Physiologic Flow Related Signal Intensity in Dural Sinuses on Time
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anatomical Variants of the Emissary Veins: Unilateral Aplasia of Both the Sigmoid Sinus and the Internal Jugular Vein and Development of the Petrosquamosal Sinus
Folia Morphol. Vol. 70, No. 4, pp. 305–308 Copyright © 2011 Via Medica C A S E R E P O R T ISSN 0015–5659 www.fm.viamedica.pl Anatomical variants of the emissary veins: unilateral aplasia of both the sigmoid sinus and the internal jugular vein and development of the petrosquamosal sinus. A rare case report O. Kiritsi1, G. Noussios2, K. Tsitas3, P. Chouridis4, D. Lappas5, K. Natsis6 1“Hippokrates” Diagnostic Centre of Kozani, Greece 2Laboratory of Anatomy in Department of Physical Education and Sports Medicine at Serres, “Aristotle” University of Thessaloniki, Greece 3Orthopaedic Department of General Hospital of Kozani, Greece 4Department of Otorhinolaryngology of “Hippokration” General Hospital of Thessaloniki, Greece 5Department of Anatomy of Medical School of “National and Kapodistrian” University of Athens, Greece 6Department of Anatomy of the Medical School of “Aristotle” University of Thessaloniki, Greece [Received 9 August 2011; Accepted 25 September 2011] We report a case of hypoplasia of the right transverse sinus and aplasia of the ipsilateral sigmoid sinus and the internal jugular vein. In addition, development of the petrosquamosal sinus and the presence of a large middle meningeal sinus and sinus communicans were observed. A 53-year-old Caucasian woman was referred for magnetic resonance imaging (MRI) investigation due to chronic head- ache. On the MRI scan a solitary meningioma was observed. Finally MR 2D veno- graphy revealed this extremely rare variant. (Folia Morphol 2011; 70, 4: 305–308) Key words: hypoplasia, right transverse sinus, aplasia, ipsilateral sigmoid sinus, petrosquamosal sinus, internal jugular vein INTRODUCTION CASE REPORT Emissary veins participate in the extracranial A 53-year-old Caucasian woman was referred for venous drainage of the dural sinuses of the poste- magnetic resonance imaging (MRI) investigation due to rior fossa, complementary to the internal jugular chronic frontal headache complaints. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity
Published July 16, 2020 as 10.3174/ajnr.A6647 ORIGINAL RESEARCH INTERVENTIONAL Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity M. Shapiro, K. Srivatanakul, E. Raz, M. Litao, E. Nossek, and P.K. Nelson ABSTRACT BACKGROUND AND PURPOSE: Tentorial sinus venous channels within the tentorium cerebelli connecting various cerebellar and su- pratentorial veins, as well as the basal vein, to adjacent venous sinuses are a well-recognized entity. Also well-known are “dural lakes” at the vertex. However, the presence of similar channels in the supratentorial dura, serving as recipients of the Labbe, super- ficial temporal, and lateral and medial parieto-occipital veins, among others, appears to be underappreciated. Also under-recog- nized is the possible role of these channels in the angioarchitecture of certain high-grade dural fistulas. MATERIALS AND METHODS: A retrospective review of 100 consecutive angiographic studies was performed following identification of index cases to gather data on the angiographic and cross-sectional appearance, location, length, and other features. A review of 100 consecutive dural fistulas was also performed to identify those not directly involving a venous sinus. RESULTS: Supratentorial dural venous channels were found in 26% of angiograms. They have the same appearance as those in the tentorium cerebelli, a flattened, ovalized morphology owing to their course between 2 layers of the dura, in contradistinction to a rounded cross-section of cortical and bridging veins. They are best appreciated on angiography and volumetric postcontrast T1- weighted images. Ten dural fistulas not directly involving a venous sinus were identified, 6 tentorium cerebelli and 4 supratentorial. -

