Chemically Activated Cooling Vest's Effect on Cooling Rate Following
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alex Sawyer, Bank of America Chicago Marathon, 1.312
September 10, 2015 Reporters May Contact: Alex Sawyer, Bank of America Chicago Marathon, 1.312.992.6618 [email protected] Diane Wagner, Bank of America, 1.312.992.2370 [email protected] 2012 Chicago Champion and Current Half Marathon World Record-holder Headline 2015 Bank of America Chicago Marathon Elite Field International Elites Attempt to Qualify for National Olympic Teams CHICAGO – Today, the Bank of America Chicago Marathon announced 2012 champion Tsegaye Kebede of Ethiopia and current half marathon world record-holder Florence Kiplagat of Kenya will return to compete for the crown at the 38th annual event. Kebede and Kiplagat accent an international elite field that represents the global road to Rio de Janeiro. Many athletes hope to use the 2015 Chicago Marathon as a springboard (via qualifying times and notable performances) to representing their countries at the Rio de Janeiro 2016 Olympic Games. Chicago marks the site of Kebede’s 2012 marathon personal best (2:04:38) and his sole victory in three attempts down the homestretch on Columbus Drive. His 2010 epic, head-to-head battle against the late Sammy Wanjiru is considered by many to be one of the most courageous marathon duels of all time. On the women’s side, Kenya’s Florence Kiplagat comes back to Chicago after finishing in 2:25:57 last year. Kiplagat has something no other woman in the field has: the half marathon world record. The 2010 IAAF World Half Marathon champion and the 2011 and 2013 Berlin Marathon champion broke her own half marathon world record in February, clocking a remarkable 1:05:09 in Barcelona (she also set the 15K and 20K world records en route). -

Sporting Events 2015 Date Sport Event Venue 26 Dec 2014 – 5 Jan Ice Hockey 2015 World Junior Ice Hockey Championships Air Canada Centre, Toronto Bell Centre, Montreal
Sheet2 Sporting Events 2015 Date Sport Event Venue 26 Dec 2014 – 5 Jan Ice hockey 2015 World Junior Ice Hockey Championships Air Canada Centre, Toronto Bell Centre, Montreal 4 Jan – 10 Jan Ice hockey 2015 IIHF World Women's U18 Championship – Division I Vaujany, France 4 Jan – 10 Jan Tennis 2015 Hopman Cup Perth, Australia 4 Jan – 17 Jan Rallying 2015 Dakar Rally Buenos Aires, Argentina 5 Jan – 12 Jan Ice hockey 2015 IIHF World Women's U18 Championship Buffalo, United States 10 Jan Formula E 2015 Buenos Aires ePrix Argentine 15 Jan – 25 Jan Snowboarding FIS Snowboarding World Championships 2015 Kreischberg, Austria 15 Jan –25 Jan Freestyle skiing FIS Freestyle World Ski Championships 2015 Kreischberg, Austria 15 Jan – 1 Feb Handball 2015 World Men's Handball Championship Qatar 16 Jan – 17 Jan Luge 2015 FIL Junior World Luge Championships Lillehammer, Norway 19 Jan – 25 Jan Ice hockey 2015 World Junior Ice Hockey Championships – Division III Dunedin, New Zealand 19 Jan – 25 Jan Ice hockey 2015 IIHF World Women's U18 Championship – Division I Qualification Katowice, Poland 19 Jan –1 Feb Tennis 2015 Australian Open Melbourne Park in Melbourne, Australia 22 Jan – 1 Feb Nordic skiing 2015 IPC Biathlon and Cross-Country Skiing World Championships Cable, Wisconsin United states 24 Jan – 1 Feb Multi-sport 2015 Winter Universiade (co-host with Spain) Granada, Spain 25 Jan – 15 Nov Rallying 2015 World Rally Championship season Europe, North and South America and Australia 31 Jan – 1 Feb Cyclo-cross 2015 UCI Cyclo-cross World Championships Tabor -

Pauline Tse Brief Profile
