Approved Minutes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Schools Are Listed Alphabetically in Associated School Groups. Secondary School Highlighted in Yellow
Schools are listed alphabetically in Associated School Groups. Secondary school highlighted in Yellow NAME & ADDRESS HEAD TEACHER CONTACT DETAILS Aberdeen Grammar School Graham Legge Tel: 01224 642299 Fax: 01224 627413 Skene Street Aberdeen AB10 1HT [email protected] www.grammar.org.uk Ashley Road School Anne Wilkinson Tel: 01224 588732 Fax: 01224 586228 45 Ashley Road Aberdeen AB10 6RU [email protected] www.ashleyroad.aberdeen.sch.uk Gilcomstoun School Stewart Duncan Tel: 01224 642722 Fax: 01224 620784 Skene Street Aberdeen AB10 1PG [email protected] www.gilcomstoun.aberdeen.sch.uk Mile End School Eleanor Sheppard Tel: 01224 498140 Fax: 01224 208758 Midstocket Road Aberdeen AB15 5PD [email protected] www.mileend.aberdeen.sch.uk Skene Square School Eileen Jessamine Tel: 01224 630493 Fax: 01224 620788 61 Skene Square Aberdeen AB25 2UN [email protected] www.skenesquare.aberdeen.sch.uk St Joseph’s RC School Catherine Tominey Tel: 01224 322730 Fax: 01224 325463 5 Queens Road Aberdeen AB15 4YL [email protected] www.stjosephsprimary.aberdeen.sch.uk NAME & ADDRESS HEAD TEACHER CONTACT DETAILS Bridge of Don Academy Daphne McWilliams Tel: 01224 707583 Fax: 01224 706910 Braehead Way Bridge of Don [email protected] Aberdeen AB22 8RR www.bridgeofdon.aberdeen.sch.uk Braehead School Diane Duncan Tel: 01224 702330 Fax: 01224 707659 Braehead Way Bridge of Don [email protected] Aberdeen AB22 8RR www.braehead.aberdeen.sch.uk Scotstown School Caroline Bain Tel: 01224 703331 Fax: 01224 820289 Scotstown Road Bridge of Don [email protected] Aberdeen AB22 8HH www.scotstown.aberdeen.sch.uk Balmedie School Ken McGowan Tel: 01358 742474 Forsyth Road Balmedie [email protected] Aberdeenshire www.balmedie.aberdeenshire.sch.uk AB23 8YW Schools are listed alphabetically in Associated School Groups. -

Aberdeen Royal Infirmary, Aberdeen, Scotland, United Kingdom
Aberdeen Royal Infirmary, Aberdeen, Scotland, United Kingdom Aberdeen Royal Infirmary opened its doors to its first 4 patients in August 1742, and admitted 21 patients in its first year, tak- ing in people from the Northeast region of Scotland and beyond. The early 1800s saw huge changes take place, including the opening of a dedicated mental health hospital. In 1830, increasing demand on the Infirmary resulted in the construction of the Simpson Pavilion at the Woolmanhill site (top left), accommodating 230 patients. Early cardiology records from 1890 show an unidentified physician diagnosing mitral and aortic stenosis. Aberdeen graduate Augustus Désiré Waller conceptualized and recorded the world’s first ECG in 1887, and the first ECG machine was introduced at Woolmanhill in 1920. The New Aberdeen Royal Infirmary at Foresterhill opened in 1936 (aerial photo, top right), expanding over the last century to become one of the largest hospital complexes in Europe (bottom right). As the main teaching hospital of the University of Aberdeen (world’s fifth-oldest English-speaking University, established 1495), doctors and scientists work closely together in shared facilities. Aberdeen Royal Infirmary is home to many medical discoveries and innovations. In the early 1970s, John Mallard andJim Hutchinson pioneered the design and construction of the world’s first whole body magnetic resonance imaging scanner for clinical use (bottom left). Development of the next generation of the technology (fast field cycling magnetic reso- nance imaging) continues here today. In collaboration with general practitioners, Aberdeen cardiologists pioneered prehospital thrombolysis for acute myocardial infarction in the prepercutaneous intervention era. Dana Dawson, DM, DPhil University of Aberdeen and Aberdeen Royal Infirmary, Scotland Euan Wemyss, BSc (Hons) University of Aberdeen, Scotland. -