The Condylar Canal and Emissary Vein—A Comprehensive and Pictorial Review of Its Anatomy and Variation
Child's Nervous System (2019) 35:747–751 https://doi.org/10.1007/s00381-019-04120-4 REVIEW ARTICLE The condylar canal and emissary vein—a comprehensive and pictorial review of its anatomy and variation Stefan Lachkar1 & Shogo Kikuta1 & Joe Iwanaga1,2 & R. Shane Tubbs1,3 Received: 6 March 2019 /Accepted: 8 March 2019 /Published online: 21 March 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract The condylar canal and its associated emissary vein serve as vital landmarks during surgical interventions involving skull base surgery. The condylar canal serves to function as a bridge of communication from the intracranial to extracranial space. Variations of the condylar canal are extremely prevalent and can present as either bilateral, unilateral, or completely absent. Anatomical variations of the condylar canal pose as a potential risk to surgeons and radiologist during diagnosis as it could be misinterpreted for a glomus jugular tumor and require surgical intervention when one is not needed. Few literature reviews have articulated the condylar canal and its associated emissary vein through extensive imaging. This present paper aims to further the knowledge of anatomical variations and surgical anatomy involving the condylar canal through high-quality computed tomography (CT) images with cadaveric and dry bone specimens that have been injected with latex to highlight emissary veins arising from the condylar canal. Keywords Posterior condylar canal . Anatomical variation . Anatomy . Cadaver . Skull . Emissary vein Introduction the posterior cranial fossa near or in the jugular fossa (Figs. 3 and 4)[2, 7, 9]. Its contents include the condylar emissary The condylar canal serves as a vital passageway for venous vein, which connects the sigmoid sinus or superior jugular circulation (condylar emissary vein) (Fig. -

Hemodynamic Features in Normal and Cavernous Sinus Dural ORIGINAL RESEARCH Arteriovenous Fistulas
Published September 6, 2012 as 10.3174/ajnr.A3252 Superior Petrosal Sinus: Hemodynamic Features in Normal and Cavernous Sinus Dural ORIGINAL RESEARCH Arteriovenous Fistulas R. Shimada BACKGROUND AND PURPOSE: Normal hemodynamic features of the superior petrosal sinus and their H. Kiyosue relationships to the SPS drainage from cavernous sinus dural arteriovenous fistulas are not well known. We investigated normal hemodynamic features of the SPS on cerebral angiography as well as the S. Tanoue frequency and types of the SPS drainage from CSDAVFs. H. Mori T. Abe MATERIALS AND METHODS: We evaluated 119 patients who underwent cerebral angiography by focusing on visualization and hemodynamic status of the SPS. We also reviewed selective angiography in 25 consecutive patients with CSDAVFs; we were especially interested in the presence of drainage routes through the SPS from CSDAVFs. RESULTS: In 119 patients (238 sides), the SPS was segmentally (anterior segment, 37 sides; posterior segment, 82 sides) or totally (116 sides) demonstrated. It was demonstrated on carotid angiography in 11 sides (4.6%), receiving blood from the basal vein of Rosenthal or sphenopetrosal sinus, and on vertebral angiography in 235 sides (98.7%), receiving blood from the petrosal vein. No SPSs were demonstrated with venous drainage from the cavernous sinus. SPS drainage was found in 7 of 25 patients (28%) with CSDAVFs. CSDAVFs drained through the anterior segment of SPS into the petrosal vein without draining to the posterior segment in 3 of 7 patients (12%). CONCLUSIONS: The SPS normally works as the drainage route receiving blood from the anterior cerebellar and brain stem venous systems. -

Sigmoid Sinus Diverticulum, Dehiscence, and Venous Sinus Stenosis: Potential Causes of Pulsatile Tinnitus in Patients with Idiopathic Intracranial Hypertension?
