MIGRATION of MEDICAL DOCTORS from KERALA Acknowledgements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Operation Theatre Technician Anurag
OPERATION THEATRE TECHNICIAN ANURAG. A. S ADARSH. A. S ANU BHAVAN VIDYA VIHAR, VEERALAM VALIYAPARAMBU ATTINGAL PO MARAYAMUTTOM PO TRIVANDRUM 695101 TRIVANDRUM 695124 Roll No. 1001 Roll No. 1008 AJULAL. T ANURAJ. S. R LINUBHAVANAM, THAZHAM VARUVILA PUTHEN VEEDU EAST KALLADA PO, MAMKOOTTAM THIRUPURAM PO KOLLAM, 691502 TRIVANDRUM 695133 Roll No. 1002 Roll No. 1009 AMAL NATH. R. M ANUSREE. A SARALAMANDIRAM SREELAKAM MADATHUVATHUKKAL KAROOR, POTHENCODE PO MITHIRMALA PO‐ 695610 TRIVANDRUM 695584 Roll No. 1003 Roll No. 1010 ANILA. P. V ARCHANA. S PUTHIYA VEETTIL ARCHANA BHAVAN POOKODE PO PULLOORKONAM, VIZHINJAM PO KANNUR 670691 TRIVANDRUM. 695521 Roll No. 1004 Roll No. 1011 ANTO VINCENT. T ARCHANA. S ANTO NIVAS SREEPADMAM, LMSRA‐65 VIRALY, UCHAKKADA PO L. M. S. JUNCTION, ATTINGAL NEYYATTINKARA TRIVANDRUM, 695101 TRIVANDRUM,695506 Roll No. 1012 Roll No. 1005 ARUN. G. J ANUJA. S. S AMBADI, VAMANAPURAM ADITHYA BHAVAN VAMANAPURAM PO KATTACHAL KUZHI PO TRIVANDRUM, 695606 BALARAMAPURAM Roll No. 1013 TRIVANDRUM 695501 Roll No. 1006 ASWANI. R LAKSHMIGOVINDAM' ANURADHA. S. P KAYAKKAL HOUSE, PAYAMBRA POST SAFALYA KUNNAMANGALAM (VIA) PUTHENVEEDU KOZHIKODE 673571 PALLIPPURAM PO Roll No. 1014 TRIVANDRUM 695316 Roll No. 1007 ASWATHI. S ILANGO. K KRISHNA VILASOM NO. 18, K. K. ILLAM KADATHOOR, K. S. PURAM PO KALIAMMAN KOVIL STREET KARUNAGAPPALLY KEEZHAKASAKUDY, KOTTUCHERRY KOLLAM 690544 KARAIKAL 609609 Roll No. 1015 Roll No. 1023 BABU. T. N JEENA. J. V NO. 20, CONTRACTOR SUBRAMANI FIRST STREET THEKKEYIDA VILAKATHU THORAPADI, VELLORE MELE PUTHEN VEEDU TAMIL NADU, 632002 AMOTTUKONAM, CHAIKOTTUKONAM PO Roll No. 1016 TRIVANDRUM 695122 Roll No. 1024 BIFIN. B ARUMALOORKONAM JINI. M. G MEKKE PLANKALA VEEDU SOUPARNIKA KUNNATHUKAL, KARAKONAM PO MAMPALLIKUNNAM TRIVANDRUM 695504 CHATHANNUR PO Roll No. -
Pathanamthitta
Census of India 2011 KERALA PART XII-A SERIES-33 DISTRICT CENSUS HANDBOOK PATHANAMTHITTA VILLAGE AND TOWN DIRECTORY DIRECTORATE OF CENSUS OPERATIONS KERALA 2 CENSUS OF INDIA 2011 KERALA SERIES-33 PART XII-A DISTRICT CENSUS HANDBOOK Village and Town Directory PATHANAMTHITTA Directorate of Census Operations, Kerala 3 MOTIF Sabarimala Sree Dharma Sastha Temple A well known pilgrim centre of Kerala, Sabarimala lies in this district at a distance of 191 km. from Thiruvananthapuram and 210 km. away from Cochin. The holy shrine dedicated to Lord Ayyappa is situated 914 metres above sea level amidst dense forests in the rugged terrains of the Western Ghats. Lord Ayyappa is looked upon as the guardian of mountains and there are several shrines dedicated to him all along the Western Ghats. The festivals here are the Mandala Pooja, Makara Vilakku (December/January) and Vishu Kani (April). The temple is also open for pooja on the first 5 days of every Malayalam month. The vehicles go only up to Pampa and the temple, which is situated 5 km away from Pampa, can be reached only by trekking. During the festival period there are frequent buses to this place from Kochi, Thiruvananthapuram and Kottayam. 4 CONTENTS Pages 1. Foreword 7 2. Preface 9 3. Acknowledgements 11 4. History and scope of the District Census Handbook 13 5. Brief history of the district 15 6. Analytical Note 17 Village and Town Directory 105 Brief Note on Village and Town Directory 7. Section I - Village Directory (a) List of Villages merged in towns and outgrowths at 2011 Census (b) -

