The Silver Cation (Ag+): Antibacterial Mode of Action and Mechanisms of Resistance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 6,395,889 B1 Robison (45) Date of Patent: May 28, 2002
USOO6395889B1 (12) United States Patent (10) Patent No.: US 6,395,889 B1 Robison (45) Date of Patent: May 28, 2002 (54) NUCLEIC ACID MOLECULES ENCODING WO WO-98/56804 A1 * 12/1998 ........... CO7H/21/02 HUMAN PROTEASE HOMOLOGS WO WO-99/0785.0 A1 * 2/1999 ... C12N/15/12 WO WO-99/37660 A1 * 7/1999 ........... CO7H/21/04 (75) Inventor: fish E. Robison, Wilmington, MA OTHER PUBLICATIONS Vazquez, F., et al., 1999, “METH-1, a human ortholog of (73) Assignee: Millennium Pharmaceuticals, Inc., ADAMTS-1, and METH-2 are members of a new family of Cambridge, MA (US) proteins with angio-inhibitory activity', The Journal of c: - 0 Biological Chemistry, vol. 274, No. 33, pp. 23349–23357.* (*) Notice: Subject to any disclaimer, the term of this Descriptors of Protease Classes in Prosite and Pfam Data patent is extended or adjusted under 35 bases. U.S.C. 154(b) by 0 days. * cited by examiner (21) Appl. No.: 09/392, 184 Primary Examiner Ponnathapu Achutamurthy (22) Filed: Sep. 9, 1999 ASSistant Examiner William W. Moore (51) Int. Cl." C12N 15/57; C12N 15/12; (74) Attorney, Agent, or Firm-Alston & Bird LLP C12N 9/64; C12N 15/79 (57) ABSTRACT (52) U.S. Cl. .................... 536/23.2; 536/23.5; 435/69.1; 435/252.3; 435/320.1 The invention relates to polynucleotides encoding newly (58) Field of Search ............................... 536,232,235. identified protease homologs. The invention also relates to 435/6, 226, 69.1, 252.3 the proteases. The invention further relates to methods using s s s/ - - -us the protease polypeptides and polynucleotides as a target for (56) References Cited diagnosis and treatment in protease-mediated disorders. -

Comparative Study of Disinfectants for Use in Low-Cost Gravity Driven Household Water Purifiers Rajshree A
443 © IWA Publishing 2013 Journal of Water and Health | 11.3 | 2013 Comparative study of disinfectants for use in low-cost gravity driven household water purifiers Rajshree A. Patil, Shankar B. Kausley, Pradeep L. Balkunde and Chetan P. Malhotra ABSTRACT Point-of-use (POU) gravity-driven household water purifiers have been proven to be a simple, low- Rajshree A. Patil Shankar B. Kausley (corresponding author) cost and effective intervention for reducing the impact of waterborne diseases in developing Pradeep L. Balkunde Chetan P. Malhotra countries. The goal of this study was to compare commonly used water disinfectants for their TCS Innovation Labs – TRDDC, fi 54B, Hadapsar Industrial Estate, feasibility of adoption in low-cost POU water puri ers. The potency of each candidate disinfectant Pune - 411013, was evaluated by conducting a batch disinfection study for estimating the concentration of India E-mail: [email protected] disinfectant needed to inactivate a given concentration of the bacterial strain Escherichia coli ATCC 11229. Based on the concentration of disinfectant required, the size, weight and cost of a model purifier employing that disinfectant were estimated. Model purifiers based on different disinfectants were compared and disinfectants which resulted in the most safe, compact and inexpensive purifiers were identified. Purifiers based on bromine, tincture iodine, calcium hypochlorite and sodium dichloroisocyanurate were found to be most efficient, cost effective and compact with replacement parts costing US$3.60–6.00 for every 3,000 L of water purified and are thus expected to present the most attractive value proposition to end users. Key words | disinfectant, drinking water, E. -