Published July 13, 2017 as 10.3174/ajnr.A5277 ORIGINAL RESEARCH HEAD & NECK Sigmoid Sinus Diverticulum, Dehiscence, and Venous Sinus Stenosis: Potential Causes of Pulsatile Tinnitus in Patients with Idiopathic Intracranial Hypertension? X J.A. Lansley, X W. Tucker, X M.R. Eriksen, X P. Riordan-Eva, and X S.E.J. Connor ABSTRACT BACKGROUND AND PURPOSE: Pulsatile tinnitus is experienced by most patients with idiopathic intracranial hypertension. The patho- physiology remains uncertain; however, transverse sinus stenosis and sigmoid sinus diverticulum/dehiscence have been proposed as potential etiologies. We aimed to determine whether the prevalence of transverse sinus stenosis and sigmoid sinus diverticulum/ dehiscence was increased in patients with idiopathic intracranial hypertension and pulsatile tinnitus relative to those without pulsatile tinnitus and a control group. MATERIALS AND METHODS: CT vascular studies of patients with idiopathic intracranial hypertension with pulsatile tinnitus (n ϭ 42), without pulsatile tinnitus (n ϭ 37), and controls (n ϭ 75) were independently reviewed for the presence of severe transverse sinus stenosis and sigmoid sinus diverticulum/dehiscence according to published criteria. The prevalence of transverse sinus stenosis and sigmoid sinus diverticulum/dehiscence in patients with idiopathic intracranial hypertension with pulsatile tinnitus was compared with that in the nonpulsatile tinnitus idiopathic intracranial hypertension group and the control group. Further comparisons included differing degrees of transverse sinus stenosis (50% and 75%), laterality of transverse sinus stenosis/sigmoid sinus diverticulum/dehiscence, and ipsilateral transverse sinus stenosis combined with sigmoid sinus diverticulum/dehiscence. RESULTS: Severe bilateral transverse sinus stenoses were more frequent in patients with idiopathic intracranial hypertension than in controls (P Ͻ .001), but there was no significant association between transverse sinus stenosis and pulsatile tinnitus within the idiopathic intracranial hypertension group. -

Dural Venous Sinuses Dr Nawal AL-Shannan Dural Venous Sinuses ( DVS )
Dural venous sinuses Dr Nawal AL-Shannan Dural venous sinuses ( DVS ) - Spaces between the endosteal and meningeal layers of the dura Features: 1. Lined by endothelium 2. No musculare tissue in the walls of the sinuses 3. Valueless 4.Connected to diploic veins and scalp veins by emmissary veins .Function: receive blood from the brain via cerebral veins and CSF through arachnoid villi Classification: 15 venous sinuses Paried venous sinuses Unpaired venous sinuses ( lateral in position) • * superior sagittal sinus • * cavernous sinuses • * inferior sagittal sinus • * superior petrosal sinuses • * occipital sinus • * inferior petrosal sinuses • * anterior intercavernous • * transverse sinuses • sinus * sigmoid sinuses • * posterior intercavernous • * spheno-parietal sinuses • sinus • * middle meningeal veins • * basilar plexuses of vein SUPERIOR SAGITTAL SINUS • Begins in front at the frontal crest • ends behind at the internal occipital protuberance diliated to form confluence of sinuses and venous lacunae • • The superior sagittal sinus receives the following : • 1- Superior cerebral veins • 2- dipolic veins • 3- Emissary veins • 4- arachnoid granulation • 5- meningeal veins Clinical significance • Infection from scalp, nasal cavity & diploic tissue • septic thrombosis • CSF absorption intra cranial thrombosis (ICT) • Inferior sagittal sinus - small channel occupy • lower free magin of falx cerebri ( post 2/3) - runs backward and • joins great cerebral vein at free margin of tentorium cerebelli to form straight sinus. • - receives cerebral -

Bilateral Transverse Sinus Hypoplasia: a Rare Case Report
