6%, 70.8%) at 2 months post treatment. -

UCSF Fresno, Medical Educakon Program J Heppner MD, H Lee MD
(—THIS SIDEBAR DOES NOT PRINT—) QUICK START (cont.) DESIGN GUIDE Phytophotoderma/s Resul/ng From Citrus Exposure: A Pediatric Case Series from Central California How to change the template color theme This PowerPoint 2007 template produces a 36”x48” You can easily change the color theme of your poster by going to the presentation poster. You can use it to create your research DESIGN menu, click on COLORS, and choose the color theme of your poster and save valuable time placing titles, subtitles, text, J Heppner MD, H Lee MD, P Armenian MD choice. You can also create your own color theme. and graphics. UCSF Fresno, Medical Educaon Program We provide a series of online tutorials that will guide you through the poster design process and answer your poster production questions. To view our template tutorials, go online to PosterPresentations.com and click on HELP DESK. You can also manually change the color of your background by going to Introduc>on Case Series Descripon Case Series Descripon Discussion VIEW > SLIDE MASTER. After you finish working on the master be sure to When you are ready to print your poster, go online to Lisbon Lemon (Citrus limon) Key Lime (Citrus aurantifolia) go to VIEW > NORMAL to continue working on your poster. PosterPresentations.com Psoralens belong to the furocoumarin family, and cause This is a consecutive-patient case series of five girls Few phytophotodermatitis outbreaks demonstrate phytophotodermatitis when coupled with ultraviolet aged 7-11 transferred from an outside facility for such severity in multiple pediatric patients, How to add Text Need assistance? Call us at 1.510.649.3001 light exposure. -

Dermatological Indications of Disease - Part II This Patient on Dialysis Is Showing: A
“Cutaneous Manifestations of Disease” ACOI - Las Vegas FR Darrow, DO, MACOI Burrell College of Osteopathic Medicine This 56 year old man has a history of headaches, jaw claudication and recent onset of blindness in his left eye. Sed rate is 110. He has: A. Ergot poisoning. B. Cholesterol emboli. C. Temporal arteritis. D. Scleroderma. E. Mucormycosis. Varicella associated. GCA complex = Cranial arteritis; Aortic arch syndrome; Fever/wasting syndrome (FUO); Polymyalgia rheumatica. This patient missed his vaccine due at age: A. 45 B. 50 C. 55 D. 60 E. 65 He must see a (an): A. neurologist. B. opthalmologist. C. cardiologist. D. gastroenterologist. E. surgeon. Medscape This 60 y/o male patient would most likely have which of the following as a pathogen? A. Pseudomonas B. Group B streptococcus* C. Listeria D. Pneumococcus E. Staphylococcus epidermidis This skin condition, erysipelas, may rarely lead to septicemia, thrombophlebitis, septic arthritis, osteomyelitis, and endocarditis. Involves the lymphatics with scarring and chronic lymphedema. *more likely pyogenes/beta hemolytic Streptococcus This patient is susceptible to: A. psoriasis. B. rheumatic fever. C. vasculitis. D. Celiac disease E. membranoproliferative glomerulonephritis. Also susceptible to PSGN and scarlet fever and reactive arthritis. Culture if MRSA suspected. This patient has antithyroid antibodies. This is: • A. alopecia areata. • B. psoriasis. • C. tinea. • D. lichen planus. • E. syphilis. Search for Hashimoto’s or Addison’s or other B8, Q2, Q3, DRB1, DR3, DR4, DR8 diseases. This patient who works in the electronics industry presents with paresthesias, abdominal pain, fingernail changes, and the below findings. He may well have poisoning from : A. lead. B. -

Reticulate Dermatoses
[Downloaded free from http://www.e-ijd.org on Tuesday, April 08, 2014, IP: 111.93.251.154] || Click here to download free Android application for this journal CME Article Reticulate Dermatoses Keshavmurthy A Adya, Arun C Inamadar, Aparna Palit From the Department of Dermatology, Venereology and Leprosy, SBMP Medical College, Hospital and Research Center, BLDE University, Bijapur, Karnataka, India Abstract The term “reticulate” is used for clinical description of skin lesions that are configured in a net-like pattern. Many primary and secondary dermatoses present in such patterns involving specific body sites. Certain cutaneous manifestations of systemic diseases or genodermatoses also present in such manner. This review classifies and describes such conditions with reticulate lesions and briefly, their associated features. Key Words: Mottling, net-like, reticulate, retiform What was known? 3. Poikilodermatous Reticulate configuration of lesions is seen in many primary dermatoses and a. Inherited also as cutaneous reaction patterns consequent to internal pathology. • Rothmund–Thomson syndrome • Dyskeratosis congenita Reticulate Dermatoses • Xeroderma pigmentosum • Cockayne syndrome The term “reticulate” is commonly used for clinical • Fanconi anemia description of “net-like”, “sieve-like,” or “chicken wire” • Mendes da Costa syndrome configuration of the skin lesions. Various congenital • Kindler syndrome and acquired dermatoses present with this pattern of • Degos–Touraine syndrome skin lesions. Many systemic diseases also present with • Hereditary sclerosing poikiloderma of Weary such cutaneous manifestations providing useful clues to • Hereditary acrokeratotic poikiloderma of Weary diagnosis. • Werner’s syndrome (adult progeria) Classification • Chanarin–Dorfman syndrome • Diffuse and macular atrophic dermatosis 1. Vascular b. Acquired a. Cutis marmorata • Poikiloderma of Civatte b. -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1