Silver Nanoparticle Nanocomposite Filaments Produced by an In-Situ Reduction Reactive Melt Mixing Process
biomimetics Article Three-Dimensional Printed Antimicrobial Objects of Polylactic Acid (PLA)-Silver Nanoparticle Nanocomposite Filaments Produced by an In-Situ Reduction Reactive Melt Mixing Process Nectarios Vidakis 1, Markos Petousis 1,* , Emmanouel Velidakis 1, Marco Liebscher 2 and Lazaros Tzounis 3 1 Mechanical Engineering Department, Hellenic Mediterranean University, Estavromenos, 71004 Heraklion, Crete, Greece; [email protected] (N.V.); [email protected] (E.V.) 2 Institute of Construction Materials, Technische Universität Dresden, DE-01062 Dresden, Germany; [email protected] 3 Department of Materials Science and Engineering, University of Ioannina, 45110 Ioannina, Greece; [email protected] * Correspondence: [email protected]; Tel.: +30-2810-37-9227 Received: 14 August 2020; Accepted: 31 August 2020; Published: 2 September 2020 Abstract: In this study, an industrially scalable method is reported for the fabrication of polylactic acid (PLA)/silver nanoparticle (AgNP) nanocomposite filaments by an in-situ reduction reactive melt mixing method. The PLA/AgNP nanocomposite filaments have been produced initially + reducing silver ions (Ag ) arising from silver nitrate (AgNO3) precursor mixed in the polymer melt to elemental silver (Ag0) nanoparticles, utilizing polyethylene glycol (PEG) or polyvinyl pyrrolidone (PVP), respectively, as macromolecular blend compound reducing agents. PEG and PVP were added at various concentrations, to the PLA matrix. The PLA/AgNP filaments have been used to manufacture 3D printed antimicrobial (AM) parts by Fused Filament Fabrication (FFF). The 3D printed PLA/AgNP parts exhibited significant AM properties examined by the reduction in Staphylococcus aureus (S. aureus) and Escherichia coli (E. coli) bacteria viability (%) experiments at 30, 60, and 120 min duration of contact (p < 0.05; p-value (p): probability). -

Silver As a Drinking-Water Disinfectant
Silver as a drinking-water disinfectant Silver as a drinking-water disinfectant Alternative drinking-water disinfectants: silver ISBN 978-92-4-151369-2 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Alternative drinking-water disinfectants: bromine, iodine and silver. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. -

Serine Proteases with Altered Sensitivity to Activity-Modulating
(19) & (11) EP 2 045 321 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2009 Bulletin 2009/15 C12N 9/00 (2006.01) C12N 15/00 (2006.01) C12Q 1/37 (2006.01) (21) Application number: 09150549.5 (22) Date of filing: 26.05.2006 (84) Designated Contracting States: • Haupts, Ulrich AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 51519 Odenthal (DE) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Coco, Wayne SK TR 50737 Köln (DE) •Tebbe, Jan (30) Priority: 27.05.2005 EP 05104543 50733 Köln (DE) • Votsmeier, Christian (62) Document number(s) of the earlier application(s) in 50259 Pulheim (DE) accordance with Art. 76 EPC: • Scheidig, Andreas 06763303.2 / 1 883 696 50823 Köln (DE) (71) Applicant: Direvo Biotech AG (74) Representative: von Kreisler Selting Werner 50829 Köln (DE) Patentanwälte P.O. Box 10 22 41 (72) Inventors: 50462 Köln (DE) • Koltermann, André 82057 Icking (DE) Remarks: • Kettling, Ulrich This application was filed on 14-01-2009 as a 81477 München (DE) divisional application to the application mentioned under INID code 62. (54) Serine proteases with altered sensitivity to activity-modulating substances (57) The present invention provides variants of ser- screening of the library in the presence of one or several ine proteases of the S1 class with altered sensitivity to activity-modulating substances, selection of variants with one or more activity-modulating substances. A method altered sensitivity to one or several activity-modulating for the generation of such proteases is disclosed, com- substances and isolation of those polynucleotide se- prising the provision of a protease library encoding poly- quences that encode for the selected variants. -
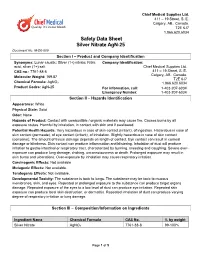
Safety Data Sheet Silver Nitrate Agn-25 Document No
Chief Medical Supplies Ltd. 411 – 19 Street, S. E. Calgary, AB., Canada. T2E 6J7 1.866.620.6034 Safety Data Sheet Silver Nitrate AgN-25 Document No. M-D6-009 Section I – Product and Company Identification Synonyms: Lunar caustic; Silver (1+) nitrate; Nitric Company Identification: acid, silver (1+) salt Chief Medical Supplies Ltd. CAS no.: 7761-88-8 411 – 19 Street, S. E. Calgary, AB., Canada. Molecular Weight: 169.87 T2E 6J7 Chemical Formula: AgNO3 1.866.620.6034 Product Codes: AgN-25 For information, call: 1-403-207-6034 Emergency Number: 1-403-207-6034 Section II – Hazards Identification Appearance: White Physical State: Solid Odor: None Hazards of Product: Contact with combustible / organic materials may cause fire. Causes burns by all exposure routes. Harmful by inhalation, in contact with skin and if swallowed. Potential Health Hazards: Very hazardous in case of skin contact (irritant), of ingestion. Hazardous in case of skin contact (permeate), of eye contact (irritant), of inhalation. Slightly hazardous in case of skin contact (corrosive). The amount of tissue damage depends on length of contact. Eye contact can result in corneal damage or blindness. Skin contact can produce inflammation and blistering. Inhalation of dust will produce irritation to gastro-intestinal or respiratory tract, characterized by burning, sneezing and coughing. Severe over- exposure can produce lung damage, choking, unconsciousness or death. Prolonged exposure may result in skin burns and ulcerations. Over-exposure by inhalation may cause respiratory irritation. Carcinogenic Effects: Not available Mutagenic Effects: Not available. Teratogenic Effects: Not available. Developmental Toxicity: The substance is toxic to lungs. -

