Non-Selective Beta-Blockers Decrease Infection, Acute Kidney
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Analysis of Residential and Auto Break-In Records in Taipei City
Portland State University PDXScholar Engineering and Technology Management Student Projects Engineering and Technology Management Winter 2018 Analysis of Residential and Auto Break-in Records in Taipei City Afnan Althoupety Portland State University Aishwarya Joy Portland State University Juchun Cheng Portland State University Priyanka Patil Portland State University Tejas Deshpande Portland State University Follow this and additional works at: https://pdxscholar.library.pdx.edu/etm_studentprojects Part of the Applied Statistics Commons, and the Social Control, Law, Crime, and Deviance Commons Let us know how access to this document benefits ou.y Citation Details Althoupety, Afnan; Joy, Aishwarya; Cheng, Juchun; Patil, Priyanka; and Deshpande, Tejas, "Analysis of Residential and Auto Break-in Records in Taipei City" (2018). Engineering and Technology Management Student Projects. 1943. https://pdxscholar.library.pdx.edu/etm_studentprojects/1943 This Project is brought to you for free and open access. It has been accepted for inclusion in Engineering and Technology Management Student Projects by an authorized administrator of PDXScholar. Please contact us if we can make this document more accessible: [email protected]. Analysis of Residential and Auto Break-in Records in Taipei City Course: ETM 538 Term: Winter 2018 Instructors: Daniel Sagalowicz, Mike Freiling Date: 03/09/2018 Authors:Afnan Althoupety , Aishwarya Joy , Juchun Cheng , Priyanka Patil , Tejas Deshpande 1 1. Introduction Taipei City is the capital of Taiwan. It has population of 2.7 million living in the city area of 271 km2 (104 mi2). There are totally 12 administrative districts in this city. To maintain the safety of the city, Taipei City Police Bureau has arranged regular patrol routes with focus on the high-risk area where residential and auto break-in occurs. -

Healthy Cities in Taiwan
Healthy Cities in Taiwan Content 1. Development of healthy cities in Taiwan 2 2. Promotional models for healthy cities in Taiwan 3 3. Taiwan healthy city indicators 3 4. Taiwan healthy cities network 5 5. Taiwan Healthy City A wards 6 Appendix 13 I. Themes of Awards and Awardees for the First Taiwan Healthy City Award II. Themes of Awards and Awardees for the Second Taiwan Healthy City Award III. \Contact information and websites of healthy cities in Taiwan Commission: Bureau of Health Promotion, Department of Health, Taiwan Compile and Print: Healthy City Research Center, National Cheng Kung University October 2010 1. Development of healthy cities in Taiwan The healthy cities movement began in 1986. It was first promoted by the WHO Regional Office for Europe, and primarily targeted European cities. After almost two decades of work, the results have been very good, and European healthy cities are now exemplars for the world. As a result, WHO regional offices have started to advocate healthy cities for each of their regions. In Taiwan, the Republic of China decided to participate in the healthy cities movement in the beginning of the new Millennium. The Bureau of Health Promotion (BHP), Department of Health called for a pilot proposal in 2003, a cross-disciplinary team of scholars at National Cheng Kung University won the project, and found collaboration from Tainan City, thus, pioneered the healthy city development in Taiwan. BHP has since continued to fund other local authorities to promote healthy cities, including Miaoli County, Hualien County, Kaohsiung City and Taipei County. Since the results have been excellent, some other counties and cities have also allotted budgets to commission related departments for implementation. -
