Background Study-Rama Padma 7-2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5Bb5d0e237837-1321573-Sample
Notion Press Old No. 38, New No. 6 McNichols Road, Chetpet Chennai - 600 031 First Published by Notion Press 2018 Copyright © Shikha Bhatnagar 2018 All Rights Reserved. ISBN 978-1-64429-472-7 This book has been published with all efforts taken to make the material error-free after the consent of the author. However, the author and the publisher do not assume and hereby disclaim any liability to any party for any loss, damage, or disruption caused by errors or omissions, whether such errors or omissions result from negligence, accident, or any other cause. No part of this book may be used, reproduced in any manner whatsoever without written permission from the author, except in the case of brief quotations embodied in critical articles and reviews. Contents Foreword vii Ode to Hyderabad ix Chapter 1 Legend of the Founding of the City of Good Fortune, Hyderabad 1 Chapter 2 Legend of the Charminar and the Mecca Masjid 13 Chapter 3 Legend of the Golconda Fort 21 Chapter 4 Legend of Shri Ram Bagh Temple 30 Chapter 5 Legends of Ashurkhana and Moula Ali 52 Chapter 6 Legends of Bonalu and Bathukamma Festivals 62 Chapter 7 Legendary Palaces, Mansions and Monuments of Hyderabad 69 v Contents Chapter 8 Legend of the British Residency or Kothi Residency 81 Chapter 9 Legendary Women Poets of Hyderabad: Mah Laqa Bai Chanda 86 Chapter 10 The Legendary Sarojini Naidu and the Depiction of Hyderabad in Her Poems 92 Conclusion 101 Works Cited 103 vi Chapter 1 Legend of the Founding of the City of Good Fortune, Hyderabad The majestic city of Hyderabad is steeped in history and culture. -

Tender for Pickup and Door Delivery of Parcels and Couriers for Apsrtc Logistics for a Period of One Year and Extendable by Two More Years at the Following Cities
1 TENDER NOTIFICATION NO: Log-02/2018 CM (Comm), Tender ID- 238318 APSRTC TENDER FOR PICKUP AND DOOR DELIVERY OF PARCELS AND COURIERS FOR APSRTC LOGISTICS FOR A PERIOD OF ONE YEAR AND EXTENDABLE BY TWO MORE YEARS AT THE FOLLOWING CITIES. 1. VIJAYAWADA 2. VISAKHAPATNAM 3. HYDERABAD AND SECUNDERABAD Signature of the tenderer 2 DISCLAIMER The information contained in this Tender document or subsequently provided to tenderers, whether in document or verbal or any other form by or on behalf of Andhra Pradesh State Road Transport Corporation (APSRTC) by any of its employees or advisors, is provided to tenderers on the terms and conditions set out in this Tender document and such other terms and conditions subject to which such information is provided. The purpose of this Tender document is to provide interested parties with information that may be useful to them in eliciting their proposals pursuant to this Tender document. This Tender document may not be appropriate for all persons, and it is not possible for APSRTC, its employees or advisors to consider the investment objectives, financial situation and particular needs of each party who reads or uses this Tender document. This Tender document includes statements, which reflect various assumptions and assessments made by APSRTC in relation to the Contract. Such assumptions, assessments and statements do not purport to contain all the information that each tenderer may require. The assumptions, assessments, statements and information contained in this Tender document, may not be complete, accurate, adequate or correct. Each tenderer should, therefore, conduct his/its own investigations and analysis and should check the accuracy, adequacy, correctness, reliability and completeness of the assumptions, assessments, statements and information contained in this Tender document and obtain independent advice from appropriate sources. -