Name : Pauline Tse Brief Profile - A previously sedentary woman who found her potential in sports in 2004 and now a committed athlete with strong interest in distance running, trail running, triathlon and adventure racing. - Mentored by Dr Dennis Whitby, who was the Director of HK Sports Institute in the 90s, and assisted him in coaching his athletes at SportPlus Ltd. for 4 years. - Obtained MSc in Exercise Science at Chinese University of Hong Kong in 2011. - Frequent award winners at local races including the Standard Chartered HK Marathon. - Founded the HKU Marathon Team in 2006 with over 3000 current members. - Now a running coach training individual athletes as well as for corporate run team. - Personal running goal for 2016 : to complete the Six World Major Marathons by first quarter, 2016 Awards in past few years : 2014 14th HKAAA female athlete in Standard Chartered Full Marathon 2012 HKU 37K Round The Island Female Champion 2012 Hong Kong ITU Triathlon (Olymipic Distance) – Age Group 1st Runner-up 2011 Standard Chartered HK Marathon 10K Age Group Champion (HK resident) 2010 Adidas 5K Series – 1st runner-up 2010 King of the City – 1st runner-up 2-person Relay 2010 Kam Sheung Road Duathlon Race – Age Group Champion 2010 Folding Bike Urban Chase – 1st runner-up 2010 China Coast Marathon – 1st runner-up 2009 30K Pre-marathon – 4th runner-up 2009 Unicef Half Marathon – 5th runner-up 2009 Hong Kong ITU Triathlon – 2nd runner-up Olympic Distance 2009 Sprint Triathlon Championship – Age Group Champion 2009 Round the Island Time Trial -

Sporting Events 2015
Sheet1 Sporting Events 2015 Date Sport Event Venue 4 June – 7 June 3x3 (basketball) 2015 FIBA 3x3 U18 World Championships Hungary 2 Feb – 15 Feb Alpine skiing FIS Alpine World Ski Championships 2015 United States, at Vail / Beaver Creek, Colorado 1 Mar –10 Mar Alpine skiing 2015 IPC Alpine Skiing World Championships Canada 14 May – 24 May Amateur boxing 2015 Women's Junior/Youth World Boxing Championships Taipei, Taiwan 2 Sep – 13 Sep Amateur boxing 2015 Junior World Boxing Championships St Petersburg, Russia 5 Oct – 18 Oct Amateur boxing 2015 World Amateur Boxing Championships Doha, Qatar 4 July – 18 July American football 2015 IFAF World Championship Panama 24 July – 9 August Aquatics 2015 World Aquatics Championships Kazan, Russia 8 June – 14 June Archery 2015 World Archery Youth Championships Yankton, USA 26 July – 2 August Archery 2015 World Archery Championships Copenhagen, Denmark 13 Sep – 25 Sep Archery 2016 Summer Olympics Test Events Rio de Janeiro, Brazil 24 Oct – 2 Nov Artistic gymnastics 2015 World Artistic Gymnastics Championships Glasgow, Scotland 30 May – 20 June Association football 2015 FIFA U-20 World Cup New Zealand 6 June – 5 July Association football 2015 FIFA Women's World Cup Canada 13 June – 29 June Association football 2015 CPISRA Football 7-a-side World Championships St Georges Park, UK 17 Oct– 8 Nov Association football 2015 FIFA U-17 World Cup Chile 28 Mar Athletics 2015 IAAF World Cross Country Championships Guiyang, China 15 May Athletics Qatar Athletic Super Grand Prix Doha, Qatar 17 May Athletics Shanghai Golden Grand Prix Shanghai, PR China 30 May Athletics Prefontaine Classic Eugene, Oregon, U.S. -

Athletics Monthly
` November 2014 Athletics Monthly The Journal of the World Famous Scarborough Athletic Club Club members at the start of the Drewton Woods cross country, present a 75th birthday shirt to the editor A full Press Report is included in this edition In this edition; Fixtures Lists. Road, Multi Terrain,Fell Road Rankings Athletics Biographies. Club Chairman Harry Forkin Pro Am Newsletter. Stretching and Back Pain. Jenna Wheatman. BSc. MSST Easy day running. Runners World USA article Cartoon of the Month Quote of the Month. Re cross country by John Treacey,a two times World Champion Press Reports From the Editor Welcome to the November edition, which is slightly later this month. Thank you to Harry Forkin and Jenna Wheatman for their contributions. I recommend reading Jenna’s views on stretching. As I write, the cross country season is well underway and we have had some good individual results in both the East Yorkshire and North Yorkshire Leagues. Whilst our attendances at the East Yorkshire League have increased, we need some good team scores in the remaining four fixtures, starting with our home fixture at Langdale End on Sunday 14 December. In the more traditional NYSD, we have as yet, only one team score, that of the our Senior Women’s team at Filey, but we have had some promising results from several new members, and have provided some senior men and women at all three fixtures so far. I have added the New Year cross country dates to the fixtures list, and next month will publish as many 2015 road race dates as I can establish Mick Thompson 01723 864442 [email protected] Fixtures Club members have participated in almost all of the races listed. -