Payment Locations - Muthoot
Payment Locations - Muthoot District Region Br.Code Branch Name Branch Address Branch Town Name Postel Code Branch Contact Number Royale Arcade Building, Kochalummoodu, ALLEPPEY KOZHENCHERY 4365 Kochalummoodu Mavelikkara 690570 +91-479-2358277 Kallimel P.O, Mavelikkara, Alappuzha District S. Devi building, kizhakkenada, puliyoor p.o, ALLEPPEY THIRUVALLA 4180 PULIYOOR chenganur, alappuzha dist, pin – 689510, CHENGANUR 689510 0479-2464433 kerala Kizhakkethalekal Building, Opp.Malankkara CHENGANNUR - ALLEPPEY THIRUVALLA 3777 Catholic Church, Mc Road,Chengannur, CHENGANNUR - HOSPITAL ROAD 689121 0479-2457077 HOSPITAL ROAD Alleppey Dist, Pin Code - 689121 Muthoot Finance Ltd, Akeril Puthenparambil ALLEPPEY THIRUVALLA 2672 MELPADAM MELPADAM 689627 479-2318545 Building ;Melpadam;Pincode- 689627 Kochumadam Building,Near Ksrtc Bus Stand, ALLEPPEY THIRUVALLA 2219 MAVELIKARA KSRTC MAVELIKARA KSRTC 689101 0469-2342656 Mavelikara-6890101 Thattarethu Buldg,Karakkad P.O,Chengannur, ALLEPPEY THIRUVALLA 1837 KARAKKAD KARAKKAD 689504 0479-2422687 Pin-689504 Kalluvilayil Bulg, Ennakkad P.O Alleppy,Pin- ALLEPPEY THIRUVALLA 1481 ENNAKKAD ENNAKKAD 689624 0479-2466886 689624 Himagiri Complex,Kallumala,Thekke Junction, ALLEPPEY THIRUVALLA 1228 KALLUMALA KALLUMALA 690101 0479-2344449 Mavelikkara-690101 CHERUKOLE Anugraha Complex, Near Subhananda ALLEPPEY THIRUVALLA 846 CHERUKOLE MAVELIKARA 690104 04793295897 MAVELIKARA Ashramam, Cherukole,Mavelikara, 690104 Oondamparampil O V Chacko Memorial ALLEPPEY THIRUVALLA 668 THIRUVANVANDOOR THIRUVANVANDOOR 689109 0479-2429349 -

NATIONAL MEANS CUM MERIT SCHOLARSHIP EXAMINATION (NMMSE)-2019 (FINAL LIST of ELIGIBLE CANDIDATES) THIRUVANANTHAPURAM DISTRICT GENERAL CATEGORY Sl
NATIONAL MEANS CUM MERIT SCHOLARSHIP EXAMINATION (NMMSE)-2019 (FINAL LIST OF ELIGIBLE CANDIDATES) THIRUVANANTHAPURAM DISTRICT GENERAL CATEGORY Sl. Caste ROLL NO Applicant Name School_Name No Category 1 42192790174 SREEHARI VINOD General Govt. Model HSS For Boys Attingal , Attingal 2 42192830290 GOPIKA I G General Govt. V.H.S.S. Kallara , KALLARA 3 42192730328 ARATHY M General GOVT. H S S, NEDUVELI, KONCHIRA, VEMBAYAM , 4 42192750125 ANAND SWAROOP J S General Govt. H S S Elampa , Elampa 5 42192740003 AMAL A L General L. V. H. S. Pothencode , Pothencode 6 42192860293 DEVANARAYANAN S R General P. P. M. H. S. Karakonam , karakonam 7 42192810350 KRIPA SUDISH General R R V GHSS Kilimanoor , kilimanoor 8 42192830280 ASNA S General Govt. V.H.S.S. Kallara , KALLARA 9 42192870029 AKHILA S General St. Thomas H. S. S. Amboori , Amboori 10 42192830299 MIDHUNA S NAIR General Govt. V.H.S.S. Kallara , KALLARA 11 42192740032 RESHMA S R General St. Goretti's Girls H. S. S. Nalanchira , Nalanchira 12 42192760120 ASHTAMI A S General DBHS Vamanapuram , vamanapuram 13 42192790241 GANGA G PRASANNAN General Govt H S S For Girls Attingal , Attingal 14 42192790227 ATHIDI ANILKUMAR General Govt H S S For Girls Attingal , Attingal 15 42192810135 DEVIKA B General Govt. HSS Kilimanoor , kilimanoor 16 42192820005 ADWAITH S R General Govt V H S S Njekkad , NJEKKAD 17 42192830371 RISHAV RAJ General M R M K M M H S S Edava , EDAVA 18 42192850125 SHANU S General St. Mary`s H. S. S. Vizhinjam , Vizhinjam 19 42192840321 JAYASREE J S General New H. S. -

Internet Usage Patterns Among Medical Interns of Muzaffarnagar: a Comprehensive Survey Analysis
