Occlusion in Implant – Supported Prosthesis 20 Editorial Office Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Detils of Toll Colecting Bridges in Kerala( Roads
Detils of toll colecting bridges in Kerala( Roads Planning ) Average Uptodate collection per Collection in Sl No Name of Bridge Day in Rs Rs Remarks 1 Thiruvananthapuram Roads Division Nil 2 Kollam Roads Division Nil 3 Alapuzha Roads Division 1 Aroor-Arukutty 1816 7928704 2 Kainadi 131 267312 3 Thakazhi 1671 968797 4 Pathanamthitta Roads Division 1 Bunglamkadavu 225 426350 5 Kottayam Roads Division 1 Murinjapuzha 4475 1368046 6 Idukki Roads Division Nil 7 Muvattupuzha Roads Division 1 Peruvamoozhi 9375 2398000 8 Eranakulam Roads Division 1 Kumbalangi – Perumpatappu 1608 1727358 9 Trissure Roads Division 1 Krishnankodu 1647 732830 2 Mathilakam 645 1275341 3 Poovathumkadavu 520 1065085 4 Thachappally 946 469037 5 New Cochin 10650 21256446 6 Pulikkakadavu 1283 2260134 7 Njaralakadavu 366 723600 8 Pulikkakadavu 575 1291055 10 Palakkadu Roads Division 1 Kalikkavu 819 1375100 11 Manjeri Roads Division 1 Karimpuzhakadavu 430 1494073 2 Srayilkadavu 263 170804 3 Panampuzhakadavu 452 676477 4 Kadalundikadavu 938 792703 5 Edaserrykadavu 62 37284 12 Kozhikkode Roads Division 1 Nelliyadikadavu 655 2115486 13 Vadakara Roads Division Nil 14 Wayanadu Roads Division 1 Koodalkadavu 225 458128 15 Kannoor Roads Division 1 Muttam- Palacode 90 477782 2 Munderykadavu 554 1231692 3 Chempallikund 64 452950 4 Ayiramthengu 42 63601 Page 1 5 Mammakunnu 472 1919335 6 Koralayi 41 199616 7 Varamkadavu 154 2526 8 Puthiyapuzhakara 84 1302 9 Pavannurkadavu 351 106567 10 Malapattam Munabukadavu 145 584925 16 Kasaragode Roads Division 1 Arayakadavu 137 201596 Page 2 Proceedings of the Chief Engineer, PWD Design &Administration, Thiruvananthapuram (Present: Sri. K . Sundaran ) Sub: Infrastructure Conference―2012―MLAs and Guests – Officers on waiting – Authorisation –reg- Order No. -

Marian College Kuttikkanam the Annual Quality Assurance Report
The Annual Quality Assurance Report (AQAR) 2010-11 marian college kuttikkanam Established: 1995 Affiliation: Mahatma Gandhi Univeristy Kerala NAAC accreditation: 'A Grade College with Potential for excellence Post Us Call Us marian college kuttikkanam Manager : +91- 4869 - 233601 Kuttikkanam P.O., Peermade Fax : +91- 4869 - 232438 Kerala, India - 685 531 Principal : +91- 4869 - 233203 Vice Principal : +91- 4869 - 233512 Office : +91- 4869 - 232203, 232654 Mail Us Visit us [email protected] www.mariancollege.org [email protected] www.mariancollege.ac.in 2010-2011 [The Annual Quality Assurance Report (AQAR)] Part A: The plan of action chalked out by the IQAC in the beginning of the year towards quality enhancement and the outcome achieved by the end of the year. Plans Outcomes CPE Status • Marian college was awarded CPE Status in March 2010. The college celebrated the CPE status on 17 May 2010.The function was presided over by His Excellency Mar Mathew Arackal, Patron of the College and the function was inaugurated by Dr. Cyriac Thomas, Member, and National Commission for Minority Educational Institutions. Mr. Anto Antony MP, Smt. E. S. Bijimol MLA, etc felicitated the gathering. Common Quality Standards • Prepared the quality standards and was presented in the staff meeting Quality Sustenance and • The seven criterion committee members Enhancement Drive 2010 and heads presented the details of the status of our regular practice , remedial mechanism and new things to practice Best Practice documentation • The best practice in each department was collected and compiled. Next year it will be published as a book Marian Annual Academic • Organized on 24 and 25 May, 2010 at Planning and evaluation of Hotel Royale Park, Alappuzha progress of action plans • Action plan devised by each Department were deliberated during the academic retreat. -