![[カテゴリー]Location Type [スポット名]English Location Name [住所](https://docslib.b-cdn.net/cover/8080/location-type-english-location-name-1138080.webp)
[カテゴリー]Location Type [スポット名]English Location Name [住所
※IS12TではSSID"ilove4G"はご利用いただけません [カテゴリー]Location_Type [スポット名]English_Location_Name [住所]Location_Address1 [市区町村]English_Location_City [州/省/県名]Location_State_Province_Name [SSID]SSID_Open_Auth Misc Hi-Life-Jingrong Kaohsiung Store No.107 Zhenxing Rd. Qianzhen Dist. Kaohsiung City 806 Taiwan (R.O.C.) Kaohsiung CHT Wi-Fi(HiNet) Misc Family Mart-Yongle Ligang Store No.4 & No.6 Yongle Rd. Ligang Township Pingtung County 905 Taiwan (R.O.C.) Pingtung CHT Wi-Fi(HiNet) Misc CHT Fonglin Service Center No.62 Sec. 2 Zhongzheng Rd. Fenglin Township Hualien County Hualien CHT Wi-Fi(HiNet) Misc FamilyMart -Haishan Tucheng Store No. 294 Sec. 1 Xuefu Rd. Tucheng City Taipei County 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.204 Sec. 2 Zhongshan Rd. Jiaoxi Township Yilan County 262 Taiwan (R.O.C.) Yilan CHT Wi-Fi(HiNet) Misc 7-Eleven No.231 Changle Rd. Luzhou Dist. New Taipei City 247 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Restaurant McDonald's 1F. No.68 Mincyuan W. Rd. Jhongshan District Taipei CHT Wi-Fi(HiNet) Restaurant Cobe coffee & beauty 1FNo.68 Sec. 1 Sanmin Rd.Banqiao City Taipei County Taipei CHT Wi-Fi(HiNet) Misc Hi-Life - Taoliang store 1F. No.649 Jhongsing Rd. Longtan Township Taoyuan County Taoyuan CHT Wi-Fi(HiNet) Misc CHT Public Phone Booth (Intersection of Sinyi R. and Hsinsheng South R.) No.173 Sec. 1 Xinsheng N. Rd. Dajan Dist. Taipei CHT Wi-Fi(HiNet) Misc Hi-Life-Chenhe New Taipei Store 1F. No.64 Yanhe Rd. Anhe Vil. Tucheng Dist. New Taipei City 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.7 Datong Rd. -

Deep Learning Application for Vocal Fold Disease Prediction Through Voice Recognition: Preliminary Development Study
JOURNAL OF MEDICAL INTERNET RESEARCH Hu et al Original Paper Deep Learning Application for Vocal Fold Disease Prediction Through Voice Recognition: Preliminary Development Study Hao-Chun Hu1,2,3, MD; Shyue-Yih Chang4, MD; Chuen-Heng Wang5, MSc; Kai-Jun Li2, MSc; Hsiao-Yun Cho2,6, MD; Yi-Ting Chen5, MSc; Chang-Jung Lu4, MSc; Tzu-Pei Tsai4, MSc; Oscar Kuang-Sheng Lee1,7,8,9, MD, PhD 1Institute of Clinical Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan 2Department of Otorhinolaryngology-Head and Neck Surgery, Fu Jen Catholic University Hospital, Fu Jen Catholic University, New Taipei City, Taiwan 3School of Medicine, College of Medicine, Fu Jen Catholic University, New Taipei City, Taiwan 4Voice Center, Department of Otolaryngology, Cheng Hsin General Hospital, Taipei, Taiwan 5Muen Biomedical and Optoelectronic Technologist Inc, Taipei, Taiwan 6Graduate Institute of Business Administration, Fu Jen Catholic University, New Taipei City, Taiwan 7Department of Orthopedics, China Medical University Hospital, Taichung, Taiwan 8Stem Cell Research Center, National Yang Ming Chiao Tung University, Taipei, Taiwan 9Department of Medical Research, Taipei Veterans General Hospital, Taipei, Taiwan Corresponding Author: Oscar Kuang-Sheng Lee, MD, PhD Institute of Clinical Medicine National Yang Ming Chiao Tung University No 155, Section 2, Li-Nong Street, Beitou District Taipei, 11221 Taiwan Phone: 886 2 28757391 Fax: 886 2 28757841 Email: [email protected] Abstract Background: Dysphonia influences the quality of life by interfering with communication. However, a laryngoscopic examination is expensive and not readily accessible in primary care units. Experienced laryngologists are required to achieve an accurate diagnosis. Objective: This study sought to detect various vocal fold diseases through pathological voice recognition using artificial intelligence. -
