UC Berkeley UC Berkeley Electronic Theses and Dissertations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Handbook of Cultural Sociology the Subaltern, the Postcolonial, And
This article was downloaded by: 10.3.98.104 On: 27 Sep 2021 Access details: subscription number Publisher: Routledge Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered office: 5 Howick Place, London SW1P 1WG, UK Handbook of Cultural Sociology John R. Hall, Laura Grindstaff, Ming-Cheng Lo The subaltern, the postcolonial, and cultural sociology Publication details https://www.routledgehandbooks.com/doi/10.4324/9780203891377.ch3 Raka Ray, Smitha Radhakrishnan Published online on: 21 Jul 2010 How to cite :- Raka Ray, Smitha Radhakrishnan. 21 Jul 2010, The subaltern, the postcolonial, and cultural sociology from: Handbook of Cultural Sociology Routledge Accessed on: 27 Sep 2021 https://www.routledgehandbooks.com/doi/10.4324/9780203891377.ch3 PLEASE SCROLL DOWN FOR DOCUMENT Full terms and conditions of use: https://www.routledgehandbooks.com/legal-notices/terms This Document PDF may be used for research, teaching and private study purposes. Any substantial or systematic reproductions, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden. The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The publisher shall not be liable for an loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material. Downloaded By: 10.3.98.104 At: 16:39 27 Sep 2021; For: 9780203891377, chapter3, 10.4324/9780203891377.ch3 First published 2010 by Routledge 2 Park Square, Milton Park, Abingdon, Oxon, OX14 4RN Simultaneously published in the USA and Canada by Routledge 270 Madison Avenue, New York, NY 10016 Routledge is an imprint of the Taylor & Francis Group, an informa business This edition published in the Taylor & Francis e-Library, 2010. -

1 Dawne Moon, Ph.D. Associate Professor of Sociology Department of Social & Cultural Sciences PO Box 1881, Marquette Univers
Dawne Moon, Ph.D. Associate Professor of Sociology Department of Social & Cultural Sciences PO Box 1881, Marquette University, Milwaukee WI 53201-1881 [email protected] VITA AUGUST 2019 Education: Ph. D. 2000, University of Chicago, Chicago IL MA 1994, University of Chicago, Chicago IL BA 1991, University of Chicago, Chicago IL Academic Experience: 2014- , Associate Professor, Marquette University 2007-2014, Assistant Professor, Marquette University 2000-2007, Assistant Professor, University of California, Berkeley Fields of Expertise: Gender, sexuality, religion, culture, identity, qualitative methods I. PUBLICATIONS A. Book 2004 Moon, Dawne. God, Sex and Politics: Homosexuality and Everyday Theologies. Chicago, IL: University of Chicago Press. 281 pp. B. Articles (in refereed journals) 2019 Dawne Moon and Theresa W. Tobin. 2019. “Humility: Rooted in Relationship, Reaching for Justice.” Political Power and Social Theory 36, 101-121. 2019 Dawne Moon, Theresa W. Tobin, and J. E. Sumerau. “Alpha, Omega, and the Letters in Between: LGBTQI Conservative Christians Undoing Gender.” Gender & Society 33(4): 583-606. https://doi.org/10.1177/0891243219846592 2019 J. E. Sumerau, Lain A. B. Mathers, and Dawne Moon, “Foreclosing Fluidity at the Intersection of Gender and Sexual Normativities.” Symbolic Interaction. DOI: 10.1002/SYMB.431 2019 Theresa W. Tobin and Dawne Moon. “The Politics of Shame in the Motivation to Virtue: Lessons from the Shame, Pride, and Humility Experiences of LGBT Conservative Christians and their Allies.” Journal of Moral Education. 48(1): 109-125. 2018 Moon, Dawne and Theresa W. Tobin. “Sunsets and Solidarity: Overcoming Sacramental Shame in Conservative Christian Churches to Forge a Queer Vision of Love and Justice.” Hypatia 33(3): 451-468. -