SAGY - I DETAILS of SAANSAD ADARSH GRAM YOJANA (SAGY) VILLAGES in the STATE of KERALA (Phase-I, Phase-II &Phase-III)
SAGY - I DETAILS OF SAANSAD ADARSH GRAM YOJANA (SAGY) VILLAGES IN THE STATE OF KERALA (Phase-I, Phase-II &Phase-III) Sl. Phase District Block/Sub-District Gram Panchayat Name of the MP House Constituency Name No. 1 Phase-I Alappuzha Ambalappuzha Aryad Shri K. C. Venugopal LS Alappuzha 2 Phase-I Alappuzha Cherthala Kadakkarappally Sh. Vayalar Ravi RS 3 Phase-I Alappuzha Cherthala Thaicattussery Shri A.K. Antony RS 4 Phase-I Alappuzha Kuttanad Thakazhi Sh. Suresh Kodikunnil LS Mavelikkara 5 Phase-I Ernakulam Kanayannur Udayamperur Shri P. Rajeeve RS 6 Phase-I Ernakulam Paravur Kottuvally Prof. Kuruppassery Varkey Thomas LS Ernakulam 7 Phase-I Idukki Idukki Idukki - Kanjikuzhy Shri (Adv.) Joice George LS Idukki 8 Phase-I Kannur Taliparamba Kuttiattor Smt. P.K.Sreemathi Teacher LS Kannur 9 Phase-I Kannur Thalassery Kolayad Shri K K Ragesh RS 10 Phase-I Kasaragod Vellarikkundu Kinanoor Karindalam Shri P. Karunakaran LS Kasaragod 11 Phase-I Kollam Kollam Panayam Dr. K.N. Balagopal RS 12 Phase-I Kollam Punalur Alayamon Shri N.K. Premachandran LS Kollam 13 Phase-I Kottayam Kottayam Neendoor Shri Jose K. Mani LS Kottayam 14 Phase-I Kottayam Meenachil Melukavu Shri Joy Abraham RS 15 Phase-I Kozhikode Koyilandi Chengottukavu Shri Ramachandran Mullappally LS Vadakara 16 Phase-I Kozhikode Koyilandi Kottur Shri C.P. Narayanan RS 17 Phase-I Kozhikode Thamarassery Unnikulum Shri M. K. Raghavan LS Kozhikode 18 Phase-I Malappuram Ernad Pulpatta Shri E. Ahamed LS Malappuram 19 Phase-I Malappuram Nilambur Karulai Shri P. V. Abdulwahab RS 20 Phase-I Malappuram Tirurangadi Nannambra Shri E. -
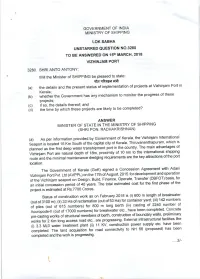
Clacfiir6{Dfr
GOVERNMENT OF INDIA MINISTRY OF SHIPPING LOK SABHA UNSTARRED QUESTION NO.328O TO BE ANSWERED ON 15th MARCH' 2018 VIZHINJAM PORT 3280. SHRI ANTO ANTONY: Will the Minister of SHIPPING be pleased to state: clacfiIr6{dfr projects Vizhinjam Port in (a) the details and the present status of implementation of at Kerala; (b)wnetnertneGovernmenthasanymechanismtomonitortheprogressofthese projects; (c) if so, the details thereof; and (d) the time by which these projects are likely to be completed? ANSWER MINISTER OF STATE IN THE MINISTRY OF SHIPPING (SHRI PON. RADHAKRISHNAN) (a)AsperinformationprovidedbyGovernmentofKerala,theVizhinjamlnternational which is Se"port is located 16 Km South of the capital city of Kerala, Thiruvananthapuram, plannedasthefirstdeepwatertranshipmentportinthecountry.Themainadvantagesof Virhinlr. port are natural depth of 1Bm, proximity of 10 nm to the international shipping key attrac'tions of the port route and the minimal maintenance dredging requirements are the location. with Adani The Government of Kerala (GoK) signed a Concession Agreement VizhinjamPortPvt.Ltd(AVPPL)onthelTthofAugust,20l5fordevelopmentandoperation oftheVizhinjamseaportonDesign,Build,Finance,Operate'Transfer(DBFOT)basis'for the first phase of the an initial concession period of 40 years. The total estimated cost for project is estimated at Rs.7700 Crores. StatusofconstructionworkasonFebruary20lsis(i)600mlengthofbreakwater (outof3100m);(ii)33Haofreclamation(outof53Ha)forcontaineryard;(iii)142numbers of of piles (out of 615 numbers) for 800 m long berth (iv) casting ol 2240 number completed. concrete ,lccropode-lt (out of 17000 numbers) for breakwater etc., have been walls, preliminary pre.casting works of structural members of berth, construction of boundary infrastructural facilities like works for 2 Km long access road etc., are progressing. External power supply etc have been (i) 3.3 MLD water ireatment plant (ii) 11 KV, construction (proposed) has been completed. -