Effects of Some Chemicals on Vase Life of Some Cut Flowers I
J. Plant Production, Mansoura Univ., Vol. 8 (1): 49 - 53, 2017 Effects of Some Chemicals on Vase Life of Some Cut Flowers I. Effect of 8-Hydroxyquinoline Sulfate, Silver Nitrate, Silver Nano Particles and Chitosan on Vase Life and Quality of Cut Rose Flowers (Rosa hybrida. Cv. “Black Magic”) Abdel-Kader, H. H.1; A. M. Hamza1; T. T. Elbaz2 and S. M. Eissa2 1 Veg. and Flor. Dept., Fac. of Agric., Mansoura Unive. 2 Ornam, Plants and Lands. Gard. Res. Dept., Hort. Res. Inst., Agric. Res. Cent., Giza ABSTRACT This investigation was carried out during 2015 and 2016 seasons to determine whether the selected chemical agents could be used to improve the postharvest quality of Rosa hybrida L.cv. “Black Magic” cut flowers. Freshly cut flowers were placed in glass cylinders containing 100 ml of preservative solutions [8-hydroxyquinoline sulfate (8-HQS) at 200 ppm, silver nitrate (AgNO3) at 10 ppm, Chitosan at 50, 75 or 100 ppm silver nano-particles (SN) at 5, 10 or 15 ppm, and distilled water as a control treatment].All preservative solutions and the control treatment included sucrose at 20 g/l. Compared to the control, treatments which contained of (AgNO3) or (SN) improved the quality and vase life of the flowers. They were more effective in promoting water uptake, increasing fresh weight of the flower and water balance so that the vase life of cut flowers were extended to 13.67 and 12 days during the first and second seasons, respectively. The results of bacterial count in the vase solution and the Scanning Electron Microscopy (SEM) pictures of the cut base of the stem indicated that (AgNO3) or (SN) strongly reduced bacterial population in both the vase solution and the cut stem base. -