Centrepoint Retail Park Aberdeen Ab25 3Sq
NEW LETTING TO CENTREPOINT RETAIL PARK ABERDEEN AB25 3SQ PRIME RETAIL PARK TO THE WEST OF ABERDEEN CITY CENTRE LEASE EXTENSION WITH MECCA 94,376 SQ FT | 8768 SQ M / 600 PARKING SPACES / OPEN PLANNING CONSENT NORTH ELLON A90 G T N 20 MINUTE DRIVE TIME STATS O R CLIFTON RD T NEWMACHAR H E R N R O A D 20 MIN BALMEDIE 20 DRIVE TIME 20 MINUTE DRIVE TIME KITTYBREWSTER P O FOR 250,000 PEOPLE BLACKDOG W RETAIL PARK BLACKBURN DYCE IS T E INVERNESS BACK HILTON RD R R ABERDEEN A C INTERNATIONAL E AIRPORT BEDFORD RD ASHGROVE RD A96 ERSKINE ST ABERDEEN ELMBANK TERRACE POWIS TERRACE A96 58.3% BELMONT RD WESTHILL KINGSWELLS LESLIE TERRACE OF TOTAL HOUSEHOLDS ABERDEEN ARE ABC1 HARBOUR CULTS BIELDSIDE SAINSBURY’S PETERCULTER BERRYDEN ROAD COVE CALSAYSEAT RD POWIS PLACE 42% GEORGE STREET LESLIE TERRACE OF POPULATION AGED AWPR ELM PLACE BETWEEN 20 AND 44 Aberdeen Western YEARS OLD Peripheral Route RAILWAY NETWORK - LINKS TO BERRYDEN ROAD NORTHERN AND CHESNUT ROW SOUTHERN CITIES PORTLETHEN SOUTH A90 BERRYDEN 500,000 LOCATION: RETAIL PARK ABERDEEN’S APPROXIMATE Centrepoint Retail Park is located approximately CATCHMENT POPULATION 1 mile North West of Aberdeen city centre. UNDER OFFER BERRYDEN UNIT 3 RETAIL PARK AVAILABLE 285 6500 SQ FT CAR SPACES CENTREPOINT RETAIL PARK 600 CAR SPACES SAINSBURY’S 276 CAR SPACES SAINSBURY’S [85,000 SQ FT / 7897 SQ M] CENTREPOINT RETAIL PARK [94,376 SQ FT / 8768 SQ M] Mecca Bingo Poundland BERRYDEN RETAIL PARK [73,141 SQ FT / 6795 SQ M] Next Argos Mothercare Currys Contact the joint letting agents to discuss asset management opportunities at Centrepoint. -

EIR-19-1340 - Electric Vehicle Date: 29 October 2019 16:31:17 Attachments: V3 - Further Information - Right to Review & Appeal.Pdf
From: Foi Enquiries To: Subject: EIR-19-1340 - Electric Vehicle Date: 29 October 2019 16:31:17 Attachments: V3 - Further Information - Right to Review & Appeal.pdf Dear Thank you for your information request of 7 October 2019. Aberdeen City Council (ACC) has completed the necessary search for the information requested. Our response is now detailed below. Please could you provide the following details in regards to all Electric Vehicle Charger usage of which your Local Authority Hosts. For the period of 2018 (1/1/18 - 31/12/18) and separately H1 2019 (1/1/19 - 30/6/19). Presented in the following manner. CPS* Number, City/Town, Location, Type, Charging Sessions, Total Kw. For example: 51247 Stonehaven Station Car Park Rapid 50kw 1480 16042.263 51293 Stonehaven Market Square Standard 7Kw 749 4706.44 CPS* Location, City/Town Type Charging Total kWh Number Sessions 50200 Kittybrewster Depot, Aberdeen 7kW double 465 2224.96 50201 Kittybrewster Depot, Aberdeen 7kW double 423 3524.11 50202 Kittybrewster Depot, Aberdeen 7kw/3kW 296 2569.49 combi 50204 Marischal College Car Park, Aberdeen 7kW double 501 2410.08 50205 Marischal College Car Park, Aberdeen 7kW single 261 1299.56 50206 Marischal College Car Park, Aberdeen 7kW single 234 1189.16 50207 Spring Gardens Car Park, Aberdeen 7kW double 7 96.86 50208 Spring Gardens Car Park, Aberdeen 7kW double 183 941.22 50210 Tullos depot 7kW double 0 0 50212 Grove Nursery, Aberdeen 7kW double 205 1071.18 50216 West North Street Car Park, Aberdeen 7kW double 144 1090.75 50340 Sclattie Park Car Park, Aberdeen -