Kerala Legislative Assembly
KERALA LEGISLATIVE ASSEMBLY Phone Numbers Designation, Name, Constituency Residential * Residence/ Address & Location Direct EPABX Mobile SPEAKER SHRI P. SREERAMAKRISHNAN 2305830 3003 2302698 “Neethi”, (48-Ponnani) 3002 2513014 Legislature Complex, Room No. 515, 3035 2512393 Vikas Bhavan P.O., I Floor, Assembly Building. 3007 9447799330 Thiruvananthapuram. Fax : 0471-2512131 PIN - 695 033 e-mail: [email protected] website: www.niyamasabha.org DEPUTY SPEAKER SHRI V. SASI 2305831 3008 2512152 “Swathi”, (129-Chirayinkeezhu - SC) 9847311660 Legislature Complex, Room No. 626, Vikas Bhavan P.O., II Floor, Assembly Building. Thiruvananthapuram. Fax: 0471-2512596 PIN - 695 033 e-mail: [email protected] website: www.niyamasabha.org COUNCIL OF MINISTERS Phone Numbers Name, Constituency Residential Assembly Designation & Location Residence/ Address Direct Retiring Mobile Room SHRI PINARAYI VIJAYAN 2333241 2512040 2318406 Cliff House, (12-Dharmadam) 2314853 Nanthancode, Chief Minister 9447565656 Kowdiar P.O, Room No. 505, Thiruvananthapuram. I Floor, Assembly Building. PIN - 695 003 Fax: 0471-2333489 e-mail: [email protected] website: www.keralacm.gov.in SHRI A. K. BALAN 2333849 2512069 2310664 “Pamba”, (57-Tarur-SC) 2333772 9846361111 Cliff House Minister for Welfare of 9447962200 Compound, Scheduled Castes, Scheduled Nanthancode, Tribes, Backward Classes, Law, Kowdiar P.O., Culture and Parliamentary Affairs Thiruvananthapuram. Room No. 629, PIN -695 003 II Floor, Assembly Building. Fax: 0471-2332239 e-mail: [email protected] *EPABX numbers can be contacted from outside by prefixing 251. STD Code of all 7-digit numbers is 0471, if not specified otherwise. 1 Phone Numbers Name, Constituency Residential Designation & Location Assembly Residence/ Address Direct Retiring Mobile Room SHRI E. -

Ea=H ¼Jherh Fuezyk Lhrkje.K½ ¼Lora= Izhkkj½
GOVERNMENT OF INDIA MINISTRY OF COMMERCE & INDUSTRY (DEPARTMENT OF COMMERCE) LOK SABHA STARRED QUESTION NO. 205 TO BE ANSWERED ON 1st AUGUST, 2016 INDIA'S SHARE IN GLOBAL TRADE *205. SHRI JAYADEV GALLA: Will the Minister of COMMERCE & INDUSTRY (वािणय एव उयोग मं ंत्री ) be pleased to state: (a) the share of India's exports in the global trade at present; (b) whether the Government has taken steps to acquire a greater share in global trade including mapping of region-specific exports and if so, the details thereof; (c) the extent to which these steps are likely to help capture greater market share in global trade and achieve the export targets; and (d) whether special emphasis has been given to certain sectors including the food processing sector in this regard and if so, the details thereof? ANSWER okf.kT; ,oa m|ksx jkT; ea=h ¼Jherh fueZyk lhrkje.k½ ¼Lora= izHkkj½ THE MINISTER OF STATE IN THE MINISTRY OF COMMERCE AND INDUSTRY (INDEPENDENT CHARGE) (SMT. NIRMALA SITHARAMAN) a) to d): A Statement is laid on the Table of the House. ***** STATEMENT REFERRED TO IN REPLY TO PARTS (a) TO (d) OF LOK SABHA STARRED QUESTION NO. 205 FOR ANSWER ON 1st AUGUST, 2016 REGARDING “INDIA'S SHARE IN GLOBAL TRADE” (a) The share of India’s exports in global trade was 2.2% as in the year 2015, according to data published by WTO. Of this, the share of merchandise exports was 1.6% and share of commercial services was 3.3%. (b) Government has taken a number of steps to acquire greater share in global trade. -

Government of India Ministry of External Affairs Lok