Directory of Head Office and Branches
Directory of Head Office and Branches 一 國內總分行營業單位一覽表 二 海外分支機構 I. Domestic Business Units II. Overseas Units Foreword I. Domestic Business Units No. 120 Sec 1‚ Chongcing South Road‚ Jhongjheng District‚ Taipei City 10007‚ Taiwan (R.O.C. ) P. O. Box 5 or 305‚ Taipei‚ Taiwan SWIFT: BKTWTWTP http://www. bot. com. tw TELEX: 11201 TAIWANBK Introduction CODE OFFICE ADDRESS TELEPHONE FAX No. 120 Sec. 1‚ Chongcing South Road‚ Jhongjheng District‚ 0037 Department of Business 02-23493399 02-23759708 Taipei City Governance Corporate Department of Public 0059 No. 120 Sec. 1‚ Gueiyang Street‚ Jhongjheng District‚ Taipei City 02-23615421 02-23751125 Treasury 0082 Department of Trusts No. 49 Sec. 1‚ Wuchang St.‚ Jhongjheng District‚ Taipei City 02-23618030 02-23821846 Report 0691 Offshore Banking Branch 1F.‚ No.162 Bo-ai Road‚ Jhongjheng District‚ Taipei City 02-23493456 02-23894500 Department of Securities 2F., No. 58 Sec. 1‚ Chongcing South Road‚ Jhongjheng District‚ 1698 02-23882188 02-23716159 (note) Taipei City Activities Fund-Raising 0071 Guancian Branch No. 49 Guancian Road‚ Jhongjheng District‚ Taipei City 02-23812949 02-23753800 0093 Tainan Branch No. 155 Sec. 1‚ Fucian Road‚ Central District‚ Tainan City 06-2160168 06-2160188 0107 Taichung Branch No. 140 Sec. 1‚ Zihyou Road‚ West District‚ Taichung City 04-22224001 04-22224274 0118 Kaohsiung Branch No. 264 Jhongjheng 4th Road‚ Cianjin District‚ Kaohsiung City 07-2515131 07-2211257 Conditions General 0129 Keelung Branch No. 16‚ Yee 1st Road‚ Jhongjheng District‚ Keelung City 02-24247113 02-24220436 Chunghsin New Village No. 11 Guanghua Road‚ Jhongsing Village‚ Nantou City‚ Operating 0130 049-2332101 049-2350457 Branch Nantou County 0141 Chiayi Branch No. -
Preoperative Estimate of Natural Ureteral Length Based on Computed
www.nature.com/scientificreports OPEN Preoperative estimate of natural ureteral length based on computed tomography and/or plain radiography Jen‑Ting Hsu1, Jen‑Shu Tseng1,6*, Marcelo Chen1,3,4, Fang‑Ju Sun1,4,6, Chien‑Wen Chen2, Wun‑Rong Lin1,3, Pai‑Kai Chiang1,3 & Allen W. Chiu1,5 To predict natural ureter lengths based on clinical images. We reviewed our image database of patients who underwent multiphasic computed tomography urography from January 2019 to April 2020. Natural ureteral length (ULCTU ) was measured using a three‑dimensional curved multiplanar reformation technique. Patient parameters including age, height, and height of the lumbar spine, the index of ureteral length using kidney/ureter/bladder (KUB) radiographs (C‑P and C‑PS) and computed tomography (ULCT) were collected. ULCTU correlated most strongly with ULCT. R square and adjusted R square values from multivariate regression were 0.686 and 0.678 (left side) and 0.516 and 0.503 (right side), respectively. ULCTU could be estimated by the regression model in three diferent scenarios as follows: ULCT + C-P × + × ULCTUL = 0.405 ULCTL 0.626 C-PL – 0.508 cm × + × ULCTUR = 0.558 ULCTR 0.218 C-PR + 6.533 cm × + ULCTULCTUL = 0.876 ULCTL 6.337 cm × + ULCTUR = 0.710 ULCTR 9.625 cm C-P × + ULCTUL = 0.678 C-PL 4.836 cm × + ULCTUR = 0.495 C-PR 10.353 cm We provide equations to predict ULCTU based on CT, KUB or CT plus KUB for diferent clinical scenarios. The formula based on CT plus KUB provided the most accurate estimation, while the others had lower validation values but could still meet clinical needs. -

Short‐Term and Long‐Term Impacts of Helicobacter Pylori Eradication With
bs_bs_banner doi:10.1111/jgh.14736 GASTROENTEROLOGY Short-term and long-term impacts of Helicobacter pylori eradication with reverse hybrid therapy on the gut microbiota Ping-I Hsu,* Chao-Yu Pan,† John Y Kao,‡ Feng-Woei Tsay,* Nan-Jing Peng,§ Sung-Shuo Kao,* Yan-Hua Chen,* Tzung-Jiun Tsai,* Deng-Chyang Wu¶ and Kuo-Wang Tsai**,†† *Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan†Institute of Biomedical InformaticsAcademia Sinica, National Yang-Ming University and Institute of Biomedical Sciences, Taipei, Taiwan‡Department of Internal Medicine, Division of Gastroenterology, Michigan Medicine, University of Michigan, Ann Arbor, Michigan USA§Department of Nuclear Medicine, Kaohsiung Veterans General Hospital and National Yang-Ming University, Kaohsiung, Taiwan¶Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan**Department of Medical Education and Research, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan††Institute of Biomedical Sciences, National Sun Yat-Sen University, Kaohsiung, Taiwan Key words Abstract dysbiosis, erm(B), Helicobacter pylori, microbiome, treatment. Background and Aims: Anti-Helicobacter pylori therapy may lead to the growth of path- ogenic or antibiotic-resistant bacteria in the gut. The study aimed to investigate the short- Accepted for publication 13 May 2019. term and long-term impacts of H. pylori eradication with reverse hybrid therapy on the components and macrolide resistance of the gut microbiota. Correspondence Methods: Helicobacter pylori-related gastritis patients were administered a 14-day reverse Dr Kuo-Wang Tsai, Department of Medical hybrid therapy. Fecal samples were collected before treatment and at the end of week 2, Education and Research, Kaohsiung Veterans week 8, and week 48. -

Documentation Checked: from 2020-08-05 to 2020-10-12
Technical Report Technical Report No.: 61.327.20.017.01 Date: 2020-10-12 HSIANG FU CHIA ENTERPRISE CO., LTD. NO. 41, Lane 737, Jiadian Rd., Homei Town 50860 Changhua County, Client: TAIWAN Contact person: Ms. Sandy Chen HSIANG FU CHIA ENTERPRISE CO., LTD. NO. 41, Lane 737, Jiadian Rd., Homei Town 50860 Changhua County, Manufacturing place: TAIWAN Contact person: Ms. Sandy Chen Product: Steps (Dome type) Test subject: Type: T5, T6, T7, T8 EK5/AK1 19-01:2019 EN 14183:2003 Test specification: AfPS GS 2019:01 PAK • Inspection according to specified requirements to realize the conformity with the Produktsicherheitsgesetz – ProdSG • Inspection according to the test specification Purpose of examination: The test result show that the presented product is in compliance with the specific requirements. Test result: Requirements of AfPS GS 2019:01 PAK have been evaluated and found to be met by evaluation and/or relevant test 7 Rev. Rev. - Any use for advertising purposes must be granted in writing. This technical report may only be quoted in full. This report is the result of a single examination of the object in question and is not generally applicable evaluation of the quality of other products in regular production. For further details please see testing and certification regulation, chapter A-3.4. TTW0902.02E - Report No.: 61.327.20.017.01 TEL: +886 2 2898 6818 TÜV SÜD Asia Ltd. Taiwan Branch ITC Rev.: 01 FAX: +886 2 2895 1598 7F, No.37, Section 2, Zhongyang S. Road, Date: 2020-10-12 www.tuvsud.com Beitou District, 11270, Taipei City, Taiwan Page 1 of 5 Doc No.: Doc No.: Technical Report 1. -

Taiwan Tourism Coupon Guide Book
Taiwan Tourism Coupon Guide Book Qinbi Village, Beigan Township, Matsu Travel Tips Travel Preface Travel Tips A land of beautiful scenery and warm human touch, Taiwan is blessed with the winds of freedom, a fertile land, and a sincere and kind-hearted people. Moreover, Taiwan ranks among the top 10 safest countries in the world. Pay attention to the following entry and visa information, and have a great trip to Taiwan! Entry Visa make purchases of at least NT$2,000 on the same day Taiwan, a Rarefrom the Verdant same designated stores Gem with the “Taiwan Tax There are four types of visas according to the Refund”-label is eligible to request the “Application purposes of entry and the identity of applicants: inside the Tropic of FormCancer for VAT Refund.” To claim the refund, they must 1. Visitor visa: a short-term visa with a duration of stay apply at the port of their departure from the R.O.C. of up to 180 days Taiwan, the beautiful island on the Pacificwithin Ocean, 90 daysis a rarefollowing verdant the dategem of among purchase, the and they 2. Resident visa: a long-term visa with a duration of countries that the Tropic of Cancer passes through.must take the purchased goods out of the country with stay of more thanTaiwan’s 180 days area accounts for only 0.03% of the world’s total area. However, Taiwan them. For further details, please visit the following 3. Diplomaticcontains visa substantial natural resources. Continuous tectonic movements have created websites: 4. Courtesy visacoastlines, basins, plains, rolling hills, valleys, and majestic peaks for the island and made it - http://www.taxrefund.net.tw Types of theabundantly duration endowof stay includewith mountains; 14-day, 30- over 200 of its peaks are more than 3,000 meters high, - http://admin.taiwan.net.tw day, 60-day, 90-day,making etc. -
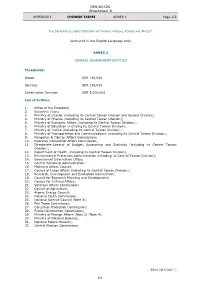
GPA/W/326 Attachment K K1
GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 1/2 THE SEPARATE CUSTOMS TERRITORY OF TAIWAN, PENGHU, KINMEN AND MATSU* (Authentic in the English Language only) ANNEX 1 CENTRAL GOVERNMENT ENTITIES Thresholds: Goods SDR 130,000 Services SDR 130,000 Construction Services SDR 5,000,000 List of Entities: 1. Office of the President; 2. Executive Yuan; 3. Ministry of Interior (including its Central Taiwan Division and Second Division); 4. Ministry of Finance (including its Central Taiwan Division); 5. Ministry of Economic Affairs (including its Central Taiwan Division); 6. Ministry of Education (including its Central Taiwan Division); 7. Ministry of Justice (including its Central Taiwan Division); 8. Ministry of Transportation and Communications (including its Central Taiwan Division); 9. Mongolian & Tibetan Affairs Commission; 10. Overseas Compatriot Affairs Commission; 11. Directorate-General of Budget, Accounting and Statistics (including its Central Taiwan Division); 12. Department of Health (including its Central Taiwan Division); 13. Environmental Protection Administration (including its Central Taiwan Division); 14. Government Information Office; 15. Central Personnel Administration; 16. Mainland Affairs Council; 17. Council of Labor Affairs (including its Central Taiwan Division); 18. Research, Development and Evaluation Commission; 19. Council for Economic Planning and Development; 20. Council for Cultural Affairs; 21. Veterans Affairs Commission; 22. Council of Agriculture; 23. Atomic Energy Council; 24. National Youth Commission; 25. National Science Council (Note 3); 26. Fair Trade Commission; 27. Consumer Protection Commission; 28. Public Construction Commission; 29. Ministry of Foreign Affairs (Note 2) (Note 4); 30. Ministry of National Defense; 31. National Palace Museum; 32. Central Election Commission. … 2014 (WT/Let/…) K1 GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 2/2 * In English only. -