ORIGINAL ARTICLE ASIAN JOURNAL OF MEDICAL SCIENCES Internet usage patterns among medical interns of Muzaffarnagar: A comprehensive survey analysis Sanjeev Davey1, Santosh Kumar Raghav1, Anuradha Davey2, Nirankar Singh1, J.V. Singh1 Department of Community Medicine, 1Muzaffarnagar Medical College & Hospital, Muzaffarnagar, 2Subharti Medical College, Meerut, Uttar Pradesh, India Submitted: 18-07-2014 Revised: 22-08-2014 Published: 31-10-2014 ABSTRACT Introduction: Internship period of medical interns of India often have a relatively free time Access this article online after their duty hours, which is nowadays is being more diverted to spending time online Website: on internet, consequently their usage pattern justifi es the study in this area. Materials and Methods: A cross-sectional survey was carried out on all medical Interns of one full batch http://nepjol.info/index.php/AJMS attending department of Community Medicine every month (10 Interns/month-total=100) of DOI: 10.3126/ajms.v6i2.10754 a Private medical College in Muzaffarnagar from 1st July 2013 to 1st July 14. First approval of ethical committee of the of Institution was sought, followed by Medical interns enlisting and then consent were taken for participation in this study. A pre-tested semi-structured questionnaire was e-mailed to collect data from medical interns while maintaining anonymity and data analysis was done using Epi-info software version 7.1.3.3.Results: Internet usage by Interns was found primarily through Smartphone’s (60%), in which Google search & Facebook were used in maximum (69% & 75%).The difference between impact of Internet on daily and professional life of interns was found to be highly statistically signifi cant (X2= 16.82, d.f=1, p<0.001), but there was no association between monthly amount spent on internet and number of hours spent on Internet (X2=0.74, df=1,p>0.05). -

Reg No: Name Reg.No Reg Date 455188 MONICA CHRISTOPHER 77001 14--07--2020 412394 ARYA.V 77003 14--07--2020 328998 Aswathysasidha
List - XXII Permanent Registration Number alone Allotted (Continuation from List XXI) Details of Permanent Register number allotted to Modern medicine Doctors (Applications received up to 20/08/2020) Certificate will be issued after completing all formal procedures Reg No: Name Name of College` Reg.No Reg Date 455188 MONICA CHRISTOPHER TRAVANCORE MEDICAL COLLEGE, MEDICITY, KOLLAM 77001 14--07--2020 412394 ARYA.V JUBILEE MISSION MEDICAL COLLEGE & RESEARCH INSTITUTE, THRISSUR 77003 14--07--2020 328998 AswathySasidharan Government Medical College, Thrissur 77005 14--07--2020 336170 Anjumol T.A Government Medical College, Kottayam 77006 14--07--2020 463840 SHAMSHEEDA GOVERNMENT MEDICAL COLLEGE , KANNUR 77751 18--08--2020 512297 AKSHAY M DILEEP Government Medical College, Kottayam 77752 18--08--2020 506767 NOUREEN FAZAL Government Medical College, Thrissur 77753 18--08--2020 508435 FIDHA FATHIMA SADAR Government Medical College, Kottayam 77754 18--08--2020 505802 NAHJA ROSHIN A.M. TRAVANCORE MEDICAL COLLEGE, MEDICITY, KOLLAM 77756 18--08--2020 481395 AISWARYA VIJAY V J SREE NARAYANA INSTITUTE OF MEDICAL SCIENCES, ERNAKULAM 77757 18--08--2020 506776 SONA MARIA PETER PK DAS INSTITUTE OF MEDICAL SCIENCES, PALAKKAD 77758 18--08--2020 445548 SWABEEHA ABOOBACKER PK DAS INSTITUTE OF MEDICAL SCIENCES, PALAKKAD 77759 18--08--2020 507536 DHEERAJ T. K. D.M. Wayanad Institute of Medical Sciences, Wayanad 77760 18--08--2020 499438 MURSHIDA P MALABAR MEDICAL COLLEGE HOSPITAL AND RESEARCH CENTER, KOZHIKODE 77761 18--08--2020 383612 Bini Cherian JUBILEE MISSION -

