Immunology 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(ACIP) General Best Guidance for Immunization
8. Altered Immunocompetence Updates This section incorporates general content from the Infectious Diseases Society of America policy statement, 2013 IDSA Clinical Practice Guideline for Vaccination of the Immunocompromised Host (1), to which CDC provided input in November 2011. The evidence supporting this guidance is based on expert opinion and arrived at by consensus. General Principles Altered immunocompetence, a term often used synonymously with immunosuppression, immunodeficiency, and immunocompromise, can be classified as primary or secondary. Primary immunodeficiencies generally are inherited and include conditions defined by an inherent absence or quantitative deficiency of cellular, humoral, or both components that provide immunity. Examples include congenital immunodeficiency diseases such as X- linked agammaglobulinemia, SCID, and chronic granulomatous disease. Secondary immunodeficiency is acquired and is defined by loss or qualitative deficiency in cellular or humoral immune components that occurs as a result of a disease process or its therapy. Examples of secondary immunodeficiency include HIV infection, hematopoietic malignancies, treatment with radiation, and treatment with immunosuppressive drugs. The degree to which immunosuppressive drugs cause clinically significant immunodeficiency generally is dose related and varies by drug. Primary and secondary immunodeficiencies might include a combination of deficits in both cellular and humoral immunity. Certain conditions like asplenia and chronic renal disease also can cause altered immunocompetence. Determination of altered immunocompetence is important to the vaccine provider because incidence or severity of some vaccine-preventable diseases is higher in persons with altered immunocompetence; therefore, certain vaccines (e.g., inactivated influenza vaccine, pneumococcal vaccines) are recommended specifically for persons with these diseases (2,3). Administration of live vaccines might need to be deferred until immune function has improved. -
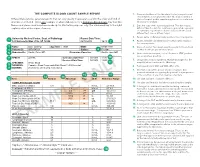
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Asplenia Vaccination Guide
Stanford Health Care Vaccination Subcommitee Revision date 11/308/2018 Functional or Anatomical Asplenia Vaccine Guide I. PURPOSE To outline appropriate vaccines targeting encapsulated bacteria for functionally or anatomically asplenic patients. Routine vaccines that may also be indicated but not addressed here include influenza, Tdap, herpes zoster, HPV, MMR, and varicella.1,2,3 II. Background Functionally or anatomically asplenic patients should be vaccinated to decrease the risk of sepsis due to organisms such as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis. Guidelines are based on CDC recommendations. For additional information, see https://www.cdc.gov/vaccines/schedules/hcp/imz/adult-conditions.html. III. Procedures/Guidelines1,2,3,6,7,8 The regimen consists of 4 vaccines initially, followed by repeat doses as specified: 1. Haemophilus b conjugate (Hib) vaccine (ACTHIB®) IM once if they have not previously received Hib vaccine 2. Pneumococcal conjugate 13-valent (PCV13) vaccine (PREVNAR 13®) IM once • 2nd dose: Pneumococcal polysaccharide 23-valent (PPSV23) vaccine (PNEUMOVAX 23®) SQ/IM once given ≥ 8 weeks later, then 3rd dose as PPSV23 > 5 years later.4 Note: The above is valid for those who have not received any pneumococcal vaccines previously, or those with unknown vaccination history. If already received prior doses of PPSV23: give PCV13 at least 1 year after last PPSV23 dose. 3. Meningococcal conjugate vaccine (MenACWY-CRM, MENVEO®) IM (repeat in ≥ 8 weeks, then every 5 years thereafter) 4. Meningococcal serogroup B vaccine (MenB, BEXSERO®) IM (repeat in ≥ 4 weeks) Timing of vaccination relative to splenectomy: 1. Should be given at least 14 days before splenectomy, if possible. -

Standards of Medical Fitness