J Exp Clin Neurosci, 2018, 5(1): 1-2 Case Report Bilateral Transverse Sinus Hypoplasia: A Rare Case Report Elyar Sadeghi-Hokmabadia, Masoud Poureisab, Neda Ghaemiana,*, Zahra Parsianc aNeurosciences Research Center, Tabriz University of Medical Science, Tabriz, Iran bDepartment of Radiology, Radiotherapy and Nuclear Medicine, Tabriz University of Medical Sciences, Tabriz, Iran cDepartment of Emergency Medicine, Tabriz University of Medical Sciences, Tabriz, Iran Abstract The dural sinuses are pathways for drainage of blood from brain to the internal jugular veins. Occipital sinus is a rare normal anatomical variation of dural sinuses which acts as an alternative drainage pathway Correspondence when the transverse sinuses are hypoplastic. It drains blood from skull and brain to the internal jugular Neda Ghaemian, vein. The variations can culminate in wrong diagnosis and imaging interpretation. We reported a Neurosciences Research Center, Tabriz 33 years old pregnant woman presented with headache and normal neurological examination. Magnetic University of Medical Science, Tabriz, Iran. resonance imaging and magnetic resonance venography studies revealed occipital sinus as the main Tel/Fax: +98-41-333340730 drainage pathway of the brain. Both the transverse sinuses were hypoplastic. Without considering this Email: [email protected] rare variation such conditions can culminate in wrong diagnosis, which can be prevented by reporting such rare conditions. Received: 2017-06-10 Accepted: 2017-12-12 Keywords: Transverse sinus, Hypoplasia, Headache DOI:10.13183/jecns.v%vi%i.75 ©2018 Swedish Science Pioneers, All rights reserved. Introduction symptoms. Pain did not respond to oral analgesics. She had The dural sinuses are pathways for drainage of blood from brain a history of chronic generalized deep seated and throbbing to the internal jugular veins [1]. -

Dural Venous Sinus Thrombosis with Hemorrhagic Venous Infarct
41 year old female with headache Elena G. Violari MD and Leo Wolansky MD ? Dural Venous Sinus Thrombosis with Hemorrhagic Venous Infarct Acute intraparenchymal hematoma measuring ~3 cm in diameter centered in the right temporal lobe with surrounding vasogenic edema. There is mass effect upon and effacement of the adjacent cortical sulci and negligible midline shift Non-contrast CT, axial view Hyperdensity is seen in the right transverse sinus (yellow arrow) in comparison with the normal left transverse/ sigmoid sinus junction (orange arrow) Non-contrast CT, axial view Acute/Hyperacute hematoma T2 AXIAL Acute/Hyperacute hematoma in the right temporal lobe with a hematocrit effect (yellow arrow). The posterior portion of the hematoma (blue arrow) demonstrates hypointense signal intensity on T2-weighted images, typical of dependently layering RBC’s. The anterior- most portion is hyperintense on T2-weighted images (plasma). There is surrounding vasogenic edema (orange arrows). T2 AXIAL Filling defect seen on the volumetric contrast- enhanced T1-weighted images, typical of acute thrombus involving the right transverse sigmoid sinus junction (yellow arrow). T1 CORONAL POST T1 AXIAL POST Filling defect seen on the volumetric contrast-enhanced T1-weighted images typical of acute thrombus throughout the right transverse sinus (blue arrows) & sigmoid sinus (violet arrow) extending into the jugular bulb (orange arrow). Compare with nonthrombosed left sigmoid and jugular (yellow arrows). Superiorly (not shown), there was extension into a cortical vein probably representing the anastomotic vein of Labbe, which coursed immediately superficial to the hematoma and is thought to represent the immediate cause of the hemorrhage. Non-contrast CT, axial view Non-contrast CT, coronal view Asymmetric hyperdensity of thrombus (yellow arrows) is visible on CT when compared with healthy sinus contralaterally (orange arrows). -

The Inferior Petrosal Sinus: a Comprehensive Review with Emphasis on Clinical Implications