Good Evening. Welcome to You All. I Believe That Both Sociologists and Non- Sociologists Are in the Audience
MICHAEL BURAWOY: Good evening. Welcome to you all. I believe that both sociologists and non- sociologists are in the audience. And this is--the theme of this conference, as you know, is public sociology, and therefore, I am glad to greet the non-sociologists, the public, from the streets of San Francisco. [ Applause ] Today is day three, thank you, day three of the ASA Conference for 2004. And the theme for today, if there has been a theme, is talking to publics. We had a great plenary earlier today, and tonight we have- -we await with great expectation an address from Arundhati Roy. Let me tell you about the rules. Since we are quite numerous here, questions. We will do what we did on day one, two, whatever it was, the other night. There are the Marxist T-shirted Berkeley undergraduates. [ Applause ] Who will be surveilling and patrolling the isles, one on each isle. We've lost a few, but we have in it for one on each isle and one at the back. Questions should be therefore written on pieces of paper and handed to the side. And best if they're not too long those questions. Raka will actually take them, and we'll sort through them, and we'll present them to Arundhati Roy, and there will be little conversation at the front like we did before. Then we make an announcement tomorrow, which is the last day of this conference. There are two events I want to alert you to. There is a closing plenary. We never had a closing plenary before, but we are determined to have a closing plenary this time. -

PRELIMINARY PROGRAM (As of 5/12/2016) This Document Is Subject to Change. Any Changes Made Will Be Made to the Online Program. T
PRELIMINARY PROGRAM (as of 5/12/2016) 459. Thematic Session. Sexuality and Social Change This document is subject to change. Any Session Organizers: Patrick Ryan Grzanka, University of Tennessee changes made will be made to the online Emily S. Mann, University of South Carolina program. Presider: Tom J. Waidzunas, Temple University Panelists: Amin Ghaziani, University of British Columbia Tuesday, August 23 Jyoti Puri, Simmons College Jessica Fields, San Francisco State University The length of each daytime session/meeting activity Georgiann Davis, University of Nevada, Las Vegas is one hour and forty minutes, unless noted Discussant: Tom J. Waidzunas, Temple University Critics of neoliberalism have argued that the early years of the 21st otherwise. The usual turnover is as follows: century have been marked by largely symbolic victories for various 8:30am-10:10am social justice movements. Rather than transform the structures of social 10:30am-12:10pm inequality, social movement politics and discourses have been coopted 12:30pm-2:10pm by conservative institutions that reconstitute equality and justice in the image of corporations and the global power elite. Tolerance, inclusion, 2:30pm-4:10pm and assimilation have displaced the approaches to radical social change advocated by various identity-based social movements, Session presiders and committee chairs are including critical race and ethnic, feminist, workers’ rights, disability, requested to see that sessions and meetings end on and LGBTQIA* activists. This panel explores the capacities of time to avoid conflicts with subsequent activities contemporary social movements to intervene in and disrupt the scheduled into the same room. neoliberal policies and practices that engender, sustain, and exacerbate social inequality. -

Katherine Eva Maich
KATHERINE EVA MAICH Department of Sociology University of California, Berkeley 410 Barrows Hall, Berkeley, CA 94720 [email protected] | 574.383.8992 katherinemaich.com EDUCATION Ph.D. University of California, Berkeley Sociology, expected May 2016 Dissertation: “The Politics of ‘After’: Social Consequences of Domestic Worker Legislation in the U.S. and Latin America.” Committee: Raka Ray (Chair), Kim Voss, Laura Enriquez, Evelyn Nakano Glenn (Ethnic Studies) Examination Areas: Labor and Work, Sociology of Gender, Social Theory Cornell University, ILR School, The Worker Institute Visiting Scholar, 2013-14 M.A. University of California, Berkeley Sociology, December 2009 Thesis: “Disciplined Go-Getters and Passive Onlookers: Gendering Divisions at an Immigrant Worker Center.” Committee: Raka Ray (Chair), Michael Burawoy, Barrie Thorne M.S. University of Massachusetts, Amherst Labor Studies, Graduate Certificate in Advanced Feminist Studies, May 2007 Thesis: “Representations of Gendered Service Workers: Examining Resistance and Agency.” B.A. University of Notre Dame English, Catholic Social Tradition, May 2004 Cum Laude, Sigma Tau Delta RESEARCH AND TEACHING INTERESTS Labor and Work, Social Movements, Gender, Latin America, Social Theory, Law and Society, Qualitative Methods PUBLICATIONS Peer-Reviewed Journal Articles Katherine Eva Maich. 2014. “Marginalized Struggles for Legal Reform: Cross-Country Consequences of Domestic Worker Organizing.” Social Development Issues 36 (3): 73-91. Special Issue: Social Development, Democracy and Human Rights in Latin America. Katherine Eva Maich. 2007. “Feminist Research and Representations of Gendered Service Workers: Examining Resistance, Agency, and Positionality.” Intersections: Women's and Gender Studies in Review across Disciplines 5: 20-28. Katherine Eva Maich 2 Manuscripts Under Review Katherine Eva Maich. “Dispatching Jobs, Dispatching Dignity: An Immigrant Worker Center’s Challenges.” Katherine Eva Maich. -