GOVERNMENT OF INDIA MINISTRY OF EXTERNAL AFFAIRS LOK SABHA UNSTARRED QUESTION NO.2187 TO BE ANSWERED ON 04.03.2020 CORONAVIRUS INFECTED INDIANS 2187. ADV. DEAN KURIAKOSE: SHRI NAMA NAGESWARA RAO: SHRI KAPIL MORESHWAR PATIL: SHRI ACHYUTANANDA SAMANTA: SHRI KODIKUNNIL SURESH: SHRI ANTO ANTONY: PROF. SAUGATA RAY: SHRI P. RAVEENDRANATH KUMAR: Will the Minister of EXTERNAL AFFAIRS be pleased to state: (a) the number of corona virus infected Indian citizens residing abroad, country-wise; (b) the number of Indians rescued from the corona virus affected areas including the cost of the evacuation, country-wise; (c) the number of corona virus infected / disinfected Indians trapped in China and various parts of the world including the ones trapped abroad a cruise ship and the measures taken by the Government and Indian embassies/consulates to safely bring the aforesaid Indians back to India; (d) whether there are restrictions placed by several nations against people travelling back to India through transit from China and other nations where coronavirus proliferation has peaked; and (e) if so, the details thereof and the reasons therefor and the measures taken by the Government to address the issue? ANSWER THE MINISTER OF STATE IN THE MINISTRY OF EXTERNAL AFFAIRS [SHRI V. MURALEEDHARAN] (a) As per information available, the number of Coronavirus infected Indian citizens abroad is as follows: - Japan (on the cruise ship) – 16 (being treated at onshore medical facilities in Japan); and - UAE - 1 (b) Government of India evacuated a total of 766 persons, including 723 Indian nationals and 43 foreigners from China. Similarly, 119 Indians have been brought back to India from the cruise ship in Japan. -

Government of India Ministry of Finance Department of Revenue
Government of India Ministry of Finance Department of Revenue ***** LOK SABHA UNSTARRED QUESTION NO.28 TO BE ANSWERED ON MONDAY, SEPTEMBER 14, 2020 BHADRAPADA 23, 1942 (SAKA) GOLD SMUGGLING CASES 28. SHRI ANTO ANTONY: SHRI N.K. PREMACHANDRAN: ADV. DEAN KURIAKOSE: Will the Minister of Finance be pleased to state: (a) whether it has come to the notice of the Government/ Enforcement Directorate/ Customs that Gold smuggling through various airports in the country including Kerala airports is increasing and has adversely affected the economic stability of the country; (b) if so, the details of such cases of gold smuggling reported from various airports of the country including kerala airports during the last five years and the current year, year-wise along with the action taken by the Government in this regard; (c) the details of gold seized from various airports including kerala airports and the number of people booked during the said period along with the value/price involved therein; (d) whether it has also come to the notice of the Government that gold smuggling is carried out through the diplomatic channel and if so, the details of involvement of diplomatic persons therein along with the action taken in this regard; (e) whether the Government has entrusted agencies for the investigation of gold smuggling in Thiruvananthapuram air cargo through diplomatic channel and if so, the details thereof; and (f) whether the investigation agencies reported to the Court that the accused in the gold smuggling are highly influential and if so, the details thereof along with the initiatives taken by the Government for fair and proper investigation? ANSWER MINISTER OF STATE IN THE MINISTRY OF FINANCE (SHRI ANURAG SINGH THAKUR) (a) to (f): The year-wise number of cases of gold smuggling through various airports along with the quantum of gold seized, number of people booked and the value of gold seized can be seen from the following table: Year Number of Quantum of Number of Value of Cases of Gold Seized people Gold Smuggling (in Kg.) booked seized of Gold at (Rs. -

Accused Persons Arrested in Kottayam District from 26.07.2020To01.08.2020
Accused Persons arrested in Kottayam district from 26.07.2020to01.08.2020 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 CR 631/20 U/S RENJITH K KUNNAPPALLI HOUSE MUTTAMBALA 31.07.2020- 188,269,336IP Kottayam VISWANATH SI 1 DIJU SOMAN M-40 VADAVATHOOR BAIL FROM PS M .10.30 HRS C&4(2)€(j) east KOTTAYAM BHAGAM KOTTAYAM KEDO2020 EAST KAMALASADNAM CR 631/20 U/S RENJITH K RADHAKRISH HOUSE MUTTAMBALA 31.07.2020- 188,269,336IP Kottayam VISWANATH SI 2 SIJUPAL M-44 BAIL FROM PS NAN NEELAMPEROOR M .10.30 HRS C&4(2)€(j) east KOTTAYAM ALAPPUZHA KEDO2020 EAST CR 631/20 U/S RENJITH K PAYIPPATTU HOUSE MUTTAMBALA 31.07.2020- 188,269,336IP Kottayam VISWANATH SI 3 SANOJ RAVEENDRAN M-46 BAIL FROM PS KOLLAD KOTTAYM M .10.30 HRS C&4(2)€(j) east KOTTAYAM KEDO2020 EAST CR 631/20 U/S RENJITH K MALIAKKELHOUSE MUTTAMBALA 31.07.2020- 188,269,336IP Kottayam VISWANATH SI 4 SANU SUKUMARAN M-41 PERINGARA VILAGE BAIL FROM PS M .10.30 HRS C&4(2)€(j) east KOTTAYAM PATHANAMTHITTA KEDO2020 EAST RENJITH K PERUMKAVUMKAL CR 616/20 U/S MUKESHKUM SUB JAIL 30..07.2020- Kottayam VISWANATH SI JFMC 1 5 KUTTAPPAN M-38 HOUSE KANGAZHA 457,361,380 AR PONKUNNAM 13.00 HRS east KOTTAYAM KOTTAYAM KOTTAYAM IPC EAST THEVERVADAKETHIL 491/2020 JUSTIN S HOUSE, 27/7/2020- MANDAPOM , 6 SARATH SASI 22/M AMAYANNOOR 118(A) OF KP AYARKUNNAM BAIL FROM PS VARAKUMALA 23.45 GSI OF ACT AMAYANNOOR POLICE VADAKKEKATTIL HOUSE, 490/2020 U/S VIKAS 28-07-2020- ANILKUMAR 7 PRAKASH 36/M AMAYANNOOR KARA AYARKUNNAM 279, 337,338 AYARKUNNAM MK GSI OF BAIL FROM PS PRAKASH 12 -30 AYARKUNNAM IPC POLICE VILLAGE MAMBRAYIL HOUSE, 490/2020 U/S AMAYANNOR KARA, 28-07-2020- ANILKUMAR 8 REJIN JOSE DAVIDSON 29/M AYARKUNNAM 279, 337,338 AYARKUNNAM MK GSI OF BAIL FROM PS AYARKUNNAM 12 -30 IPC POLICE VILLAGE KANJIRATHINKEL JUSTIN S HOUSE, 30.7.2020-- 492/2020, U/S MANDAPOM , 9 VINEETH KS SHAJI KK 26/M AMAYANNOOR. -

New Necrology.Pmd
BR. ARMOND MADHAVATH JANUARY-12 Br. Armond born on November 25, 1930 at Palackattumala in Kottayam district (later settled at Nadavayal, Manathavady diocese) made his profession in the Order on May 13, 1957 and was ordained priest on March 25, 1960. He died on January 12, 2001 and his mortal remains were laid to rest at Vimalagiri Ashram, Iritty. Br. Armond started his life as a community member in Nazareth Ashram Aluva. Later he served as director of Third Order Franciscans at Loreto Ashram Muvattupuzha and then as Rector of the Seraphic Seminary at Bharananganam where he later became the director of the charismatic retreats for a quarter of a century. It was Br. Armond who started in Kerala the first Malayalam Charismatic Retreat at Bharananganam with official ecclesiastical approval. Several years later he sought permission to go to Iritty to continue the same ministry. Though Br. Armond spent the rest of his life in organizing charismatic retreats, himself started preaching quite late until he received the special grace for it from the Holy Spirit. He was known to be a man of prayer. All through his life he kept up extra hours of personal prayer both very early in the morning and late in the night. His profound devotion to the most Blessed Trinity inspired him to write several articles on Trinitarian spirituality and conduct special retreats of Trinitarian experience. Because of his deep spirituality he could calmly face oppositions and hurdles with confidence in God’s power. He lived a life fully resigned to God. In this respect his life at Aluva, Muvattupuzha, Bharananganam and Iritty provides shining example for us. -