Childs Nerv Syst (2014) 30:831–834 DOI 10.1007/s00381-014-2378-7 REVIEW PAPER The inferior petrosal sinus: a comprehensive review with emphasis on clinical implications Martin M. Mortazavi & Christoph J. Griessenauer & Sanjay Krishnamurthy & Ketan Verma & Marios Loukas & R. Shane Tubbs Received: 1 December 2013 /Accepted: 29 January 2014 /Published online: 14 February 2014 # Springer-Verlag Berlin Heidelberg 2014 Abstract and brain stem along its course prior to emptying into the Introduction The inferior petrosal sinus is an important com- junction of the sigmoid sinus and superior jugular bulb. In the ponent of the cerebral venous system with implications in jugular foramen, the relationship of the IPS and the cranial diagnosis and treatment of a variety of diseases such as nerves is of great importance. Embryologically, the IPS de- Cushing’s disease, carotid cavernous, and dural arteriovenous velops as a new structure connecting the anterior head vein, fistulas. precursor of the cavernous sinus, and jugular bulb vesicle Methods This manuscript will review the anatomy, embryol- vein. Endovascular access to the IPS has important diagnostic ogy, and clinical implications of the inferior petrosal sinus. and therapeutic utility for a variety of conditions involving the Conclusions Knowledge of the inferior petrosal sinus is of cavernous sinus and sellar regions. This manuscript will re- great importance for open surgical approaches to the skull view the anatomy, embryology, and important clinical impli- base and endovascular access to the cavernous sinus and sellar cations of the IPS. region. Anatomy Keywords Inferior petrosal sinus . Anatomy . Skull base . Pathology The IPS (Figs. 1, 2, 3,and4) are paired venous structures at the base of the skull that drain venous blood from the cavern- ous sinus to the junction of the sigmoid sinus and the superior Introduction jugular bulb on each side. -

Prevalence of Sigmoid Sinus Dehiscence and Diverticulum Among Adults with Skull Base Cephaloceles
ORIGINAL RESEARCH HEAD & NECK Prevalence of Sigmoid Sinus Dehiscence and Diverticulum among Adults with Skull Base Cephaloceles H. Sotoudeh, G. Elsayed, S. Ghandili, O. Shafaat, J.D. Bernstock, G. Chagoya, T. Atchley, P. Talati, D. Segar, S. Gupta, and A. Singhal ABSTRACT BACKGROUND AND PURPOSE: Cephaloceles are relatively rare conditions caused by a congenital and/or acquired skull defect. The incidence of associated venous brain anomalies with regard to cephaloceles remains to be fully elucidated. Accordingly, we sought to assess the prevalence of sigmoid sinus dehiscence and diverticula in patients with spontaneous skull base cephaloceles. MATERIALS AND METHODS: Our institutional data base was retrospectively queried from 2005 to 2018. Patients in whom sponta- neous skull base cephaloceles were identified were ultimately included in the study cohort. These patients subsequently had their sigmoid sinuses re-evaluated with focused attention on the possible presence of dehiscence and/or diverticula. RESULTS: We identified 56 patients: 12 men and 44 women. After re-evaluation of the sigmoid sinuses, evidence of dehiscence and/or diverticula was noted in 21 patients. The right sigmoid sinus was involved in 11 patients, and the left sigmoid sinus was involved in 7 patients, including 3 cases of diverticulum. In 3 patients, evidence of bilateral sigmoid sinus dehiscence and diverticula was noted. Female sex was associated with sigmoid sinus dehiscence and diverticula by univariate analysis (P ¼ .019). By linear regression, cephalocele volume was negatively associated with sigmoid sinus dehiscence and diverticula (coefficient, À2266, P value , .007, adjusted R2 ¼ 0.1077). By uni- variate logistic regression using average cephalocele volume as a cutoff, we demonstrate a statistically significant finding of lower vol- umes being associated with sigmoid sinus dehiscence and diverticula with an odds ratio of 3.58 (P ¼ .05). -
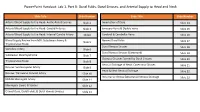
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation.