27. Assessment of Injection Practices in India
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Domain Fresh Registration Analysis Report This Has a Reference to The
Domain Fresh Registration Analysis report This has a reference to the DOMAIN SKILLING SKILL DEVELOPMENT CENTER REGISTRATION on Bihar Skill Development Mission (BSDM) portal based on the demand for SDC requirements received from various funding departments / entities. In order to empanel fresh applicants against the requirements received the DOMAIN SKILLING SKILL DEVELOPMENT CENTER REGISTRATION 2018 process was commenced on the 17th of July, 2018. The last date for entering into the registration process was 3rd September, 2018 and the Last date for reaching the DMT stage was 7th September, 2018. The DOMAIN SKILLING SKILL DEVELOPMENT CENTER REGISTRATION 2018 process was a restricted registration process opened for a specific set of Courses and Districts/Blocks/Urban Local Bodies (ULB). The course-wise and location wise SDC requirement is also a part of Annexure 1 for your reference. There were multiple applications received against the various requirements and thus as indicated in the DOMAIN SKILLING SKILL DEVELOPMENT CENTER REGISTRATION process noticedated 10th July, 2018 the First-Come-First-Serve (FCFS) algorithm was used based on the timestamp of reaching the DMT stage. The statistics of the analysis / evaluation done by the concerned district in-charges is as follows: Sl. No. Particulars Total Remarks Total BSDM location-course combination 1 requirements 479 2 Total applications received 5080 Were Animal Husbandry & Fisheries Dept. TPs who had applied through this 3 Total applications not a part of this process 5 process by mistake Total applications that reached DMT after cut- 4 off date(7-9-18) 212 5 Total applications considered for evaluation 4863 6 Total eligible applicants 3461 7 Total ineligible applicants 1402* Total requirements with no eligible 8 applications 24 Total requirements for which center selection 9 happened 455 *The 3 reasons of ineligibility establishment during evaluation were as follows: The sector corresponding to the course chosen is not as per the sector stated in the requirement floated. -
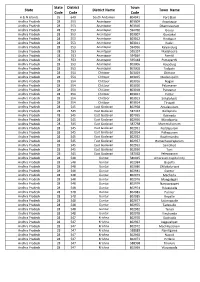
Statutory Towns Size
State District Town State District Name Town Name Code Code Code A & N Islands 35 640 South Andaman 804041 Port Blair Andhra Pradesh 28 553 Anantapur 803009 Anantapur Andhra Pradesh 28 553 Anantapur 803010 Dharmavaram Andhra Pradesh 28 553 Anantapur 594760 Gooty Andhra Pradesh 28 553 Anantapur 803007 Guntakal Andhra Pradesh 28 553 Anantapur 803012 Hindupur Andhra Pradesh 28 553 Anantapur 803011 Kadiri Andhra Pradesh 28 553 Anantapur 594956 Kalyandurg Andhra Pradesh 28 553 Anantapur 595357 Madakasira Andhra Pradesh 28 553 Anantapur 594864 Pamidi Andhra Pradesh 28 553 Anantapur 595448 Puttaparthi Andhra Pradesh 28 553 Anantapur 803006 Rayadurg Andhra Pradesh 28 553 Anantapur 803008 Tadpatri Andhra Pradesh 28 554 Chittoor 803019 Chittoor Andhra Pradesh 28 554 Chittoor 803015 Madanapalle Andhra Pradesh 28 554 Chittoor 803016 Nagari Andhra Pradesh 28 554 Chittoor 803020 Palamaner Andhra Pradesh 28 554 Chittoor 803018 Punganur Andhra Pradesh 28 554 Chittoor 803017 Puttur Andhra Pradesh 28 554 Chittoor 803013 Srikalahasti Andhra Pradesh 28 554 Chittoor 803014 Tirupati Andhra Pradesh 28 545 East Godavari 802958 Amalapuram Andhra Pradesh 28 545 East Godavari 587337 Gollaprolu Andhra Pradesh 28 545 East Godavari 802955 Kakinada Andhra Pradesh 28 545 East Godavari 802956 Mandapeta Andhra Pradesh 28 545 East Godavari 587758 Mummidivaram Andhra Pradesh 28 545 East Godavari 802951 Peddapuram Andhra Pradesh 28 545 East Godavari 802954 Pithapuram Andhra Pradesh 28 545 East Godavari 802952 Rajahmundry Andhra Pradesh 28 545 East Godavari 802957 Ramachandrapuram -

City Wise Progress
CITY wise details of PMAY(U) Financial Progress (Rs in Cr.) Physical Progress (Nos) Sr. Central Central State /City Houses Houses Houses No. Investment Assistance Assistance Sanctioned Grounded* Completed* Sanctioned Released A&N Island 1 Port Blair 151.59 8.96 0.46 598 38 25 Andhra Pradesh 1 Penukonda 200.68 62.43 - 4162 3 0 2 Thallarevu 0.58 0.35 0.15 23 23 12 3 Pendurthi 268.45 120.57 28.37 8038 1030 264 4 Naidupeta 288.43 68.84 36.18 4592 3223 2430 5 Amaravati 360.24 76.27 76.36 5069 5069 5069 6 Hukumpeta 0.19 0.02 0.02 1 1 1 7 Palakonda 83.36 35.55 9.40 2364 1218 969 8 Tekkali 515.94 219.62 13.61 14641 93 0 9 Anandapuram 0.29 0.02 0.02 1 1 1 10 Anandapuram 0.12 0.03 0.03 1 1 1 11 Kothavalasa 0.26 0.01 0.01 2 2 2 12 Thotada 0.60 0.06 0.06 3 3 3 13 Thotada 0.55 0.06 0.06 3 3 3 14 jammu 0.15 0.01 0.01 1 1 1 15 Gottipalle 0.25 0.02 0.02 1 1 1 16 Narasannapeta 329.42 149.11 17.88 9939 2108 237 17 Boddam 0.14 0.03 0.03 1 1 1 18 Ragolu 0.22 0.02 0.02 1 1 1 19 Patrunivalasa 0.70 0.11 0.11 5 5 5 20 Peddapadu 0.20 0.02 0.02 1 1 1 21 Pathasrikakulam 3.58 0.29 0.29 13 13 13 22 Balaga(Rural) 2.44 0.21 0.21 10 10 10 23 Arsavilli(Rural) 2.51 0.19 0.19 9 9 9 24 Ponduru 0.32 0.02 0.02 1 1 1 25 Jagannadharaja Puram 0.50 0.08 0.08 4 4 4 26 Ranastalam 0.15 0.02 0.02 1 1 1 27 Tekkali 0.15 0.02 0.02 1 1 1 28 Shermahammadpuram 0.95 0.12 0.12 6 6 6 29 Pudivalasa 0.27 0.02 0.02 1 1 1 30 Kusalapuram 2.23 0.16 0.16 7 7 7 31 Thotapalem 0.79 0.10 0.10 4 4 4 32 Etcherla 227.17 121.97 25.56 8130 3904 276 33 Yegulavada 0.32 0.05 0.05 2 2 2 34 Kurupam 109.03 49.32 -

Arts /Commerce Bite Musapur Erce Bite Musapur ( KATIHAR ) 2019-21
Arts /Commerce Bite Musapur ( KATIHAR ) 2019-21 Category Gen Merit Sl Candidate Qualifica Categor Reg. Id Gender Father's Name Village Post District DOB Mark Mobile No. Reg. Date No. Name tion y s C/O-PATNA X-RAY & 1 IMAGING CENTRE, NEHA CHANDRA LINE BAZAR Intermed BITEMP2019051019581 KUMARI Female KISHOR THAKUR PURNEA PURNEA Purnea 06/05/2001 iate 83.9 Gen 8521144057 10/05/2019 D/O- PANKAJ 2 KUMAR GOKUL AKRITI KRISHNA ASHRAM Intermed BITEMP2019051119916 KUMARI Female PANKAJ KUMAR ROAD PURNEA Purnea 02/10/2001 iate 83.9 Gen 7488626817 11/05/2019 3 ABHILAASH ASHISH KUMAR Intermed BITEMP2019051522280 A RASHMI Female JHA SUKHANAGAR SUKHANAGAR Supaul 01/07/1997 iate 82.3 Gen 9457991766 15/05/2019 AT JAYPRAKASH NAGAR LAW 4 COLLEGE ROAD SUBHASHI MANOJ KUMAR NEAR PURNEA Intermed BITEMP2019051521693 NI KUMARI Female SINGH COLLEGE HOSTEL PURNEA Purnea 10/04/2001 iate 79.7 Gen 9430635194 15/05/2019 AKANKSHA SHREE 5 MANI NARAYAN Intermed BITEMP2019051522010 TRIPATHI Female TIWARI SIWANA GURUBAZAR Katihar 21/10/1999 iate 77.9 Gen 8235543490 15/05/2019 6 AT-COLONY NO-1 , KUMAR NEAR KALI MANDIR Intermed BITEMP2019043017522 GOURAV Male BIRENDRA JHA , KUMAR BHAWAN KATIHAR Katihar 02/01/1997 iate 77.3 Gen 7549167469 30/04/2019 SHASTRI NAGAR 7 SUCHITA D/O SARWAJEET MADHUBANI MADHUBANI Intermed BITEMP2019051623659 ANAND Female KUMAR PURNEA PURNEA Purnea 15/04/2001 iate 76.2 Gen 7903815884 16/05/2019 SHASTRI NAGAR 8 SUCHITA D/O SARWAJEET MADHUBANI MADHUBANI Intermed BITEMP2019051623691 ANAND Female KUMAR PURNEA PURNEA Purnea 15/04/2001 iate 76.2 Gen 6203704756 -

CENTRAL COALFIELDS LIMITED OFFICE of the GENERAL MANAGER (B&K) AREA PO: BERMO, DIST.: Bokaro , PIN - 829104______
CENTRAL COALFIELDS LIMITED OFFICE OF THE GENERAL MANAGER (B&K) AREA PO: BERMO, DIST.: Bokaro , PIN - 829104____________ Ref No.: CCL/B&K/GMU/Civil/NIQ/19-20/ 115 Date: 03 .10. 2019 NOTICE INVITING QUOTATION (NIQ) QUOTATION NOTICE NO. - 10 of 2019-20 01. Sealed Quotation in one part is invited from eligible contractors for the following work:- 02. Sl. Description of work Estimated Earnest Money Period of No. Cost of (Rs.) Completion work (Rs.) 1 Providing approach road near west bank to 174346.60 2200.00 30 Days Damodar river at Kargali under G.M.unit of B&K Area 2 Making 04 nos. dustbin at senior quarter, 160366.84 2050.00 30 Days Rest House, Double storied and near Mahila Mandal under G.M.unit of B&K Area 3 Renovation of 200 ft. drain facility at 183403.70 2300.00 30 Days Chalkari Basti near Hari Mandir under G.M.unit of B&K Area 4 Jungle cleaning, leveling, dressing and 182777.30 2300.00 30 Days landscaping of filter plant under G.M.unit, B&K Area 5 Providing NP2 class 150 mm RCC pipe for 179702.78 2300.00 30 Days drainage waste water & sludge at Chalkari basti under G.M.Unit of B&K Area 6 Repair & maintenance including roof 170528.30 2150.00 30 Days grading of qtr. No. 2A/4 hospital colony occupied by Sri Kundan Kumar SO (MM), Dhori Area under G.M.Unit B&K Area 03. Earnest money can be deposited in the form of Bank Draft drawn in favour of “CCL B&K Area” on any Nationalised Bank Payable at “SBI, Phusro Bazar, BTPS, Bokaro Colliery”. -

ST Code DT Code SDT Code Town Code Town Name 10 000 00000
MDDS e-GOVERNANCE CODE (Census 2011 PLCN) ST Code DT Code SDT Code Town Code Town Name 10 000 00000 000000 BIHAR 10 203 00000 000000 Pashchim Champaran 10 203 01013 000000 Sidhaw 10 203 01014 000000 Ramnagar 10 203 01014 801277 Ramnagar (NP) 10 203 01015 000000 Gaunaha 10 203 01016 000000 Mainatanr 10 203 01017 000000 Narkatiaganj 10 203 01017 801278 Narkatiaganj (Nagar Parishad) 10 203 01018 000000 Lauriya 10 203 01019 000000 Bagaha 10 203 01019 801279 Bagaha (Nagar Parishad) 10 203 01020 000000 Piprasi 10 203 01021 000000 Madhubani 10 203 01022 000000 Bhitaha 10 203 01023 000000 Thakrahan 10 203 01024 000000 Jogapatti 10 203 01025 000000 Chanpatia 10 203 01025 801280 Chanpatia (NP) 10 203 01026 000000 Sikta 10 203 01027 000000 Majhaulia 10 203 01028 000000 Bettiah 10 203 01028 801281 Bettiah (Nagar Parishad) 10 203 01029 000000 Bairia 10 203 01030 000000 Nautan 10 204 00000 000000 Purba Champaran 10 204 01031 000000 Raxaul 10 204 01031 801282 Raxaul Bazar (Nagar Parishad) 10 204 01032 000000 Adapur 10 204 01033 000000 Ramgarhwa 10 204 01034 000000 Sugauli Page 1 of 21 MDDS e-GOVERNANCE CODE (Census 2011 PLCN) ST Code DT Code SDT Code Town Code Town Name 10 204 01034 801283 Sugauli (NP) 10 204 01035 000000 Banjaria 10 204 01036 000000 Narkatia 10 204 01037 000000 Bankatwa 10 204 01038 000000 Ghorasahan 10 204 01039 000000 Dhaka 10 204 01039 801284 Dhaka (NP) 10 204 01040 000000 Chiraia 10 204 01041 000000 Motihari 10 204 01041 801285 Motihari (Nagar Parishad) 10 204 01042 000000 Turkaulia 10 204 01043 000000 Harsidhi 10 204 01044 000000 -

District Census Handbook, Belgaum, Part XII-B, Series-11
CENSUS OF INDIA 1991 Series ·11 KARNATAKA DISTRICT CENSUS HANDBOOK BELGAUM DISTIUCf PART XII·B VILLAGE AND TOWN WISE PRIMARY CENSUS ABSTRACT SOBHA NAMBISAN Director or Census Operations, Kamataka CONTENTS • ..ge No. FOREWORD v - vi PREFACE vii-viii IMPORTA..W STATISTICS ix - xii ANALYTICAL NOTE 1 - 37 Explanatory Notes 41 - 44 A. District Primary Census Abstract 46-63 (i) Village/l'own~ Primary Census Abstract Alphabetical List of Villages - Athni C.D.Block 67 - 69 Primary CeQ$us Abstract - Athni C.D.Block 70 - 81 Alphabetical Lis1 of Villages - Belgaum C.D.Block 85-88 Primary Census Abstract - Belgaum C.D.Block 90 - 109 Alphabetical List of Villages - Chikodi CD.Block 113 - 115 P~ Census Abstract - Chikodi C.D.Block 116 - 131 Alphabetical List of Villages - Gokak C.D.Block 135 - 137 Primary Census Abstract - Gokak C.D.Block 138 - 153 Alphabetical List of Villages - Hukeri C.D.Block 157 - 160 Primary Census Abstract - Hukeri C.D.Block 162 - In Alphabetical List of Villages - Kbanapur C.D.Block 181 - 186 Primary Census Abstract - .Kbanapur C.D.Block 188 - 215 Alphabetical List of Villages - Parasgad C.D.Block· 219 - 221 Primary Census Abstract - Parasgad C.D.Block 222 - 237 : . Alphabetical List P~ Villages - R.ybag C.D.Block 241 - 242 Primary CensUs Abstract - Raybag C.D.Block 244 - 251 Alphabetical List of Villages - Ramdurg C.D.Block 255 - 257 Primary Ceqsus Abstract - Ramdurg C.D.Block 258 - 273 i Alphabetical List oLVillages - Sampgaon CD:Block m - '1PIJ Primary Census Abstract -- Sampgaon C.D.Block m - '1!:1T (iii) Page No. (ii) Town Primary Census Abstract (Wardwise) Alphabetic:al List of Towns in the District 301 Athni 302 - 305 Bailhoagal 302 - 303 Chikodi 302 - 305 Dhupdal 302 - 305 Gobk 302 - 305 , Gokak FaDs (NAC) 306 - 309 . -

7Th Common Review Mission- Jharkhand
7TH COMMON REVIEW MISSION- JHARKHAND 11TH NOVEMBER- 17TH NOVEMBER M i n i s t r y O f H e a l t h & F a m i l y W e l f a r e , G o v e r n m e n t o f I n d i a Table of Contents Team Composition 2 Facilities visited 2 Profile of the State 3 Summary of Findings 7 TOR 1. Service Delivery 13 TOR 2. Reproductive and Child Health 24 TOR 3. Disease Control Pgrammes 38 TOR 4. Human Resource & Training 42 TOR 5. Community Process & Training 47 TOR 6. Information and Knowledge 53 TOR 7. Health Care Financing 58 TOR 8. Medicine and Technology 63 TOR 9. National Urban Health Mission 65 TOR 10. Governance and Management 67 NUHM FGD1 71 NUHM FGD 2 73 NUHM FGD 3 76 th 7 Common Review Mission Jharkhand Report Page | 1 Team Members District Bokaro District Sahebganj Mr. Dilip Kumar, Director (NRHM) Mr. Vikas Arya, Director (EPW) Mr Sanjay Kumar, Deputy Director (MCTS) Dr. Bhattacharya, NVBDCP Dr. M Jalis Subhani Deputy Advisor (AYUSH) Mr. Samarjit Chakraborthy, State Director PFI Dr Sachin Gupta, USAID Dr. Sovesh Dass, Consultant MoHFW Dr Mithila Dayanithi Consultant MoHFW Ms. Monica Chaturvedi, PHFI Mr Prabhash Jha, Consultant MoHFW Dr Shalini Singh, Consultant NHSRC Ms. Shraddha Masih, Consultant MoHFW Facilities Visited District Bokaro District Sahebganj SDH Chas Sadar Hospital, Sahibganj CHC Nawadih SDH Rajmahal CHC Peterwar CHC Taljhari CHC Chas PHC Udhawa APHC Chalkari PHC Mirzachoki HSC Chapri HSC Koyla Bazar HSC Harladih HSC Khorikhotana HSC Partar HSC Tertaria HSC Bijulia HSC Madansahi Bokaro General Hospital HSC Maharajpur UHC Yadohadih More HSC Sakrigali and Sahiya meeting AWC Pindrar VHND HSC Karalh (Khorikhotana) MMU Umari MCH, MTC, Mamta Vahan th 7 Common Review Mission Jharkhand Report Page | 2 1. -

29/01/2020 Government of Karnataka Page: 88
29/01/2020 GOVERNMENT OF KARNATAKA PAGE: 88 DEPARTMENT OF PRE UNIVERSITY EDUCATION LIST OF PU COLLEGES IN CHIKODI DISTRICT AS ON 29/01/2020 ******************************************************************************** SLNO COLCD NAME AND ADDRESS YEAR OF OPEN & COLL TYPE OPENING & AIDED GO NOS. WITH DATE ******************************************************************************** 1177 DC013 GI BAGEWADI PU COLLEGE 61-62 BIFUR PU COL NIPANI CHIKODI TQ ED 031 UPC 61 DT 30-09-1961 BELGAUM DT 591237 -------------------------------------------------------------------------------- 1178 DC015 GOVT EX-MUNICIPAL PU COL 81-82 GOVT PU COL GOKAK ED 16 SHM 81 DT 01-07-1981 BELGAUM DT 591307 -------------------------------------------------------------------------------- 1179 DC016 SDVS SANGHA'S PU COLLEGE BIFUR PU COL SANKESHWAR HUKKERI TQ BELGAUM DT 591313 -------------------------------------------------------------------------------- 1180 DC018 BASAPRABHUKORE PU COLLEGE 69-70 BIFUR PU COL CHIKODI ANKALI ROAD AC2 GIA-MG 70-71 DT 16-11-1970 BELGAUM DT 591201 -------------------------------------------------------------------------------- 1181 DC025 S S M S PU COLLEGE BIFUR PU COL ATHANI BELGAUM DT 591304 -------------------------------------------------------------------------------- 1182 DC026 SHIVANANDA COLLEGE 67-68 BIFUR PU COL KAGVAD ATHANI TQ ED 94 UAC 67 DT 30-10-1967 BELGAUM DT 591223 -------------------------------------------------------------------------------- 1183 DC028 JA COMP PU COLLEGE 72-73 AIDED PU COL ATHANI ED 19 TPU 72 DT -

1 the Presentation on EIA & EMP for Environmental Clearance of Konar
The presentation on EIA & EMP for Environmental Clearance of Konar Exp OCP (8.0 MTPA normative capacity/11.0 MTPA peak capacity & integrated non-coking coal washery of 7.0 MTPA) was made on 23.06.2016. The EAC, MOEF&CC noted following points/ raised queries. SN Observation of EAC Reply/ Status 1. The proposal envisages The TOR for Konar Expansion OCP amalgamation of Konar OCP and was issued with increase in project the Khasmahal OCP (sanctioned area from 520.93 Ha to 729.40 Ha. /granted individually earlier) followed by integration with the proposed In the prescribed TOR, the EAC washery of 7 MTPA. That would desired that project proponent may involve correction in area from the explore the possibility of reducing present of 620.08 ha to 547.38 ha. forest land requirement by locating The documentation needs to be the washery & FBC plant in non- revised accordingly. forest land. The project area of Khasmahal OCP as per EC condition is 318.71 Ha & Konar OCP is 301.37 Ha. The combined area comes to 620.08 Ha. However, these project areas overlap with each other to accommodate the common external OB dump for the two mines (to the extent of 99.16 Ha). After deducting the common area, the net project area of Khasmahal OCP as per EC condition is 219.56 Ha & Konar OCP is 301.37 Ha. Accordingly net combined project area of existing project becomes 520.93 Ha not 620.08 Ha. In view of observations of EAC regarding reduced use of forest land to the extent possible, the project area was reworked including reduction in area required for future use & boundary rationalisation. -

Bedkar Veedhi S.O Bengaluru KARNATAKA