The Pneumatic Experiences of the Indian Neocharismatics
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Birmingham Research Archive, E-theses Repository THE PNEUMATIC EXPERIENCES OF THE INDIAN NEOCHARISMATICS By JOY T. SAMUEL A Thesis Submitted to The University of Birmingham for the Degree of DOCTOR OF PHILOSOPHY School of Philosophy, Theology and Religion College of Arts and Law The University of Birmingham June 2018 i University of Birmingham Research e-thesis repository This unpublished thesis/dissertation is copyright of the author and /or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any success or legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. i The Abstract of the Thesis This thesis elucidates the Spirit practices of Neocharismatic movements in India. Ever since the appearance of Charismatic movements, the Spirit theology has developed as a distinct kind of popular theology. The Neocharismatic movement in India developed within the last twenty years recapitulates Pentecostal nature spirituality with contextual applications. Pentecostalism has broadened itself accommodating all churches as widely diverse as healing emphasized, prosperity oriented free independent churches. Therefore, this study aims to analyse the Neocharismatic churches in Kerala, India; its relationship to Indian Pentecostalism and compares the Sprit practices. It is argued that the pneumatology practiced by the Neocharismatics in Kerala, is closely connected to the spirituality experienced by the Indian Pentecostals. -

District Census Handbook
Census of India 2011 KERALA PART XII-B SERIES-33 DISTRICT CENSUS HANDBOOK PATHANAMTHITTA VILLAGE AND TOWN WISE PRIMARY CENSUS ABSTRACT (PCA) DIRECTORATE OF CENSUS OPERATIONS KERALA CENSUS OF INDIA 2011 KERALA SERIES-33 PART XII-B DISTRICT CENSUS HANDBOOK PATHANAMTHITTA VILLAGE AND TOWN WISE PRIMARY CENSUS ABSTRACT (PCA) Directorate of Census Operations, Kerala MOTIF Sabarimala Sree Dharma Sastha Temple A well known pilgrim centre of Kerala, Sabarimala lies in this district at a distance of 191 km. from Thiruvananthapuram and 210 km. away from Cochin. The holy shrine dedicated to Lord Ayyappa is situated 914 metres above sea level amidst dense forests in the rugged terrains of the Western Ghats. Lord Ayyappa is looked upon as the guardian of mountains and there are several shrines dedicated to him all along the Western Ghats. The festivals here are the Mandala Pooja, Makara Vilakku (December/January) and Vishu Kani (April). The temple is also open for pooja on the first 5 days of every Malayalam month. The vehicles go only up to Pampa and the temple, which is situated 5 km away from Pampa, can be reached only by trekking. During the festival period there are frequent buses to this place from Kochi, Thiruvananthapuram and Kottayam. Contents Pages 1 Foreword 1 2 Preface 3 3 Acknowledgement 5 4 History and Scope of the District Census Handbook 7 5 Brief History of the District 9 6 Administrative Setup 12 7 District Highlights - 2011 Census 14 8 Important Statistics 16 9 Section - I Primary Census Abstract (PCA) (i) Brief note on Primary Census Abstract 20 (ii) District Primary Census Abstract 25 Appendix to District Primary Census Abstract Total, Scheduled Castes and (iii) 33 Scheduled Tribes Population - Urban Block wise (iv) Primary Census Abstract for Scheduled Castes (SC) 41 (v) Primary Census Abstract for Scheduled Tribes (ST) 49 (vi) Sub-District Primary Census Abstract Village/Town wise 57 (vii) Urban PCA-Town wise Primary Census Abstract 89 Gram Panchayat Primary Census Abstract-C.D. -