Silver Nitrate Complexes of Nitrogen-Containing
Silver Nitrate Complexes of Nitrogen-Containing Heterocycles Hubert Schmidbaur*, Angelika Mair, Gerhard Müller*, Joachim Lachmann+, and Siegfried Gamper+ Anorganisch-chemisches Institut der Technischen Universität München, Lichtenbergstraße 4, D-8046 Garching Z. Naturforsch. 46b, 912-918 (1991); received February 19, 1991 Silver Complexes, Nitrogen Heterocycles, Pyrazole. Triazole, 8 -Amino-quinoline Pyrazole, 1,2,4-triazole, and 8 -amino-quinoline form complexes as neutral ligands with sil ver nitrate in slightly acidic aqueous medium. With pyrazole a 2:1 complex (1) is obtained. The crystal structure determination revealed an ionic structure with independent N 0 3~ anions and centrosymmetrical (pyr) 2Ag+ cations with a linear coordination geometry at the silver atoms. The reactions with 1,2,4-triazole and 8 -amino-quinoline yield dimeric 1:1 complexes (2, 3), in which the silver atoms are bridged by the ligands and have short contacts with nitrate oxygen atoms. The coordination geometry of the metals can thus be described as distorted tetrahedral. A 1 :1 complex with 2,3-diphenyl-1,2,4-triazole (2a) and a 2:1 complex with 8 -hydroxy-quino- line (4) have also been prepared, but not characterized in detail. Introduction prepared and characterized a series of complexes Complex formation of silver(I) cations by am of silver nitrate with pyrazole, (diphenyl)triazole, monia and amines has been well established in an 8 -amino-quinoline, and 8 -hydroxy-quinoline. alytical chemistry and chemical technology of sil ver for more than a century. However, nitrogen- Preparation and Properties of the Complexes containing heterocycles have also been among the early complexing agents. -

Virulence Factors in Staphylococcus Associated with Small Ruminant Mastitis: Biofilm Production and Antimicrobial Resistance Genes
antibiotics Article Virulence Factors in Staphylococcus Associated with Small Ruminant Mastitis: Biofilm Production and Antimicrobial Resistance Genes Nara Cavalcanti Andrade 1, Marta Laranjo 1 , Mateus Matiuzzi Costa 2 and Maria Cristina Queiroga 1,3,* 1 MED–Mediterranean Institute for Agriculture, Environment and Development, Instituto de Investigação e Formação Avançada, Universidade de Évora, Pólo da Mitra, Ap. 94, 7006-554 Évora, Portugal; [email protected] (N.C.A.); [email protected] (M.L.) 2 Federal University of the São Francisco Valley, BR 407 Highway, Nilo Coelho Irrigation Project, s/n C1, Petrolina 56300-000, PE, Brazil; [email protected] 3 Departamento de Medicina Veterinária, Escola de Ciências e Tecnologia, Universidade de Évora, Pólo da Mitra, Ap. 94, 7006-554 Évora, Portugal * Correspondence: [email protected]; Tel.: +351-266-740-800 Abstract: Small ruminant mastitis is a serious problem, mainly caused by Staphylococcus spp. Different virulence factors affect mastitis pathogenesis. The aim of this study was to investigate virulence factors genes for biofilm production and antimicrobial resistance to β-lactams and tetracyclines in 137 staphylococcal isolates from goats (86) and sheep (51). The presence of coa, nuc, bap, icaA, icaD, blaZ, mecA, mecC, tetK, and tetM genes was investigated. The nuc gene was detected in all S. aureus isolates and in some coagulase-negative staphylococci (CNS). None of the S. aureus isolates carried the bap gene, while 8 out of 18 CNS harbored this gene. The icaA gene was detected in Citation: Andrade, N.C.; Laranjo, M.; S. aureus and S. warneri, while icaD only in S. aureus. None of the isolates carrying the bap gene Costa, M.M.; Queiroga, M.C. -
Table of Contents
An Investigation of Staphylococcus aureus and Related Species From Flood Affected and Other Environmental Sources A Thesis in Molecular Microbiology by Nadeesha Samanmalee Jayasundara BSc (Environmental Conservation & Management) School of Biomedical Science, Institute of Health & Biomedical Innovation Queensland University of Technology Brisbane, Australia Thesis submitted to Queensland University of Technology in fulfilment of the requirements for the degree of Masters of Applied Science (Research) May 2014 2 Abstract The genus Staphylococcus consists of 45 species and is widely distributed across environments such as skin and mucous membranes of humans and animals, as well as in soil, water and air. S. aureus and S. epidermidis are the most commonly associated species with human infections. Hence, most studies have focused on clinical and clinically sourced staphylococci. In addition, S. haemoliticus, S. intermidius, S. delphini, and S. saprophiticus are also considered potentially pathogenic members of the genus. Although staphylococci are distributed in various environments, there have been very few studies examining residential air as a reservoir of clinically significant pathogens, particularly Staphylococcus species. As a result, airborne transmission of staphylococci, and associated health risks, remains unclear. This study included not only residential air but also air samples from flood affected houses. Flood water can be considered as a potential carrier of pathogenic bacteria, because flood water can be affected by residential septic systems, municipal sanitary sewer systems, hospital waste, agricultural lands/operations and wastewater treatment plants. Even after the flood waters recede, microorganisms that are transported in water can remain in soil, in or on plant materials and on numerous other surfaces. Therefore, there is a great concern for use of previously flooded indoor and outdoor areas. -