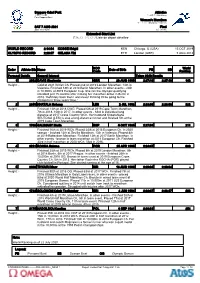
Extended Start List 拡張スタートリスト / Liste De Départ Détaillée
Sapporo Odori Park Athletics 札幌大通公園 陸上競技 / Athlétisme Parc Sapporo Odori Women's Marathon 女子マラソン / Marathon - femmes SAT 7 AUG 2021 Final Start Time 06:00 決勝 / Finale Extended Start List 拡張スタートリスト / Liste de départ détaillée WORLD RECORD 2:14:04 KOSGEI Brigid KEN Chicago, IL (USA) 13 OCT 2019 OLYMPIC RECORD 2:23:07 GELANA Tiki ETH London (GBR) 5 AUG 2012 NOC World Order Athlete Bib Name Code Date of Birth PB SB Ranking Personal Details General Interest Tokyo 2020 Results 1 2002 DAVIS Stephanie GBR 26 AUG 1990 2:27:16 2:27:16 192 Height: - Gold at 2021 British Ch. Placed 2nd at 2019 London Marathon, 14th in Valencia. Finished 18th at 2018 Berlin Marathon. In other events - 24th in 10,000m at 2019 European Cup. She ran the Olympic qualifying standard just 15 months after making her marathon debut in Berlin in 2018. 'Definitely back then I was never thinking I'll be going to the Olympics in three years' time.' 2 2859 KHATALA Neheng LES 2 JUL 1992 2:28:06 2:28:06 322 Height: - Finished 13th at 2018 CWG. Placed 6th at 2019 Cape Town Marathon, 7th in 2018, 10th in 2017. In other events - 83rd in individual long distance at 2017 Cross Country WCh. Her husband Khoarahlane SEUTOALI (LES) is also a long-distance runner and finished 5th at the 2019 Cape Town Marathon. 3 1766 GALIMANY Marta ESP 5 OCT 1985 2:27:08 211 Height: - Finished 16th at 2019 WCh. Placed 24th at 2018 European Ch. In 2020 season - finished 12th at Sevilla Marathon, 13th in Valencia. -

A Gendered Analysis of the Men's and Women's World
A GENDERED ANALYSIS OF THE MEN’S AND WOMEN’S WORLD CUP COMMENTARY: THE CONTINUATION OF MEN’S DOMINANCE IN THE FOOTBALLING WORLD Bethan Cate Sullivan A thesis submitted in partial fulfilment of the requirements of the University of Lincoln for the degree of MSc by Research for the School of Sport & Exercise Science, College of Social Science March 2019 Abstract This study focused on the Men’s and Women’s World Cup looking into how gender is constructed within the commentary from the 2014 & 2015 tournaments. Football was used because football had been examined in a number of different ways, such as participation rates or newspaper coverage, but commentary hadn’t been analysed in this way before. Using a combination of commentary and match reports, the narratives of the commentary was analysed to find out if there were any stylistic techniques that differed between the two sets of commentary. These tournaments were used because of their proximity to each other and only at the group stages to keep as much continuity between the two sets of commentary as possible. A Foucauldian Discourse analysis was used to examine the World Cup match commentary because of its focus on the ideological content of language. This study found that there were notable differences in the narratives between the men’s and women’s matches. The results showed that the historical impact of the men’s game related to it being the nation’s favourite sport. Men also build the image of a nation in relation to football as a symbol of England, with women taking a secondary place in football. -

2 16 CM Elite Athletes.Indd