pincode officename districtname statename 560001 Dr. Ambedkar Veedhi S.O Bengaluru KARNATAKA 560001 HighCourt S.O Bengaluru KARNATAKA 560001 Legislators Home S.O Bengaluru KARNATAKA 560001 Mahatma Gandhi Road S.O Bengaluru KARNATAKA 560001 Rajbhavan S.O (Bangalore) Bengaluru KARNATAKA 560001 Vidhana Soudha S.O Bengaluru KARNATAKA 560001 CMM Court Complex S.O Bengaluru KARNATAKA 560001 Vasanthanagar S.O Bengaluru KARNATAKA 560001 Bangalore G.P.O. Bengaluru KARNATAKA 560002 Bangalore Corporation Building S.O Bengaluru KARNATAKA 560002 Bangalore City S.O Bengaluru KARNATAKA 560003 Malleswaram S.O Bengaluru KARNATAKA 560003 Palace Guttahalli S.O Bengaluru KARNATAKA 560003 Swimming Pool Extn S.O Bengaluru KARNATAKA 560003 Vyalikaval Extn S.O Bengaluru KARNATAKA 560004 Gavipuram Extension S.O Bengaluru KARNATAKA 560004 Mavalli S.O Bengaluru KARNATAKA 560004 Pampamahakavi Road S.O Bengaluru KARNATAKA 560004 Basavanagudi H.O Bengaluru KARNATAKA 560004 Thyagarajnagar S.O Bengaluru KARNATAKA 560005 Fraser Town S.O Bengaluru KARNATAKA 560006 Training Command IAF S.O Bengaluru KARNATAKA 560006 J.C.Nagar S.O Bengaluru KARNATAKA 560007 Air Force Hospital S.O Bengaluru KARNATAKA 560007 Agram S.O Bengaluru KARNATAKA 560008 Hulsur Bazaar S.O Bengaluru KARNATAKA 560008 H.A.L II Stage H.O Bengaluru KARNATAKA 560009 Bangalore Dist Offices Bldg S.O Bengaluru KARNATAKA 560009 K. G. Road S.O Bengaluru KARNATAKA 560010 Industrial Estate S.O (Bangalore) Bengaluru KARNATAKA 560010 Rajajinagar IVth Block S.O Bengaluru KARNATAKA 560010 Rajajinagar H.O Bengaluru KARNATAKA -
Online & Offline Total Website List.Xlsx
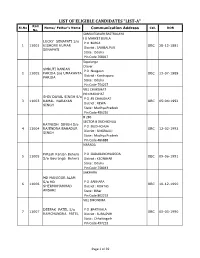
LIST OF ELIGIBLE CANDIDATES "LIST-A" Roll Sl.No Name/ Father's Name Communication Address Cat. DOB No. SAMALESWARI BASTRALAYA I G MARKET BURLA LUCKY SENAPATI S/o P O :BURLA 1 11001 KISHORE KUMAR OBC 28-12-1991 District : SAMBALPUR SENAPATI State : Odisha Pin Code 768017 Sapalanga Olaver SMRUTI RANJAN P O :Nuagaon 2 11002 PARIDA S/o UMAKANTA OBC 13-07-1989 District : Kendrapara PARIDA State : Odisha Pin Code 754227 VILL CHAKGHAT PO CHAKGHAT SHIV DAYAL SINGH S/o P O :PS CHAKGHAT 3 11003 KAMAL NARAYAN OBC 05-04-1992 District : REWA SINGH State : Madhya Pradesh Pin Code 486226 B 286 SECTOR B DUDHICHUA RATNESH SINGH S/o P O :DUDHICHUA 4 11004 RAJENDRA BAHADUR OBC 12-02-1993 District : SINGRAULI SINGH State : Madhya Pradesh Pin Code 486888 NARADA Pritesh Ranjan Behera P O :GADABANDHAGODA 5 11005 OBC 09-06-1991 S/o Gouranga Behera District : KEONJHAR State : Odisha Pin Code 758043 SAKHARA MD MANJOOR ALAM S/o MD P O :SAKHARA 6 11006 OBC 10-12-1990 SHERMOHAMMAD District : ROHTAS ANSARI State : Bihar Pin Code 802219 VILL DHONDHA DEEPAK PATEL S/o P O :BARTIKALA 7 11007 OBC 05-03-1990 RAMCHANDRA PATEL District : SURAJPUR State : Chhattisgarh Pin Code 497223 Page 1 of 39 TOPA COLLIERY LCH-170 ANIL KUMAR GUPTA P O :TOPA COLLIERY 8 11008 OBC 04-10-1986 S/o KRISHNA SAO District : RAMGARH State : Jharkhand Pin Code 825330 VILL- UKHARBERWA SUGIA KAILASH MAHTO S/o P O :KARMA 9 11009 OBC 14-12-1988 SITAL MAHTO District : RAMGARH State : Jharkhand Pin Code 829117 THOUBAL WANGMATABA WAIKHOM THAKUR P O :THOUBAL 10 11010 SINGH S/o W JILLA OBC 02-03-1991 District