Army Regulation 40–501 Medical Services Standards of Medical Fitness Rapid Action Revision (RAR) Issue Date: 23 August 2010 Headquarters Department of the Army Washington, DC 14 December 2007 UNCLASSIFIED SUMMARY of CHANGE AR 40–501 Standards of Medical Fitness This rapid action revision, dated 23 August 2010-- o Clarifies waiver authorities for officer accessions and commissions for the U.S. Military Academy, Reserve Officers’ Training Corps, and Officer Candidate School (paras 1-6c and 1-6e). o Updates the medical retention standards for psychiatric disorders and hearing (paras 3-10 and 3-31). o Adds a requirement for referral to a Medical Evaluation Board for rhabdomyolysis (para 3-40). o Provides new definitions for heat illness and reasons for a Medical Evaluation Board (para 3-45). o Clarifies who has ultimate responsibility to determine whether to deploy a Soldier (para 5-14d, 5-14e, and 5-14f). o Updates deployment-limiting psychiatric medical conditions (para 5-14f(8)). o Updates functional activities to reflect content changes to DA Form 3349, Physical Profile (chap 7). o Requires review of all permanent 3 and 4 profiles by a Medical Evaluation Board physician or other physician approval authority (para 7-4b). o Establishes and defines the term Medical Retention Determination Point (para 7-4b(2)). o Allows physician assistants, nurse practitioners, and nurse midwives to write permanent profiles as the profiling officer (para 7-6a(4)). o Changes administrative code designations for physical profiles (table 7-2). o Adds psychiatric evaluations for certain administrative separations (paras 8-24a(1) and 8-24a(2)). -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -
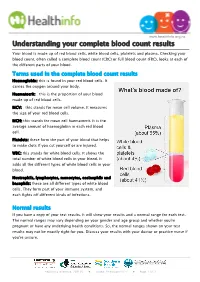
Understanding Your Complete Blood Count Results
www.healthinfo.org.nz Understanding your complete blood count results Your blood is made up of red blood cells, white blood cells, platelets and plasma. Checking your blood count, often called a complete blood count (CBC) or full blood count (FBC), looks at each of the different parts of your blood. Terms used in the complete blood count results Haemoglobin: this is found in your red blood cells. It carries the oxygen around your body. Haematocrit: this is the proportion of your blood made up of red blood cells. MCV: this stands for mean cell volume. It measures the size of your red blood cells. MCH: this stands for mean cell haematocrit. It is the average amount of haemoglobin in each red blood cell. Platelets: these form the part of your blood that helps to make clots if you cut yourself or are injured. WBC: this stands for white blood cells. It shows the total number of white blood cells in your blood. It adds all the different types of white blood cells in your blood. Neutrophils, lymphocytes, monocytes, eosinophils and basophils: these are all different types of white blood cells. They form part of your immune system, and each fights off different kinds of infections. Normal results If you have a copy of your test results, it will show your results and a normal range for each test. The normal ranges may vary depending on your gender and age group and whether you're pregnant or have any underlying health conditions. So, the normal ranges shown on your test results may not be exactly right for you. -
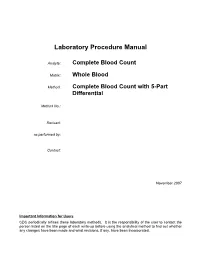
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Complete Blood Count Matrix: Whole Blood Method: Complete Blood Count with 5-Part Differential Method No.: Revised: as performed by: Contact: November 2007 Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: Lab Number Analyte SAS Label LBXWBCSI White blood cell count (SI) LBXLYPCT Lymphocyte (%) LBXMOPCT Monocyte (%) LBXNEPCT Segmented neutrophils (%) LBXEOPCT Eosinophils (%) LBXBAPCT Basophils (%) LBDLYMNO Lymphocyte number LBDMONO Monocyte number LBDNENO Segmented neutrophils number LBDEONO Eosinophils number CBC_d LBDBANO Basophils number LBXRBCSI Red cell count SI LBXHGB Hemoglobin (g/dL) LBXHCT Hematocrit (%) LBXMCVSI Mean cell volume (fL) LBXMCHSI Mean cell hemoglobin (pg) LBXMC MCHC (g/dL) LBXRDW Red cell distribution width (%) LBXPLTSI Platelet count (%) SI LBXMPSI Mean platelet volume (fL) Page 2 of 32 Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 1. Clinical Relevance and Summary of Test Principle Perform a complete blood count (CBC) in duplicate on all Sample Persons (SPs) age 1 and older. Perform the CBC on the Beckman Coulter MAXM. Run a CBC on home exam SP’s EDTA blood tubes after returning to the MEC. A. Purpose and Principle of Test The Beckman Coulter method of sizing and counting particles uses measurable changes in electrical resistance produced by nonconductive particles suspended in an electrolyte. -

Heterotaxy: Associated Conditions and Hospital- Based Prevalence in Newborns Angela E