Elite athletes Elite athlete roster.................................................................................................................................................................................. 30 Men’s biographies ................................................................................................................................................................................... 32 Women’s biographies ............................................................................................................................................................................ 74 Men’s wheelchair biographies ......................................................................................................................................................... 105 Women’s wheelchair biographies .................................................................................................................................................. 123 Elite athletes Bank of America Chicago Marathon 29 Sunday, October 9, 2016 2016 Bank of America Chicago Marathon elite field First name Last name Country Marathon PR Men Julia .....................................Roman-Duval .................USA..................................... 2:40:55 First name Last name Country Marathon PR Rachel ................................Hyland ................................USA..................................... 2:41:26 Dennis ...............................Kimetto .............................KEN ..................................... 2:02:57 -

Foundation Focus Has Been the Coming Months
IssueBusiness 1 - June 2015 Name Business Name What’s On? Event Calendar 2015 Foundation June 4th Berkeley Foundation Street Elite Festival—Westway 11th Berkeley Homes Southern Go Kart Endurance Race 11th Berkeley Capital Dragon Boat Race Focus Issue 1 - June 2015 11th Berkeley Foundation Street Elite Festival—Tower Hamlets 12th Berkeley Homes East Thames Demelza 101 Ben Nevis Trek 12th St James Three Peaks Challenge 12th Berkeley Homes Western Charity Abseil 18th Berkeley Foundation Street Elite Festival—Wandsworth Inside this issue: Welcome to the first edition! July Welcome 1 2nd Berkeley Foundation Street Elite Festival—Ealing 5th Berkeley Homes West London Strong Man Weightlifting Competition Our Rep in….. 1 9th Berkeley Foundation Street Elite Festival—Southwark In the recent staff survey you We plan to have regular sec- 24th St Edward Three Peaks Challenge said you wanted to know more tions including a feature Char- about what the Berkeley Foun- ity, spotlight on a Foundation London Marathon 2 August dation does and how we allo- Rep, key events that have cate the money that you gener- 2nd Berkeley Foundation Prudential Ride London 100 taken place and a list of Prudential Ride London 2 28th Berkeley Homes South East London 300 Mile Cycle ously raise through staff events events that have been regis- and GAYE. tered with the Foundation for September North London Hospice 3 Foundation Focus has been the coming months. 8th Berkeley Homes Western Charity Golf Day and Longridge launched to keep Berkeley staff 12th Berkeley Homes Oxford and Chiltern Three Peaks Challenge We also want to hear from in touch with Foundation activi- 12th Berkeley Homes North East London Woodberrystock Music Festival you, so tell us what you want What’s On 4 17th St Edward Clay Pigeon Shooting ties and to introduce you to the to see and we will do our best Charities, programmes and to include it in future editions. -
The Academy Spring 2016
Official Publication of the United States Sports Academy Alumni Association Vol. 38, No. 1 Spring 2016 Academy Founding President Dr. Thomas P. Rosandich Steps Down after 43 Years Dr. Thomas P. Rosandich, the founding in 1972, the Academy has conferred almost President and Chief Executive Officer (CEO) of 5,000 sport-specific degrees to its students. The the Academy, stepped down from his position at Academy has also touched the lives of count- the helm of the institution that he founded and less thousands of others working in the sport served since 1972. In their Annual Meeting held profession through its certification and diploma on Friday, 6 November 2015, the Academy’s