Committee on Government Vernment Vernment Assurances Assurances
COMMITTEE ON GOVERNMENT ASSURANCES 62 (2016-2017) SIXTEENTH LOK SABHA S IXTY-SECOND REPORT REQUESTS FOR DROPPING OF ASSURANCES (NOT ACCEDED TO) (Presented to Lok Sabha on 1 August, 2017) LOK SABHA SECRETARIAT NEW DELHI July, 2017/Shravana, 1939 (Saka) SIXTY-SECOND REPORT COMMITTEE ON GOVERNMENT ASSURANCES (2016-2017) (SIXTEENTH LOK SABHA) REQUESTS FOR DROPPING OF ASSURANCES (NOT ACCEDED TO) (Presented to Lok Sabha on 1 August, 2017) LOK SABHA SECRETARIAT NEW DELHI July, 2017/Shravana, 1939 (Saka) CGA No. 312 Price: ` 122.00 © 2017 BY LOK SABHA SECRETARIAT Published under Rule 382 of the Rules of Procedure and Conduct of Business in Lok Sabha (Fifteenth Edition) and Printed by the General Manager, Government of India Press, Minto Road, New Delhi-110 002. CONTENTS PAGE COMPOSITION OF THE COMMITTEE (2016-2017) ............................................ (iii) INTRODUCTION ........................................................................................... (v) REPORT ..................................................................................................... 1 REQUESTS FOR DROPPING OF ASSURANCES (NOT ACCEDED TO) APPENDICES-I TO XIX I. USQ No. 27 dated 22.02.2011 regarding ‘Grievances of Prasar Bharati Employees’........................................... 4 II. USQ No. 2318 dated 14.12.2015 regarding ‘Shramev Jayate Karyakram’ .................................................................. 7 III. SQ No. 521 dated 30.04.2015 (Supplementary by Shri N.K. Premachandran, M.P.) regarding ‘Pendency in Courts)’ .................................................................. -
Lok Sabha 16Th September 2020
Lok Sabha (List of Questions for WRITTEN ANSWERS Wednesday, September 16, 2020/Bhadrapada 25, 1942 (Saka)) 16th September 2020 ---- [Prime Minister - ATOMIC ENERGY - COAL - COMMERCE AND INDUSTRY - COMMUNICATIONS - DEFENCE - DEVELOPMENT OF NORTH EASTERN REGION - ELECTRONICS AND INFORMATION TECHNOLOGY - EXTERNAL AFFAIRS - LAW & JUSTICE - MINES - PARLIAMENTARY AFFAIRS - PERSONNEL,PUBLIC GRIEVANCES AND PENSIONS - RAILWAYS - SPACE - STATISTICS AND PROGRAMME IMPLEMENTATION and PLANNING ]. 15 ---- Impact of COVID-19 on GDP 461 Shri. Rajiv Ranjan Singh (Lalan)(Munger) : Sh. A.K.P. Chinraj (Namakkal ) : STATISTICS AND PROGRAMME IMPLEMENTATION:- (a) whether the Government has assessed the impact of monetisation and COVID-19 on GDP growth; (b) if so, the details thereof; (c) the measures taken by the Government to tackle the decline in GDP growth in the present economic slowdown; and (d) the details of major factors that affected GDP during the last one year? , ---- 1 GDP Growth Rate 462 Shri. Rajiv Ranjan Singh (Lalan)(Munger) : Dr. Kalanidhi Veeraswamy ( Chennai North ) : STATISTICS AND PROGRAMME IMPLEMENTATION:- (a) whether it is a fact that the economists have been calling for large stimulus packages amounting to double-digit percentages of Gross Domestic Product (GDP), despite the strain on the exchequer; (b) if so, whether GDP has shrunk by 23.9 percent in the first quarter of the financial year 2020-21 against 5.2 percent growth in Q1 2019-20 and has dipped by (minus) 27.11 percent in August 2020; and (c) the details of constructive action plan that has been taken for improving the GDP growth rate? , ---- Development of Online Games 463 Sh. Faizal P.P. Mohammed (Lakshadweep): ELECTRONICS AND INFORMATION TECHNOLOGY:- (a) whether the Government is providing any support to indigenously developed online gaming; (b) if so, the details thereof; and (c) whether the indigenous development of online game will generate employment opportunities in the country and if so, the details thereof? ---- GDP Decline , 464 Sh.