Current Challenges of Veterinary Microbiological
POST. MIKROBIOL., CURRENT CHALLENGES OF VETERINARY MICROBIOLOGICAL 2018, 57, 3, 270–277 http://www.pm.microbiology.pl DIAGNOSTICS CONCERNING THE SUSCEPTIBILITY DOI: 10.21307/PM-2018.57.3.270 OF STAPHYLOCOCCI TO ANTIBIOTICS Magdalena Kizerwetter-Świda*, Dorota Chrobak-Chmiel, Magdalena Rzewuska Division of Microbiology, Department of Preclinical Sciences, Faculty of Veterinary Medicine, Warsaw University of Life Sciences-SGGW, Poland Submitted in April, accepted in May 2018 Abstract: Staphylococci belong to bacteria often isolated from clinical material obtained from animals. Unlike in human medicine, in veterinary, different species of coagulase-positive staphylococci are isolated from clinical specimens, and exceptStaphylococcus aureus, Staphylococcus pseudintermedius, and other species are also often recognized. Recently, the taxonomy of staphylococci has been updated, therefore, now it is necessary to recognize the new species as well. Currently, coagulase-negative staphylococci are considered an important group of opportunistic pathogens. The accurate identification of species within the genus Staphylococcus is important because, according to the EUCAST and CLSI recommendations, the interpretation of the results of susceptibility testing for S. aureus and coagulase-negative staphylococci is different. Furthermore, the resistance to methicillin in S. aureus strains is detected using a cefoxitin disk, whereas in the case of S. pseudintermedius – using an oxacillin disk. An important problem for veterinary microbiological laboratories -

Gronkowce Izolowane Od Zwierząt Jako Źródło Genów Kodujących Wielolekooporność Na Antybiotyki O Krytycznym Znaczeniu Dla Zdrowia Publicznego
626 DOI: 10.21521/mw.5789 Med. Weter. 2017, 73 (10), 626-631 Artykuł przeglądowy Review Gronkowce izolowane od zwierząt jako źródło genów kodujących wielolekooporność na antybiotyki o krytycznym znaczeniu dla zdrowia publicznego MAGDALENA KIZERWETTER-ŚWIDA, JOANNA PŁAWIŃSKA-CZARNAK* Zakład Mikrobiologii, Katedra Nauk Przedklinicznych, Wydział Medycyny Weterynaryjnej, Szkoła Główna Gospodarstwa Wiejskiego, ul. Ciszewskiego 8, 02-786 Warszawa *Katedra Higieny Żywności i Ochrony Zdrowia Publicznego, Wydział Medycyny Weterynaryjnej, Szkoła Główna Gospodarstwa Wiejskiego, ul. Nowoursynowska 159, 02-776 Warszawa Otrzymano 30.05.2017 Zaakceptowano 03.07.2017 Kizerwetter-Świda M., Pławińska-Czarnak J. Staphylococci isolated from animals as a source of genes that confer multidrug resistance to antimicrobial agents of critical importance to public health Summary Antimicrobial resistance (AMR) is a global public health issue. Multidrug resistance (MDR) genes that confer resistance to antimicrobials from different classes are of particular importance in the spread of AMR. Moreover, some of these MDR genes are involved in resistance to critically important antimicrobial agents used in human and veterinary medicine. Staphylococci isolated from animals and humans harbor a wide range of resistance genes, including MDR genes. Location of MDR genes on mobile genetic elements facilitate the exchange of these genes between staphylococci of animal and human origin. The emergence of resistant Staphylococcus spp. is probably linked to therapeutic or prophylactic antimicrobial use through not only direct selection of the corresponding resistance, but also indirect selections via cross-resistance and co-resistance. Judicious use of antibiotics and the knowledge of the genetics of MRD genes and other resistance genes is indispensable to counteract further dissemination of staphylococcal MDR genes.