Slno Mandal Name of the School 1 Amberpet Ashafia High School , Old Malakpet 2 Amberpet Divyanjali High School , Bagh Amberpet, C.E
LIST OF PRIVATE UNAIDED HIGH SCHOOLS SLNO MANDAL NAME OF THE SCHOOL 1 AMBERPET ASHAFIA HIGH SCHOOL , OLD MALAKPET 2 AMBERPET DIVYANJALI HIGH SCHOOL , BAGH AMBERPET, C.E. COLONY 3 AMBERPET GANDHI HIGH SCHOOL , PATEL NAGAR 4 AMBERPET GEETA CONVENT HIGH SCHOOL , BAGH AMBERPET 5 AMBERPET GEETANJALI HIGH SCHOOL, ADIKMET , O.U. ROAD, ADIKMET 6 AMBERPET KISHORE KUNJ HIGH SCHOOL , AMBERPET LITTLE ANGELS HIGH SCHOOL , 16-9-758, RACE COURCE ROAD, OLD 7 AMBERPET MALAKPET 8 AMBERPET LITTLE BUDS GRAMMER HIGH SCHOOL , NEW NALLA KUNTA AMBERPET LITTLE SCHOLAR HIGH SCHOOL, OLD MALAKPET , OLD MALAKPET, 9 AMBERPET WATER TANK ROAD 10 AMBERPET NAVYA GRAMMAR HIGH SCHOOL , BUROJU LANE,AMBERPET 11 AMBERPET NEW CHAITANYA HIGH SCHOOL , PREM NAGAR, AMBERPET 12 AMBERPET OSMANIA MODEL HIGH SCHOOL , AMBERPET 13 AMBERPET PRAGATHI VIDYA NIKETAN HIGH SCHOOL , AMBERPET 14 AMBERPET ROSE BUDS HIGH SCHOOL , AMBERPET 15 AMBERPET SANA HIGH SCHOOL , BAPU NAGAR, AMBERPET 16 AMBERPET SARASWATHI PATASHALA HIGH SCHOOL, NALLAKUNTA , NALLAKUNTA 17 AMBERPET SARASWATHI V.N. HIGH SCHOOL , PATEL NAGAR 18 AMBERPET SRI AUROBINDO INTEGRAL HIGH SCHOOL , O.U. ROAD 19 AMBERPET SRI SAI GRAMMAR HIGH SCHOOL , 16-9-570/A,OLD MALAKPET 20 AMBERPET SRI SAI NAVANIKETHAN HIGH SCHOOL , 2-2-92/B/20,AMBERPET 21 AMBERPET SRI SHANTINIKETAN HIGH SCHOOL , 2-3-70/65, AMBERPET, HYD 22 AMBERPET ST. MARYS HIGH SCHOOL , NEW NALLAKUNTA 23 AMBERPET ST. PAUL MODEL HIGH SCHOOL , TULSI NAGAR 24 AMBERPET SWAMY DAYANANDA HIGH SCHOOL , AMBERPET 25 AMEERPET ANUPAMA HIGH SCHOOL , Madhura Nagar 26 AMEERPET BHARATH RATNA HIGH SCHOOL , AMEERPET 27 AMEERPET BLUE DIAMOND HIGH SCHOOL , S..R.Nagar 28 AMEERPET BRILLIAN GRAMMAR HIGH SCHOLL. -
Feb 2 5 1987
An Urban Design Study in The Walled City of Hyderabad by Arjun Kamal Mangaldas SUBMITTED TO THE DEPARTMENT OF ARCHITECTURE IN PARTIAL FULFILLMENT OF THE REQUIREMENTS OF THE DEGREE MASTER OF ARCHITECTURE AT THE MASSACHUSETTS INSTITUTE OF TECHNOLOGY FEBRUARY 1987 Arjun Kamal Mangaldas 1987 The author hereby grants to M.I.T. permission to reproduce and to distribute publicly copies of this thesis document in whole or in part. Signature of the author Arjun Kamal Mangaldas Department of Architecture December 18, 1986 I N Certified by William Yym n Porter Professor of Architecture and lanning Thesis Supervisor 'A .10 Accepted by -N udy D ytd Miftchell Chairman Departmen al Committee on Graduate Students MaSSCoETSmmSittee MA SSACHUSET TS INSITUTE OF TECHNOLOGY FEB 2 5 1987 UBRARIE5 Room 14-0551 77 Massachusetts Avenue Cambridge, MA 02139 Ph: 617.253.2800 MITLibraries Email: [email protected] Document Services http://Iibraries.mit.edu/docs DISCLAIMER NOTICE The accompanying media item for this thesis is available in the MIT Libraries or Institute Archives. Thank you. An Urban Design Study in the Walled City of Hyderabad by Arjun Kamal Mangaldas Submitted to the Department of Architecture on December 18, 1986 in partial fulfillment of the requirements for the Degree of Master of Architecture ABSTRACT The purpose of this study is to approach the Islamic city in India from a viewpoint which recognizes that the distinctions between cultural sections in a city are not only social and spatial but also physical, being manifest in the built environment. In this sense Hyderabad can be seen as a cross-cultural laboratory for investigating how two or more cultures (Muslim, Hindu, and a distinctly Western/colonial) operated in the same geographical environment but at different levels of social, economic, and physical development under conditions of monarchic rule. -

Ready to Take Pok: Army Chief Naravane KTR Douses 'Rebel' Fire
Follow us on: @TheDailyPioneer facebook.com/dailypioneer Established 1864 RNI No. TELENG/2018/76469 Published From *Late City Vol. 2 Issue 93 NATION 5 MONEY 6 SPECIAL 7 HYDERABAD DELHI LUCKNOW *Air Surcharge Extra if Applicable BHOPAL RAIPUR CHANDIGARH OPPN'S FALSEHOOD ON LAMBORGHINI SALES LITTLE ONES BHUBANESWAR THE LEADER CAA CREATES ANARCHY HIGHEST IN SOUTH INDIA 70MM RANCHI DEHRADUN WHO RAISED VIJAYAWADA VOICE FOR ` TELANGANA HYDERABAD, SUNDAY JANUARY 12, 2020; PAGES 12 3 AT 14 12 www.dailypioneer.com IAF OFFICER ARRESTED FOR TEJAS LANDS ON INS VIKRAMADITYA, SULTAN OF OMAN, 79, WHO RULED GADKARI: 1.5L PEOPLE DIE IN 5 LAKH POSING AS AMIT SHAH ON PHONE ACHIEVES A UNIQUE MILESTONE COUNTRY SINCE 1970, DIES ACCIDENTS EVERY YEAR IN INDIA adhya Pradesh Special Task Force (STF) has arrested a senior ndia moved a step closer to getting an indigenous fighter jet for its man's ailing Sultan Qaboos bin Said, one of the very year, around 1.5 lakh people are killed in five lakh accidents that MIndian Air Force officer for allegedly posing as Union Home Minister Inavy with the developmental Light Combat Aircraft Naval (LCA-N) OMiddle East's longest serving rulers who maintained Etake place across the country, Union Minister Nitin Gadkari said, and Amit Shah in a phone call to state Governor Lalji Tandon to facilitate his Tejas MK1 on Saturday (January 11, 2020) successfully making an the country's neutrality in regional struggles, died on expressed remorse that his ministry could not reduce these numbers friend's appointment as the vice-chancellor of a medical university, an arrested landing on Indian Navy aircraft carrier INS Vikramaditya. -

Landmarks of the Deccan
Digitized by the Internet Archive in 2019 with funding from Public.Resource.Org https://archive.org/details/landmarksofdeccaOOsyed LANDMARKS OF THE DECCAN LANDMARKS OF THE DECCAN A COMPREHENSIVE GUIDE TO THE ARCHAEOLOGICAL REMAINS OF THE CITY AND SUBURBS OF HYDERABAD SYED ALI ASGAR BILGRAMI, ASAFJAHI ASIAN EDUCATIONAL SERVICES NEW DELHI ★ MADRAS ★ 1992 ASIAN EDUCATIONAL SERVICES. * C-2/15, S.D.A. NEW DELHI-110016 * 5 SRIPCIRAM FIRST STREET, MADRAS-600014. First Published: 1927 AES Reprint New Delhi, 1992 ISBN: 81-206-0543-8 Published by J. Jetley for ASIAN EDUCATIONAL SERVICES C-2/15, SDA New Delhi-110016 Processed by APEX PUBLICATION SERVICES New Delhi-110016 Printed at Hi-tech Offset Printers Oelhi-i 10053 landmarks of tfje ©ecratr A Comprehensive Guide to the Archaeological Remains of the City and Suburbs of Hyderabad BY SYED ALI AS GAR BILGRAMI, ASAFJAHI Ag. Director of Archceology (1922-1924) Asst. Secretary to H.E.H. the Nizam’s Government, Judicial, Police & General Departments HYDERABAD-DECCAN: PRINTED AT THE GOVERNMENT CENTRAL PRESS 1927 I ■ . CONTENTS 1. DEDICATION. 2. INTRODUCTION. 3. PREFACE. 4. LIST OF MONUMENTS. 5. LIST OF ILLUSTRATIONS. 6. LIST OF AUTHORITIES. 7. CHRONOLOGY OF QUTBSHAHI DYNASTY. 8. DESCRIPTION OF MONUMENTS. 9. RETROSPECT. 10. INDEX. DEDICATION TO Lieutenant-General His Exalted Highness, Asaf Jah, Muzaffar-ul Mulk-Val-Mumalik, Nizamud-Dowlah, Nizam-ul-Mulk, NAWAB MIR SIR OSMAN ALI KHAN BAHADUR Fateh Jung, Faithful Ally of the British Government, Sipah Salar, Sultan-ul Uloom, G.C.S.I., G.C.B.E., Nizam of Hyderabad. This Book Is by Gracious Permission Dedicated by HIS EXALTED HIGHNESS’ Most Devoted Servant and Faithful Subject, SYED ALI ASGAR BILGRAMI. -

Absorption of Heavy Metals from Leafy Vegetables Grown Using Musi Water
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 11, Issue 10 Ver. I (October. 2017), PP 30-31 www.iosrjournals.org Absorption of heavy metals from leafy vegetables grown using Musi Water K. Nagajyothi, D.Ugandhar, N. Swathi & B. Hima Bindu Aurora’s Technological and Research Institute, Uppal, Hyderabad Abstract: Musiriver water is contaminated with various pollutants including toxic heavy metals which cause various health hazards. The green leafy vegetables cultivated using Musi water are found to contain the toxic heavy metals. When the heavy metals in Musi water used for cultivation,are absorbed by zeolites, the amount of heavy metals in leafy vegetables are very much reduced. Key words:Heavy metals, Musi, Clinoptilolite, Sorption, Sodium lauryl sulphate ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission: 26-09-2017 Date of acceptance: 06-10-2017 ----------------------------------------------------------------------------------------------------------------------------- ---------- I. Introduction Despite several attempts by various governments, the river Musi, which cuts across Hyderabad, continues to be one of the most polluted rivers in the country(1). A recent study discovered high levels of heavy metals like cadmium, chromium, nickel, lead, arsenic in the vegetables cultivated using Musi river water. These toxic heavy metals cause kidney, cardiovascular, nervous and bone diseases including cancer and ulcer. Heavy metals are persistent, bio accumulative and able to disrupt the metabolic functions and vital organs in humans and animals. Cadmium is a human carcinogen with an impact on respiratory system and liver. Chromium causes gastro intestinal, renal and neurological damage. Nickel’s serious health effects may include chronic bronchitis and lung cancer. -

Courtesans of Hyderabad
UC Irvine UC Irvine Previously Published Works Title Political players: Courtesans of Hyderabad Permalink https://escholarship.org/uc/item/2148b30c Journal The Indian Economic & Social History Review, 50(4) ISSN 0019-4646 Author Leonard, Karen Publication Date 2013-10-01 DOI 10.1177/0019464613502414 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Political players: Courtesans of Hyderabad Karen Leonard School of Social Sciences, UC Irvine Important recent works on the Mughal state and women in the Indo-Muslim world have not considered courtesans or tawa’ifs, the singing and dancing women employed by Indo-Muslim VWDWHVDQGQREOHVWREHVLJQL¿FDQWSDUWLFLSDQWVLQSROLWLFVDQGVRFLHW\'UDZLQJRQGHWDLOHG archival data from late nineteenth century Hyderabad state and other historical materials, I argue that courtesans were often elite women, cultural standard-setters and wielders of politi- FDOSRZHU:RPHQZKRVHDUWDQGOHDUQLQJJDLQHGWKHPSURSHUWLHVDQGDOOLDQFHVZLWKSRZHUIXO PHQWKH\ZHUHSROLWLFDOSOD\HUVLQSUHFRORQLDO,QGLDDQGLQWKHSULQFHO\VWDWHV7KH\VXFFHVVIXOO\ negotiated administrative reforms in princely states like Hyderabad, continuing to secure pro- WHFWLRQDQGSDWURQDJHZKLOHLQ%ULWLVK,QGLDWKH\EHJDQWREHFODVVL¿HGDVSURVWLWXWHV&RORQLDO and modern India have been less than kind to courtesans and their artistic traditions, and more UHVHDUFKQHHGVWREHGRQHRQWKHKLVWRU\RIFRXUWHVDQVDQGWKHLUFRPPXQLWLHV Keywords: Courtesans, Hyderabad, tawa’ifs, precolonial, Mughal India, -

Founder Members
LIST OF IRRO MEMBERS 2018-2019 AUTHORS 1. Dr. Madhu Pant 9. Shri H.L. Luthra 104 Pocket A C-13, Block C Mount Kailash Sector-6 East of Kailash HSR Layout New Delhi-110065. BANGALORE-560034. 2. Dr. D.P. Kothari 10. Dr. N.N. Kher Vice Chancellor B-103 VIT University Sector-55 Vellore-632014 NOIDA-201301. TAMIL NADU. 11. Shri Subit Kumar Saha 3. Dr. A. Padmanabhan Chemistry Group 14, 19th Cross Road BITS, Pilani 20, Shastri Nagar Pilani, (RAJASTHAN) CHENNAI. 12. Shri Dayanand Varma 4. Shri G. Krishnankutty W-21, Greater Kailash-I 7/15, Prashant Nagar NEW DELHI-110048. Ulloor Thiruvananthapuram 13. Prof. Pardeep Sahni KERALA. Faculty of Public Administration Indira Gandhi National Open 5. Shri Agam Prakash Mathur University Vice Chancellor NEW DELHI-110068. Agra University AGRA. 14. Prof. Dr. A.M. Patwardhan 22-B, Mont Vert 6. Dr. Ramesh Mehta Pashan-Sus Road 235, Rehora Pashan, JAMMU-180005. PUNE-411021. 7. Mr. M. P. Goel 15. Dr. P.V. Naik 62, Kapil Vihar Department of Physics Pitampura V.J.T.I., Matunga NEW DELHI. MUMBAI-400019. 8. Mrs. S. Devasundram 8, Elango Street Subramania Nagar Salem-636005. - 2 - 16. Dr. Shashikant Anand Kelkar 24. Prof. P.K. Gupta FNA 32 East Sion F-119, Shastri Nagar ‘Prayog’ Gr. Fl. MEERUT-250004. MUMBAI-400022. 25. Dr. A.M. Bendre 17. Dr. S.S. Awasthy 49, Golden Avenue-I Secretary General Roorkee Road Authors Guild of India MEERUT. F-12, Jangpura Extension New Delhi-110014. 26. Dr. Bindeshwar Pathak, Sulabh International Social 18. Dr. Hiralal Bachhotia Service Organisation, K40 F Saket Sulabh Gram, RZ-83, New Delhi. -
031018-TH -M-5-When Musi Was in Spate
After the deluge With homes and bridges destroyed, the city wasn’t the same * KALAKRITI ARCHIVES ter receded. Purana Pul stood strong but the approach to the bridge from both banks were cut off; several bridges were breached but Chaderghat bridge was most the most affected — it partially col- lapsed. The old and new parts of the city were cut off. Rescue operation involved searching for people stranded in- side their homes, on rooftops, and clinging on to trees. Search opera- tions continued for days, looking for bodies within the rubble. One of the photographs shows corpses now on display at Kalakriti Art Gal- on a heap of ruins after a building lery. The exhibition ‘After the De- collapsed. luge: Memories of the Flood’ held A portion of the City Wall bet- When Musi in collaboration with Krishnakriti ween Afzal Gunj and Musallam Foundation shows us how Hydera- Jung bridges was broken. Elsewh- bad was brought to its knees. ere, debris was all that remained The images, in gelatine silver of shops outside Dewan Deodi. was in spate prints, reveal the extent of dam- Victoria Zenana Hospital and Afzal age to the city’s bridges, bazaars, Gunj hospital suffered ceiling and hospitals, bungalows and other re- roof collapses. Those stranded in Kalakriti Archives encapsulates memories sidential spaces. It all began with a Begum Bazaar were rescued by cyclone in Bay of Bengal and from boats. of the great floods of 1908 through September 27 evening, as Musi be- original photographs gan to swell owing to torrential Long road to normalcy rains. -

Tender for Pickup and Door Delivery of Parcels and Couriers for Apsrtc Logistics for a Period of One Year and Extendable by Two More Years at the Following Cities