programs that are largely delivered abroad. The Board of Trustees accepted the resignation of Academy remains the only free-standing region- Rosandich and concurrently voted to name him ally accredited sports university in the country. as President Emeritus. In the role of President Rosandich has had a long and storied career Emeritus, Rosandich will remain engaged with in the profession of sport dating to the early the institution focusing on fundraising, alumni Dr. Thomas P. Rosandich 1950s. During this time, he embarked upon a affairs, the Academy’s Award of Sport program career as a coach in football and track and field, and international relations. in four disciplines in 2004. The Academy cur- an avocation that eventually had him named to In the same meeting, the Trustees voted Dr. rently enrolls approximately 900 students at all the Helms Track and Field Hall of Fame. As a Thomas J. -
MALE ELITE ATHLETES HAMBURG MARATHON 2018 1. Emmanuel
MALE ELITE ATHLETES HAMBURG MARATHON 2018 1. Emmanuel Mutai KEN/1984 2:03:13 2. Sammy Kitwara KEN/1986 2:04:28 3. Stephen Kiprotich UGA/1989 2:06:33 4. Ayele Abshero ETH/1990 2:04:23 5. Vincent Kipruto KEN/1987 2:05:13 6. Stephen Chebogut KEN/1985 2:05:52 7. Solomon Deksisa ETH/1994 2:06:22 8. Shumi Dechasa BRN/1989 2:06:43 9. Solomon Yego KEN/1987 2:07:12 10. Fikre Assefa ETH/1989 2:08:36 11. Estefanos Tewelde ERI/1981 2:09:16 12. Aychew Bantie ETH/1995 2:09:40 14. Tadu Abate ETH/1997 debut 15. Abdelhadi El Hachimi BEL/1974 2:10:35 16. Philipp Pflieger GER/1987 2:12:50 17. Ivan Gálan Bardera ESP/1979 2:13:58 18. Solomon Tesfamariam SUI/1972 2:14:51 19. Gilmar Silvestre Lopes BRA/1989 2:16:06 20. Jesper Faurschou DEN/1983 2:16:15 FEMALE ELITE ATHLETES HAMBURG MARATHON 2018 F1 Isabellah Andersson SWE/1980 2:23:41 NR F2 Shitaye Eshete BRN/1990 2:25:36 F3 Sylvia Kibet KEN/1984 2:26:16 F4 Beata Naigambo NAM/1980 2:26:57 F5 Filomena Costa POR/1985 2:28:00 F6 Birke Debele ETH/1995 2:29:45 F7 Kuftu Tahir ETH/1995 2:31:27 F8 Tejitu Daba BRN/1991 2:31:32 F9 Mimi Belete BRN/1988 debut F10 Paula Todoran ROM/1985 2:36:44 1 Emmanuel Mutai KEN/1984 2:03:13 Adidas Emmanuel Mutai is a full cousin to Richard Limo, the 2001 World Champion 5.000m. -

Runners Are Beautiful
PRESS GUIDE ALL RUNNERS ARE BEAUTIFUL MATTONI KARLOVY VARY HALF MARATHON 19 MAY 2018 ENG MATTONI KARLOVY VARY HALF MARATHON MEDIA INFORMATION Dear Sports Friends, Welcome to the 6th edition of the Mattoni Karlovy Vary Half Marathon! The Press Guide, which you are holding in your hands, contains basic information for journalists about the Mattoni Karlovy Vary Half Marathon. You will also find a short introduction of elite athletes including intermediate times leading to breaking records. We hope you find everything you need to cover this year’s event, but please do not hesitate to ask anyone on the Press Team, if you need anything else. THE PRESS TEAM The Press Team is based at the Spa Hotel Thermal. Tadeáš Mahel PR & Media 725 974 749 [email protected] Milan Janoušek PR & Media 776 712 665 [email protected] Diana Rybachenko International Media and Guests 777 746 801 [email protected] James Moberly International Media 737 186 997 [email protected] PRESS CENTER The Press Center is a place where media representatives can pick up their credentials. Also, they will find there the latest information about the race, wireless Internet access, live results and live race broadcasting. Friday – Saturday (race day) Red lounge 2 Spa Hotel Thermal, 1st floor I. P. Pavlova 11 Karlovy Vary Opening hours: Friday May 18th 11:00 a.m. – 8:30 p.m. Spa Hotel Thermal, Red lounge 2 Saturday May 19th 8:30 a.m. – 11:00 p.m. Spa Hotel Thermal, Red lounge 2 2 PRESS GUIDE MEDIA CAR Take advantage of an opportunity to ride in a special car which will drive ahead of the elite runners throughout the race! • Unique experience • Unrivaled photographs • Live coverage from the course Reserve space in the car at the Press Centre or by calling Tadeáš Mahel at tel: +420 725 974 749.