A Directory for the City of Aberdeen
F 71 JljfjjUiLSJL J)....L3. v. 3 %. Digitized by the Internet Archive in 2011 with funding from National Library of Scotland http://www.archive.org/details/directoryforcity183536uns : DIRECTORY CITY OF ABERDEEN 1835-36. 1035$ ABERDEEN Printed by D. CHALMERS & CO. FOR GEO. CLARK & SON, T. SPARK, AND D. WYLLIE & SON. MDCCCXXXV. C?/^ ;£?£-.:£>/*. £p£r43 CONTENTS. Directory, -.,---" 5 Magistrates and Incorporations, - - 180 Alphabetical List of Streets, Squares, &c. - i Carriers, - - , <-. xiii Mail Coaches, ----- xx Stage Coaches, - xxi Shipping Companies, - - - - xxiv Steam Packets, ----- xxv Principal Fairs, - - - - xxvi Post Towns and Postmasters in Scotland, - xxxiii Bridewell Assessment ; Rogue Money ; and King's Subsidy, - - - - - xxxvi Abstract of Population, - ib. List of the Shore Porters, - xxxvii Fire Engine Establishment, - ib. different Parishes in Aberdeen and Old Machar, ----- xxxviii Assessed Tax Tables for Scotland, - - xli Table of Appointments, 1835-36, - - xlvii Stamp Duties, - - - - - xlviii Imperial Weights and Measures, - - xlxix Schedule of Fees, - 1 Weigh-house Dues, - li Petty Customs, - liii Corn Laws, ----- lvii > ABERDEEN DIRECTORY 1835-36. Abel, John., blacksmith, 1, College-lane Peter, coal-broker, 4, Commerce-street Christian, poultry-shop, 76, h. Sutherland's-court, 78, Shiprow Abercrombie, Alexander, merchant, 49, Guestrow Robert, merchant, 49, Guestrow Aberdeen Academy, 115, Union-street Advertiser Office, Lamond's-court, 49, Upperkirkgate Banking Co., 53, Castle-street Brewery, 77, Causewayend, Robert M'Naughton, brewer Brick and Tile Co., Clayhills— Office, 40, Union-street Carpet Warehouse, (Wholesale and Retail,) 1, Lower Dee-street Coach Manufacturing Co., 7, Frederick- street, and 101, King-st. Commercial, Mathematical, and Nautical School, 10, Drum's- lane—W. Elgen Eye and Ear Institution, 7, Littlejohn-st. -

3 Bus Time Schedule & Line Route
3 bus time schedule & line map 3 Cove Bay View In Website Mode The 3 bus line (Cove Bay) has 4 routes. For regular weekdays, their operation hours are: (1) Cove Bay: 4:55 AM - 10:55 PM (2) Mastrick: 5:17 AM - 7:03 PM (3) Rosemount: 8:46 AM - 7:45 PM Use the Moovit App to ƒnd the closest 3 bus station near you and ƒnd out when is the next 3 bus arriving. Direction: Cove Bay 3 bus Time Schedule 50 stops Cove Bay Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday Not Operational Findhorn Road, Mastrick Findhorn Place, Aberdeen Tuesday Not Operational Fernhill Drive, Mastrick Wednesday Not Operational Mastrick Shops, Mastrick Thursday 4:55 AM - 10:55 PM Friday 4:55 AM - 10:55 PM Mastrick Land, Mastrick Mastrick Junction, Aberdeen Saturday 5:10 AM - 10:55 PM Derry Place, Mastrick Arnage Gardens, Aberdeen Derry Avenue, Mastrick 3 bus Info Direction: Cove Bay Long Walk Road, Mastrick Stops: 50 Trip Duration: 51 min Stocket Parade, Stockethill Line Summary: Findhorn Road, Mastrick, Fernhill Drive, Mastrick, Mastrick Shops, Mastrick, Mastrick Oldcroft Terrace, Stockethill Land, Mastrick, Derry Place, Mastrick, Derry Avenue, Foresterhill Road, Aberdeen Mastrick, Long Walk Road, Mastrick, Stocket Parade, Stockethill, Oldcroft Terrace, Stockethill, Ashgrove Ashgrove Place, Stockethill Place, Stockethill, Aberdeen Royal Inƒrmary, Ashgrove Place, Aberdeen Westburn, Foresterhill Health Centre, Westburn, Raeden Avenue, Westburn, Westburn Road, Aberdeen Royal Inƒrmary, Westburn Westburn, Midstocket Road, Midstocket, Hoseƒeld Foresterhill -

Information Governance Medical Directorate NHS Grampian Rosehill House Foresterhill Site Cornhill Road Aberdeen AB25 2ZG
Information Governance Medical Directorate NHS Grampian Rosehill House Foresterhill Site Cornhill Road Aberdeen AB25 2ZG BY EMAIL Date 9 January 2020 Kevin Lawson Our Ref FOI/2020/001 request-631176- Enquiries to Information Governance Team [email protected] Extension 51319 Direct Line 01224 551319 Email [email protected] Dear Mr Lawson Freedom of Information (Scotland) Act 2002 I refer to your e-mail 2 January 2020, requesting: “How many medical staff work at kittybrewster Custody suite , and what are their shifts and duties.” I can now respond as follows: How many medical staff work at kittybrewster Custody suite, and what are their shifts and duties. There are 6 Forensic Physicians. Their shifts are from 6.00am to 6.00am (24 hour shifts) or 12 hours shifts (6.00am - 6.00pm) (6.00pm - 6.00am) The duties are to cover any forensic cases, which includes sexual assault, drug/drink offences and also any general medical services for patients in custody that the nursing team are unable to deal with. Under section 20 (1) of the Act, if you are dissatisfied with the way NHS Grampian has dealt with your request, you have a right to request a review of our actions and decisions in relation to your request, and you have a right to appeal to the Scottish Information Commissioner. A request for review must be made within 40 working days and should, in the first instance, be in writing to: Directorate of Corporate Communications, Foresterhill House, Foresterhill, Aberdeen, AB25 2ZB or by email to [email protected] Requests for appeal can be made by using the Scottish Information Commissioner’s online service at www.itspublicknowledge.info/Appeal or should be made in writing to: Scottish Information Commissioner, Kinburn Castle, Doubledykes Road, St Andrews, Fife, KY16 9DS Telephone: 01334 464610, Fax: 01334 464611. -

3B Bus Time Schedule & Line Route
3B bus time schedule & line map 3B Cove Bay View In Website Mode The 3B bus line Cove Bay has one route. For regular weekdays, their operation hours are: (1) Cove Bay: 7:36 AM Use the Moovit App to ƒnd the closest 3B bus station near you and ƒnd out when is the next 3B bus arriving. Direction: Cove Bay 3B bus Time Schedule 55 stops Cove Bay Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday Not Operational Findhorn Road, Mastrick Findhorn Place, Aberdeen Tuesday Not Operational Fernhill Drive, Mastrick Wednesday Not Operational Mastrick Shops, Mastrick Thursday 7:36 AM Friday 7:36 AM Mastrick Land, Mastrick Mastrick Junction, Aberdeen Saturday Not Operational Derry Place, Mastrick Arnage Gardens, Aberdeen Derry Avenue, Mastrick 3B bus Info Direction: Cove Bay Long Walk Road, Mastrick Stops: 55 Trip Duration: 59 min Stocket Parade, Stockethill Line Summary: Findhorn Road, Mastrick, Fernhill Drive, Mastrick, Mastrick Shops, Mastrick, Mastrick Oldcroft Terrace, Stockethill Land, Mastrick, Derry Place, Mastrick, Derry Avenue, Foresterhill Road, Aberdeen Mastrick, Long Walk Road, Mastrick, Stocket Parade, Stockethill, Oldcroft Terrace, Stockethill, Ashgrove Ashgrove Place, Stockethill Place, Stockethill, Aberdeen Royal Inƒrmary, Ashgrove Place, Aberdeen Westburn, Foresterhill Health Centre, Westburn, Raeden Avenue, Westburn, Westburn Road, Aberdeen Royal Inƒrmary, Westburn Westburn, Midstocket Road, Midstocket, Hoseƒeld Foresterhill Road, Aberdeen Avenue, Midstocket, Hoseƒeld Road, Midstocket, Mile End Lane, Midstocket, Belvidere -
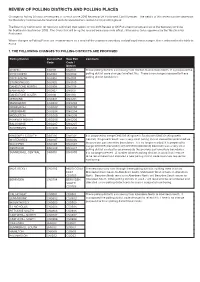
Proposals for Polling Districts and Polling Places
REVIEW OF POLLING DISTRICTS AND POLLING PLACES Changes to Polling Districts are required as a result of the 2018 Review of UK Parliament Consitiuencies. The details of this review can be viewed on the Boundary Commission for Scotland website www.bcomm-scotland.independent.gov.uk The Boundary Commission for Scotland submitted their report for the 2018 Review of UK Parliament Constituencies to the Secretary of State for Scotland in September 2018. The Order that will bring the revised boundaries into effect, still requires to be approved by the estminsterW Parliament. Where changes to Polling Places are recommended as a result of the proposed boundary and polling district changes, this is indicated in the table in Part 2. 1. THE FOLLOWING CHANGES TO POLLING DISTRICTS ARE PROPOSED Polling District Current Poll New Poll Comment Code Code / District KIRKHILL DG0101 DN0101 These polling districts are moving from Gordon to Aberdeen North. It is proposed the DYCE NORTH DG0102 DN0102 polling district code changes to reflect this. There is no change proposed to these polling district boundaries. DYCE SOUTH DG0103 DN0103 STONEYWOOD DG0105 DN0105 DANESTONE NORTH DG0106 DN0106 BANKHEAD DG0107 DN0107 DANESTONE SOUTH DG0110 DN0110 JESMOND DG0201 DN0201 MUNDURNO DG0202 DN0202 NEWBURGH DG0203 DN0203 GREENBRAE DG0204 DN0204 MIDDLETON DG0205 DN0205 PARKWAY NORTH DG0206 DN0206 BALGOWNIE DG0207 DN0207 SILVERBURN DG0208 DN0208 KINGSWELLS SOUTH DS0306 DN0301 It is proposed to merge DN0306 (Kingswells South) with DN0301 (Kingswells WHITEMYRES DN0307 DN0306 Central). Kingswells South was a very small polling district created to accommodate the previous parliamentary boundaries. It is no longer needed. It is proposed to WOODEND DS0308 DN0307 merge DN0309 (Denwood) with DS0308 (Woodend) Denwood was a very small DENWOOD DN0309 DN0307 polling district created to accommodate the previous parliamentary boundaries. -

Early Learning and Childcare Settings in Aberdeen City Listed by Associated School Group (ASG)
Early Learning and Childcare Settings in Aberdeen City Listed by Associated School Group (ASG) ABERDEEN GRAMMAR SCHOOL Local Authority Setting Address Telephone (01224) Ashley Road School 45 Ashley Road 588732 Aberdeen AB10 6RU Gilcomstoun School Skene Street 642722 Aberdeen AB10 1PG Gaelic Nursery @ Skene Street 642722 Gilcomstoun School Aberdeen AB10 1PG Mile End School Midstocket Road 498140 Aberdeen AB15 5LT St Joseph’s RC School 3-5 Queens Road 322730 Aberdeen AB15 4YL Skene Square School 61 Skene Square 630493 Aberdeen AB25 2UN Funded Provider Setting Address Telephone (01224) Albyn School 17-23 Queens Road 322408 Aberdeen AB15 4PB The Bruce Nursery 65 Osborne Place 646836 Aberdeen AB25 2BX Bright Horizons at 24 St 24 St Swithin Street 324555 Swithin Aberdeen AB10 6XD Bright Horizons at 44 St 44 St Swithin Street Swithin Aberdeen AB10 6XJ Great Western Pre-School 356-358 Great Western 311949 Road Aberdeen AB10 6LX Queen’s Cross Nursery Queen’s Cross Church 624721 Albyn Place, Aberdeen AB10 1YN Robert Gordon’s College Schoolhill 646758 Aberdeen AB10 1FE Midstocket Playgroup Rosemount Centre 07752532958 Belgrave Terrace Aberdeen AB25 2NS Summers Nursery 44 Victoria Street 628862 Aberdeen AB10 1XA Summers Nursery 50 St Swithin Street 209966 Aberdeen AB10 6XJ Little Acorns Nursery Royal Cornhill Hospital 557457 (workplace nursery only) 26 Cornhill Road Aberdeen AB25 2ZT The Kindergarten Nursery 196 Westburn Road 633803 Aberdeen AB25 2LT BRIDGE OF DON ACADEMY Local Authority Setting Address Telephone (01224) Braehead School Braehead -

ABERDEEN CITY 03.Indd
Local Government Boundary Commission for Scotland Fourth Statutory Review of Electoral Arrangements Aberdeen City Council Area Report E06001 Report to Scottish Ministers August 2006 Local Government Boundary Commission for Scotland Fourth Statutory Review of Electoral Arrangements Aberdeen City Council Area Constitution of the Commission Chairman: Mr John L Marjoribanks Deputy Chairman: Mr Brian Wilson OBE Commissioners: Professor Hugh M Begg Dr A Glen Mr K McDonald Mr R Millham Report Number E06001 August 2006 Aberdeen City Council Area 1 Local Government Boundary Commission for Scotland 2 Aberdeen City Council Area Fourth Statutory Review of Electoral Arrangements Contents Page Summary Page 7 Part 1 Background Pages 9 – 14 Paragraphs Origin of the Review 1 The Local Governance (Scotland) Act 2004 2 – 4 Commencement of the 2004 Act 5 Directions from Scottish Ministers 6 – 9 Announcement of our Review 10 – 16 General Issues 17 – 18 Defi nition of Electoral Ward Boundaries 19 – 24 Electorate Data used in the Review 25 – 26 Part 2 The Review in Aberdeen City Council Area Pages 15 – 22 Paragraphs Meeting with Aberdeen City Council 1 – 3 Concluded View of the Council 4 – 5 Aggregation of Existing Wards 6 – 11 Initial Proposals 12 – 18 Informing the Council of our Initial Proposals 19 – 20 Aberdeen City Council Response 21 – 24 Consideration of the Council Response to the Initial Proposals 25 – 29 Provisional Proposals 30 – 34 Representations 35 Consideration of Representations 36 – 39 Part 3 Final Recommendation Pages 23 – 24 Appendices Pages -

Dear , Thank You for Your Information Request of 4 April 2017. Aberdeen City Council (ACC) Has Completed the Necessary Search F
From: Foi Enquiries To: Subject: FOI-17-0547 - Council Tax Rates Date: 26 April 2017 14:22:48 Attachments: Further Information - Right to Review & Appeal.pdf FOI-17-0547 - Council Tax Credits Terminated with Prop Address.xlsx Dear , Thank you for your information request of 4 April 2017. Aberdeen City Council (ACC) has completed the necessary search for the information requested. I wish to request data for the new financial year post 1st April 2017. Please can you provide me with the following information under the Freedom Of Information Act 2000:- Please can you provide me with the following information under the Freedom Of Information Act 2000:- All Ctax domestic rate accounts with a credit balance. There are currently no live accounts with credits as the new financial year just started on 1 April 2017. I am aware that all Billing Authorities hold on account sums of money that are due to be returned to council tax payers and for a variety of reasons have not been repaid. I therefore request a breakdown of credit balances accrued since your earliest records, for the amounts owing to all incorporated companies within the authorities billing area, including the following information: A. The name of each business in respect of which council tax credit balances remain payable. I understand you will not provide individuals names. B. The value of overpayment in each case which remains unclaimed C. The years(s) in which overpayment was made (IF KNOWN) D. The property address the credit relates to E. A write to address and write to company name if available F.