Directory of Head Office and Branches
Directory of Head Office and Branches 106 I. Domestic Business Units 120 Sec 1, Chongcing South Road, Jhongjheng District, Taipei City 10007, Taiwan (R.O.C.) P.O. Box 5 or 305 SWIFT: BKTWTWTP http://www.bot.com.tw TELEX 11201 TAIWANBK CODE OFFICE ADDRESS TELEPHONE FAX 0037 Department of 120 Sec 1, Chongcing South Road, Jhongjheng District, 02-23493399 02-23759708 Business ( I ) Taipei City 0059 Department of 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23615421 02-23751125 Public Treasury Taipei City 0071 Department of 49 Guancian Road, Jhongjheng District, Taipei City 02-23812949 02-23753800 Business ( II ) 0082 Department of 58 Sec 1, Chongcing South Road, Jhongjheng District, 02-23618030 02-23821846 Trusts Taipei City 0691 Offshore Banking 1F, 3 Baocing Road, Jhongjheng District, Taipei City 02-23493456 02-23894500 Branch 1850 Department of 4F, 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23494567 02-23893999 Electronic Banking Taipei City 1698 Department of 2F, 58 Sec 1, Chongcing South Road, Jhongjheng 02-23882188 02-23716159 Securities District, Taipei City 0093 Tainan Branch 155 Sec 1, Fucian Road, Central District, Tainan City 06-2160168 06-2160188 0107 Taichung Branch 140 Sec 1, Zihyou Road, West District, Taichung City 04-22224001 04-22224274 0118 Kaohsiung Branch 264 Jhongjheng 4th Road, Cianjin District, 07-2515131 07-2211257 Kaohsiung City 0129 Keelung Branch 16, YiYi Road, Jhongjheng District, Keelung City 02-24247113 02-24220436 0130 Chunghsin New 11 Guanghua Road, Jhongsing Village, Nantou City, 049-2332101 -

Downloaded from the Website of Taiwan's National Health Insurance Administration (TNHIA) from the Third Quarter of 2010 to the Third Quarter of 2016
JMIR MEDICAL INFORMATICS Kan et al Original Paper Therapeutic Duplication in Taiwan Hospitals for Patients With High Blood Pressure, Sugar, and Lipids: Evaluation With a Mobile Health Mapping Tool Wei-Chih Kan1,2, MD; Shu-Chun Kuo3,4*, MD; Tsair-Wei Chien5*, MBA; Jui-Chung John Lin6, DC; Yu-Tsen Yeh7, BSc; Willy Chou8,9*, MD; Po-Hsin Chou10,11*, MD 1Department of Nephrology, Chi Mei Medical Center, Tainan, Taiwan 2Department of Biological Science and Technology, Chung Hwa University of Medical Technology, Tainan, Taiwan 3Department of Ophthalmology, Chi Mei Medical Center, Tainan, Taiwan 4Department of Optometry, Chung Hwa University of Medical Technology, Tainan, Taiwan 5Medical Research, Chi Mei Medical Center, Tainan, Taiwan 6USA Sports Medicine, Sherman Oaks, CA, United States 7Medical School, St George's, University of London, London, United Kingdom 8Department of Physical Medicine and Rehabilitation, Chiali Chi Mei Hospital, Tainan, Taiwan 9Department of Physical Medicine and Rehabilitation, Chung Shan Medical University, Taichung, Taiwan 10Department of Orthopedics and Traumatology, Taipei Veterans General Hospital, Taipei, Taiwan 11School of Medicine, National Yang-Ming University, Taipei, Taiwan *these authors contributed equally Corresponding Author: Po-Hsin Chou, MD Department of Orthopedics and Traumatology Taipei Veterans General Hospital 18F, 201, Section 2, Shipai Road, Beitou District Taipei, 112 Taiwan Phone: 886 228757557 Email: [email protected] Abstract Background: Cardiovascular disease causes approximately half of all deaths in patients with type 2 diabetes. Duplicative prescriptions of medication in patients with high blood pressure (hypertension), high blood sugar (hyperglycemia), and high blood lipids (hyperlipidemia) have attracted substantial attention regarding the abuse of health care resources and to implement preventive measures for such abuse.