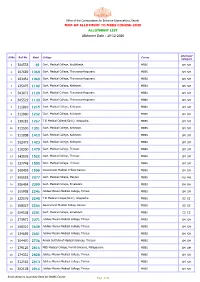
ALLOTMENT LIST MOP-UP ALLOTMENT to MBBS COURSE-2020 Allotment Date
Office of the Commissioner for Entrance Examinations, Kerala MOP-UP ALLOTMENT TO MBBS COURSE-2020 ALLOTMENT LIST Allotment Date : 20-12-2020 Allotment Sl.No. Roll No. Rank College Course Category 1 304533 39 Govt. Medical College, Kozhikkode. MBBS SM SM 2 107669 1068 Govt. Medical College, Thiruvananthapuram. MBBS SM SM 3 103451 1069 Govt. Medical College, Thiruvananthapuram. MBBS SM SM 4 135075 1102 Govt. Medical College, Kottayam. MBBS SM SM 5 303073 1128 Govt. Medical College, Thiruvananthapuram. MBBS SM SM 6 305529 1139 Govt. Medical College, Thiruvananthapuram. MBBS SM SM 7 111810 1215 Govt. Medical College, Kottayam. MBBS SM SM 8 312980 1232 Govt. Medical College, Kottayam. MBBS SM SM 9 130281 1267 T D Medical College(Govt.), Alappuzha. MBBS SM SM 10 311530 1351 Govt. Medical College, Kottayam. MBBS SM SM 11 311808 1410 Govt. Medical College, Kottayam. MBBS SM SM 12 302475 1423 Govt. Medical College, Kottayam. MBBS SM SM 13 110300 1479 Govt. Medical College, Thrissur. MBBS SM SM 14 143076 1522 Govt. Medical College, Thrissur. MBBS SM SM 15 137748 1590 Govt. Medical College, Thrissur. MBBS SM SM 16 300439 1599 Government Medical College Kannur MBBS SM SM 17 305518 2077 Govt. Medical College, Manjeri. MBBS MU MU 18 206454 2099 Govt. Medical College, Ernakulam MBBS BH BH 19 105958 2246 Jubilee Mission Medical College, Thrisur. MBBS SM SM 20 122576 2248 T D Medical College(Govt.), Alappuzha. MBBS EZ EZ 21 168027 2266 Government Medical College Kannur MBBS EZ EZ 22 304538 2281 Govt. Medical College, Ernakulam MBBS EZ EZ 23 173971 2371 Jubilee Mission Medical College, Thrisur. -
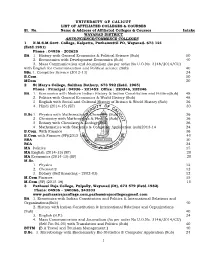
1 University of Calicut List of Affiliated Colleges
UNIVERSITY OF CALICUT LIST OF AFFILIATED COLLEGES & COURSES Sl. No. Name & Address of Affiliated Colleges & Courses Intake WAYANAD DISTRICT ARTS/SCIENCE/COMMERCE COLLEGES 1 N.M.S.M.Govt. College, Kalpetta, Puzhamuttil PO, Wayanad- 673 121 (Estd.1981) Phone : 04936 - 202625 BA 1. History with General Economics & Political Science (Sub) 50 2. Ecconomics with Development Economics (Sub) 40 3. Mass Communication and Journalism (As per order No U.O.No. 3146/2014/CU) with English for Communication and Political science (Sub) 40 BSc.1. Computer Science (2012-13) 24 B.Com 50 MCom 20 2 St Mary's College, Sulthan Bathery, 673 592 (Estd. 1965) Phone : Principal : 04936 - 221452 Office : 220246, 225246 BA 1. Economics with Modern Indian History & Indian Constitution and Politics(Sub) 48 2. Politics with General Economics & World History (Sub) 48 3 English with Social and Cultural History of Britain & World History (Sub) 36 4. Hindi (2014-15) (SF) 30 B.Sc 1. Physics with Mathematics & Chemistry (Sub) 36 2 Chemistry with Mathematics & Physics (Sub) 36 3 Botany with Chemistry & Zoology (Sub) 36 4 Mathematics with Statistics & Computer Application (sub)2013-14 24 B.Com With Finance 36 B.Com with Finance (SF)(2015-16) 40 BBA 30 BCA 24 MA Politics 15 MA English (2014-15) (SF) 20 MA Economics (2014-15) (SF) 20 M.Sc. 1. Physics 12 2. Chemistry 12 3. Botany (Self financing – 2002-03) 12 M.Com Finance 15 M.Com (SF) (2015-16) 15 3 Pazhassi Raja College, Pulpally, Wayanad (Dt), 673 579 (Estd.1982) Phone: 04936 – 240366, 243333 www.pazhassirajacollege.com,[email protected] BA 1. -