Raka Ray URSINUS COLLEGE 4:00 P.M
GREATER PHILADELPHIA Sunday, October 21 TEMPLE UNIVERSITY WOMEN’S STUDIES 7:00 p.m. Welcome reception Open to Consortium members CONSORTIUM For information: [email protected] PRESENTS Monday, October 22 VILLANOVA UNIVERSITY Scholar in Residence 12:00 p.m. Luncheon with students and faculty Room 200, Health Services Bldg. 1:30 p.m. Class visits For information: [email protected] Raka Ray URSINUS COLLEGE 4:00 p.m. Seminar: Discussion of Professor Ray’s work on cultures of servitude 6:00 p.m. Dinner with faculty members For information: [email protected] Tuesday, October 23 SAINT JOSEPH’S UNIVERSITY 11:30-1:00 p.m. Teaching Feminism in a Globalizing World: A Pedagogy Discussion Open to Consortium members For information: [email protected] WEST CHESTER UNIVERSITY 3:30 p.m. Roundtable with faculty and students Open to the public. Alumni House For information: [email protected] Associate Professor of Sociology and South and Southeast Asia UNIVERSITY OF DELAWARE Studies, Chair of the Center for South Asia Studies, University 7:30 p.m. Traveling Cultures of Servitude: of California, Berkeley. Her areas of specialization are gender Loyalty and Betrayal in New York and Calcutta and feminist theory, social movements, and relations between Open to the public. 004 Kirkbride dominant and subaltern groups in India. For information: [email protected] Wednesday, October 24 BRYN MAWR COLLEGE 10:00 a.m. Class visits 12:15 p.m. Luncheon, Vernon Room, Haffner Hall Feminism: Is the Revolution Missing or Are We Looking in the Wrong Places? Open to the public. For information: [email protected] DREXEL UNIVERSITY 5:00 p.m. -

Pointers on Pierre Bourdieu and Democratic Politics
Pointers on Pierre Bourdieu and Democratic Politics Loïc Wacquant We underestimate the properly political power to change social life by changing the represention of social life, and by putting a modicum of imagination in power. Pierre Bourdieu, “Donner la parole aux gens sans parole” (1977) Pierre Bourdieu has rarely been read as a political sociologist or philosopher.1 And yet there is sense in which his oeuvre as well as much of his intellectual activity represents a sustained, multiprong attempt to chisel a science of the social conditions of possibility of democracy – broadly defined as that social state wherein everyone would possess both the inclination and the ability to take matters political into their own hands – and to detect the historical pitfalls and possibilities of the struggles aimed at fostering its advance in different realms of life. The epicentral place that the notion of symbolic power and issues of repre- sentation, delegation, nomination, and (mis)recognition occupy in Bourdieu’s work suggest that they constitute a major untapped store of concepts, theories, and insights for rethinking the links between freedom, justice, and politics. It is useful, to elucidate the vexed relation of Bourdieu to the question of demo- cratic politics, to distinguish, if only for the sake of analytical clarity, between three tightly intervoven elements: (1) the personal political views of the individ- ual Pierre Bourdieu, which are pertinent insofar as they animate his scientific practice and civic engagements; (2) politics as encountered -
Political Science MA Syllabus and Examination Rules University Of
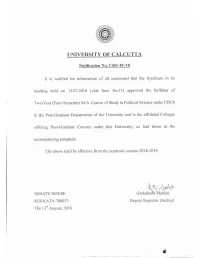
Political Science M.A. Syllabus and Examination Rules University of Calcutta Department of Political Science University of Calcutta Semesterized CBCS Syllabus 1. The Syllabus, if approved, will be operational from the session indicated in the order of the appropriate authority. 2. The M.A. Syllabus in Political Science will be of two years' duration to be divided into 4 semesters of even duration, that is 06 (six) months. 3. There will be 20 Courses – each with 4 credits thereby totalling 80 credits. 4. Each Course will be divided into two Units. 5. Each Course will be of 50 marks – 10 of which will be earmarked for Mid-Semester Internal Assessment in such forms as Written Examinations, Book Reviews, Review Essays, Interviews, Short Projects or any other form that may be decided by the Postgraduate Board of Studies in Political Science from time to time. 6. Reference Lists are only indicative and not exhaustive. 7. Each semester will consist of 5 courses as per the following sequence: Semester I: Core Cluster A: Western Political Thought and Theory Course CCI: Enlightenment and Liberalism Course CCII: Enlightenment: Lineages and Critiques Core Cluster B: Modern India: Ideas, Governance, Politics Course CCIII: Ideational Trajectories and Movements Course CCIV: State, Society and Economy Core Cluster C: Public Administration Course CCV: Theories, Concepts and Organization Semester II: Core Cluster C: Public Administration (Continued) Course CCVI: Public Policy Analysis and Indian Administration Core Cluster D: International Relations Course -

Department of Sociology University of Maryland, College Park 2112 Parren J
DAWN MARIE DOW Department of Sociology University of Maryland, College Park 2112 Parren J. Mitchell Art-Sociology Building College Park, Maryland 20742 work 301-405-6428 / cell 510-847-6768 [email protected] / www.dawndow.com ACADEMIC POSITIONS 2016-Present Assistant Professor, Department of Sociology, University of Maryland, College Park. Faculty Associate, Maryland Population Research Center 2012-2016 Assistant Professor, Department of Sociology, Maxwell School of Citizenship and Public Affairs, Syracuse University. Faculty Fellow, Institute for the Study of the Judiciary, Politics and the Media, Maxwell School of Citizenship and Public Affairs, Syracuse University. 2015-2016 Humanities Center Faculty Fellow, Syracuse University. EDUCATION 2012 Ph.D., UNIVERSITY OF CALIFORNIA, BERKELEY, SOCIOLOGY Dissertation: “Racial Distinctions in Middle-Class Motherhood: Ideologies and Practices of African American Middle-Class Mothers as Women, Mothers and Parents.” Committee: Raka Ray (Chair), Barrie Thorne, Evelyn Nakano Glenn (Ethnic Studies). Exam Fields: Sociological Theory, Sociology of Law, Gender (with an emphasis in Race and Ethnicity and Family). 2007 M.A., UNIVERSITY OF CALIFORNIA, BERKELEY, SOCIOLOGY Thesis: “Determinants of Employment of African American and White Mothers Raising Preschool Aged Children: Integrated versus Traditional Ideologies of Motherhood.” 2000 J.D., COLUMBIA UNIVERSITY, SCHOOL OF LAW 1996 B.A., BRYN MAWR COLLEGE, SOCIOLOGY Distinctions: Degree in Sociology with Honors. Minor in Africana Studies. Thesis: “Economic -

Raka-Ray-Cv.Pdf
RAKA RAY CURRENT POSITION Professor Department of Sociology Professor Department of South and Southeast Asian Studies University of California, Berkeley EDUCATION 1993 Ph.D (Sociology). University of Wisconsin-Madison. 1987 M.S. (Sociology). University of Wisconsin-Madison. 1985 A.B. (Sociology). Magna Cum Laude. Bryn Mawr College. ACADEMIC AWARDS AND HONORS 2013 UC-Berkeley Graduate Division Graduate Mentoring Award 2003-2012 Sarah Kailath Chair of India Studies 2010 (with Sanchita Saxena) Department of Education Title VI Grant for South Asia National Resource Center at the University of California, Berkeley, for 2010-14; and Foreign Language and Area Studies Fellowships Grant, for 2010-14. 2010 Department of Sociology Graduation Keynote speaker, May. 2009 Mellon Project Grant, UC Berkeley 2009 Humanities Research Fellowship, UC Berkeley 2007 Invited Scholar in Residence, Greater Philadelphia Gender Consortium 2007 Ford Foundation Grant for research on ‘The Middle Classes in India: Identity, Citizenship and the Public Sphere’ 2006 Rockefeller Foundation Fellowship, Bellagio 2006 (with Daisy Rockwell) Department of Education Title VI Grant for South Asia National Resource Center at the University of California, Berkeley, for 2006-10; and Foreign Language and Area Studies Fellowships Grant, for 2006-10. 2003-2004 Townsend Center for the Humanities Initiative Grant 2001-2002 AIIS/National Endowment for the Humanities Senior Fellowship. 2001 Faculty Research Grant, COR, University of California, Berkeley. 1998 Chancellor’s Initiative Grant, UC- Berkeley. 1998 Women’s Studies Graduation Keynote Speaker, UC-Berkeley, May. 1997 Distinguished Teaching Award for the Social Sciences Division, UC-Berkeley. 1995-96 Junior Faculty Research Grant, UC-Berkeley. 1994-95 Career Development Grant, UC-Berkeley. -

What's Wrong with Prostitution? What's Right with Sex Work? Comparing Markets in Female Sexual Labor Elizabeth Bernstein
Hastings Women’s Law Journal Volume 10 Number 1 Symposium Issue: Economic Justice for Sex Article 6 Workers 1-1-1999 What's Wrong with Prostitution? What's Right with Sex Work? Comparing Markets in Female Sexual Labor Elizabeth Bernstein Follow this and additional works at: https://repository.uchastings.edu/hwlj Recommended Citation Elizabeth Bernstein, What's Wrong with Prostitution? What's Right with Sex Work? Comparing Markets in Female Sexual Labor, 10 Hastings Women's L.J. 91 (1999). Available at: https://repository.uchastings.edu/hwlj/vol10/iss1/6 This Article is brought to you for free and open access by the Law Journals at UC Hastings Scholarship Repository. It has been accepted for inclusion in Hastings Women’s Law Journal by an authorized editor of UC Hastings Scholarship Repository. For more information, please contact [email protected]. What's Wrong with Prostitution? What's Right with Sex Work? Comparing Markets in Female Sexual Labort Elizabeth Bernstein * I. INTRODUCTION This article stems from an interest in some of the recent debates in American feminist theory over sexuality and empowerment. By the late eighties, participants in the already polarized "sexuality debates" had formed two clearly demarcated camps around such policy issues as pornography and prostitution, and around the underlying questions of power, resistance and the possibility of female sexual agency under patriarchy.} While the figure of the prostitute has served as a key trope in the writings and arguments of both groups-as symbolic of either the expropriation of female sexuality in general, or alternatively, of its socially subversive reappropriation-there has been surprisingly little empirical research done to investigate the lived conditions of contemporary prostitution.2 Amongst feminists, prostitution has been abundantly t The title for this article was inspired by Christine Overall's 1992 essay, What's Wrong with Prostitution? Evaluating Sex Work, in SIGNS: J. -
Feminist Practices in a Global Context
Prof. WANG Zheng Office Hours: Tue. 4:00-5:00 Women’s Studies Program By appointment 2156 Lane Hall, 763-6635 [email protected] Syllabus Winter 2006 WS 357 Th. 1:00-4:00 pm, 3510 FB Feminist Practices in a Global Context Feminist activism has long been a global phenomenon. How do we understand feminist practices in various locations as well as the relationships between feminisms in the east and west, and the local and global? When racial relations, sexuality, and abortion right are important issues for feminists in the US, what are the major issues concerning feminists in other countries? Without assuming a universal course of development of women’s activism, this course adopts a comparative approach to the investigation of particular historical processes of women’s movements in three countries, the United States, India, and China. Focusing on the feminist activism in the three countries, this course attempts to ground our understanding of globalization in local history, and to present in a concrete way that feminisms have histories and meanings that extend far beyond the North American continent. By comparison, we also hope to illuminate the cultural parameters of each location that have shaped various feminist practices. Personal narratives (in both textual and visual forms) of feminist activists from the three locations constitute the main body of texts for this course. Other readings and documentaries will provide historical backgrounds to these personal narratives. Students will be encouraged to actively participate in analyzing and comparing the textual and visual material in the process of learning diverse feminist issues crossing national boarders and from the personal to the political.