1 TENDER NOTIFICATION NO: Log-01/2018 CM (Comm), Tender ID-228259. APSRTC TENDER FOR PICKUP AND DOOR DELIVERY OF PARCELS AND COURIERS FOR APSRTC LOGISTICS FOR A PERIOD OF ONE YEAR AND EXTENDABLE BY TWO MORE YEARS AT THE FOLLOWING CITIES. 1. VIJAYAWADA 2. VISAKHAPATNAM 3. HYDERABAD AND SECUNDERABAD Signature of the tenderer 2 DISCLAIMER The information contained in this Tender document or subsequently provided to tenderers, whether in document or verbal or any other form by or on behalf of Andhra Pradesh State Road Transport Corporation (APSRTC) by any of its employees or advisors, is provided to tenderers on the terms and conditions set out in this Tender document and such other terms and conditions subject to which such information is provided. The purpose of this Tender document is to provide interested parties with information that may be useful to them in eliciting their proposals pursuant to this Tender document. This Tender document may not be appropriate for all persons, and it is not possible for APSRTC, its employees or advisors to consider the investment objectives, financial situation and particular needs of each party who reads or uses this Tender document. This Tender document includes statements, which reflect various assumptions and assessments made by APSRTC in relation to the Contract. Such assumptions, assessments and statements do not purport to contain all the information that each tenderer may require. The assumptions, assessments, statements and information contained in this Tender document, may not be complete, accurate, adequate or correct. Each tenderer should, therefore, conduct his/its own investigations and analysis and should check the accuracy, adequacy, correctness, reliability and completeness of the assumptions, assessments, statements and information contained in this Tender document and obtain independent advice from appropriate sources. -
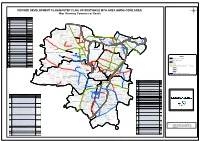
(HMDA CORE AREA) Map Showing Commercial Roads
REVISED DEVELOPMENT PLAN(MASTER PLAN) OF ERSTWHILE MCH AREA (HMDA CORE AREA) Map Showing Commercial Roads . ROADS UNDER CATEGORY C SNO ROAD NAME Osmania University Campus Junction to 6 No. Bus Stop Junction 1 C1 (Amberpet Road):Via. Shivam Road, Tilak Road Junction. Mehdipatnam Junction to Muslim Jung Bridge: T 2 Via. Asif Nagar Junction, Noble Talkies, Bhoiguda Kaman, Manghalghat C2 o w a r d N s H M (Prakash Talkies) and Asif Nagar Junction to Tappachaputra Police Station. 9 u m b a B i G Around Charminar: R a i M l u T £ o m w b Via. Gulzar House, Mittika Sher, Lad Bazar Junction, Methigalli, a a r i d 3 C3 s Panchmohalla, Mogulpura (Fire Service) Saradar Mahal Road Junction, Miralam (Police Station), Gulzar House. Sanatnagar East Allahuddin Kot i Hussaini Alam Junction to Salarjung Bridge Junction: (Sanath N agar) Via. Murgi Chowk, Kurshid Jha Dewdi Road, Himmatpura, Hari Bowli 4 C4 Junction, Talab Katta Junction, Bibi Bazar Junction, Asher Shana, Darulshifa (old MCH Office). Nehru Statue (Shalibanda) to Junction on Chandrayanagutta Road: £ 5 C5 Sanatnagar Via. Laldarwaja Road, Uppuguda Railway Station, Pool Bagh. Erragadda Road No.12, Banjara Hills, from Road No.1 and 12 Junction to Police Begumpet 6 C6 out Post (New D.No.1623 and 492). Road No.10, Banjara Hills, from Road No.1 and 10 Junction up to 7 C7 Junction at premises No.8-2-596/5 (Bank of Baroda). B K Guda £ St. Mary’s Road from Keys High School Junction to S.D.Road: 8 C8 Via.