MEDIA Handbook 2018
MEDIA hAnDbook 2018 Information & Public Relations Department Government of Kerala PERSONAL MEMORANDA Name................................................................................... Address Office Residence .......................... ............................... .......................... ............................... .......................... ............................... .......................... ............................... .......................... ............................... MEDIA HANDBOOK 2018 .......................... ............................... Information & Public Relations Department .......................... ............................... Government of Kerala Telephone No. Office ............................................... Chief Editor T V Subhash IAS Mobile ............................................... Co-ordinating Editor P Vinod Fax ............................................... Deputy Chief Editor K P Saritha E-mail ............................................... Editor Manoj K. Puthiyavila Residence ............................................. Editorial assistance Priyanka K K Nithin Immanuel Vehicle No .......................................................................... Gautham Krishna S Driving Licence No .............................................................. Ananthan R M Expires on . .......................................................................... Designer Ratheesh Kumar R Accreditation Card No ........................ Date....................... Circulation -

Medical Council of India New Delhi Executive Committee
1 MEDICAL COUNCIL OF INDIA NEW DELHI EXECUTIVE COMMITTEE Minutes of the meeting of the Executive Committee held on 6thFebruary, 2018 at 11.00 a.m. in the Council Office at Sector 8, Pocket 14, Dwarka, New Delhi. *********** Present: President Dr. Jayshree Mehta Medical Council of India, Former Professor of Surgery, Govt. Medical College, Vadodara (Gujarat) Vice-President, Medical Council of India, Dr. C.V. Bhirmanandham Former Vice-Chancellor of Dr. M.G.R. Health University, Chennai (Tamil Nadu) Lab Director, Dr. Ahuja’s Pathology & Imaging Centre, Dr. Alok Ahuja 7-B, Astley Hall, Dehradun (Uttrakhand) Principal, Dr. Anil Chauhan Dr. Radhakrishnan Govt. Medical College, Hamirpur-177001 (Himachal Pradesh) Professor, General Medicine & Superintendent, Sir Ronald Ross Institute Dr. Kampa Shankar of Tropical & Communicable Diseases, Nallkunta, Hyderabad Vice-Chancellor, Ayush & Health Sciences University, G.E. Dr. G.B. Gupta Road, Raipur (Chhatisgarh) Professor of Urology, Rajendra Instt. of Medical Sciences, Dr. Sinam Rajendra Singh Imphal (Manipur) & Director, Manipur Medical Council Imphal, Manipur Professor & Head, Department of Gastroenterology, Dr. Vijay Prakash Singh Patna Medical College, Patna (Bihar) Dr. Reena Nayyar, Secretary I/c. Apology for absence were received from Dr. Narain Venkatesh Bhandare and Dr. Mhaske Chandrakant Bhaskar. 1. Minutes of the Executive Committee Meeting held on 4th January 2018 – Confirmation of. The Executive Committee of the Council confirmed the minutes of the Executive Committee meeting held on 4th January 2018. 2 2. Minutes of the last meeting of the Executive Committee – Action taken thereon. The Executive Committee of the Council noted the action taken on the minutes of the Executive Committee meetings held on 14th December,2017& 4thJanuary, 2018 3.