May/June 2000. Vol. 2 . No. 3 Heterotaxy: Associated conditions and hospital- based prevalence in newborns Angela E. Lin, MD',~,*, Baruch S. Ticho, MD, phD3j4,Kara Houde, MA1,Marie-Noel Westgate, ME^', and Lewis B. Holmes, MD',~,~ Purpose: To provide insight into the possible etiology and prevalence of heterotaxy, we studied conditions associated with heterotaxy in a consecutive hospital population of newborns. Methods: From 1972 to March, 1999 (except February 16, 1972 to December 31, 1978), 58 cases of heterotaxy were ascertained from a cohort of 201,084 births in the ongoing Active Malformation Surveillance Program at the Brigham and Women's Hospital. This registry includes livebirths, stillbirths, and elective abortions. Prevalence among nontransfers (i.e., patients whose mothers had planned delivery at this hospital) was calculated as approximately 1per 10,000 total births (20 of 201,084). Results: We analyzed a total of 58 patients consisting of 20 (34%) nontransfers and 38 (66%) transfers. Patients were categorized by spleen status as having asplenia (7 nontransfers, 25 total), polysplenia (8, 20), right spleen (4, ll),normal left (0, I), and unknown (1, 0). Among the 20 nontransfer and 59 total heterotaxy patients, the following associated medical conditions were present: chromosome abnormality (1nontransfer, 2 total), suspected Mendelian or chromosome microdeletion disorder (1nontransfer, 6 total), and maternal insulin- dependent diabetes mellitus (1 nontransfer, 2 total). There were 6 twins (1 member each from 6 twin pairs including 1dizygous, 4 monozygous, 1conjoined; 2 were nontransfers). An associated condition occurred in 5 (25%) nontransfer and 16 (28%) total patients, or among 10 of 53 singleton births (19%). -
An Unusual Etiology of Cytopenia, Diffuse Lymphadenopathy, and Massive Splenomegaly M
Donald and Barbara Zucker School of Medicine Journal Articles Academic Works 2015 "The Great Mimicker": An Unusual Etiology of Cytopenia, Diffuse Lymphadenopathy, and Massive Splenomegaly M. Zaarour Northwell Health C. Weerasinghe Northwell Health E. Moussaly Northwell Health S. Hussein Northwell Health J. P. Atallah Hofstra Northwell School of Medicine Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Pathology Commons Recommended Citation Zaarour M, Weerasinghe C, Moussaly E, Hussein S, Atallah J. "The Great Mimicker": An Unusual Etiology of Cytopenia, Diffuse Lymphadenopathy, and Massive Splenomegaly. 2015 Jan 01; 2015():Article 683 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/683. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. For more information, please contact [email protected]. Hindawi Publishing Corporation Case Reports in Medicine Volume 2015, Article ID 637965, 6 pages http://dx.doi.org/10.1155/2015/637965 Case Report (The Great Mimicker): An Unusual Etiology of Cytopenia, Diffuse Lymphadenopathy, and Massive Splenomegaly Mazen Zaarour,1 Chanudi Weerasinghe,1 Elias Moussaly,1 Shafinaz Hussein,2 and Jean-Paul Atallah3 1 Department of Medicine, Staten Island University Hospital, North Shore-LIJ Health System, Staten Island, New York, NY 10305, USA 2Department of Pathology, Staten Island University Hospital, North Shore-LIJ Health System, Staten Island, New York, NY 10305, USA 3Division of Hematology and Oncology, Department of Medicine, Staten Island University Hospital, North Shore-LIJ Health System, StatenIsland,NewYork,NY10305,USA Correspondence should be addressed to Mazen Zaarour; [email protected] Received 11 August 2015; Accepted 4 October 2015 Academic Editor: Masahiro Kohzuki Copyright © 2015 Mazen Zaarour et al. -

In Asymptomatic Term Newborns at Risk for Sepsis, Is a Six-Hour CBC a Better Predictor of Sepsis Than a One-Hour CBC?
In asymptomatic term newborns at risk for sepsis, is a six-hour CBC a better predictor of sepsis than a one-hour CBC? Tori Treloar, R.N., B.S.N; Betsy Finley, R.N., B.S.N., M.P.H.; Audrey Nugent, R.N., B.S.N.; Lucy Schoemer, R.N., M.S.N.; Minshan Coudert, R.N., B.S.N. Background Neonatal sepsis is an invasive infection and remains one of the leading causes of Implications for Practice morbidity and mortality among both term and preterm infants (Shah, Padbury, 2014). The evidence is consistent in that well appearing The current practice at Inova Fairfax Medical Campus is to obtain a complete blood neonates at risk for sepsis should not receive a count (CBC) at one hour and again at 12 hours of life on all newborns at risk for sepsis. complete blood count (CBC) until at least six hours At one hour of life, there is normal decreased perfusion to limbs making it difficult to of life. Values obtained at or after six hours are obtain viable blood sample from a newborn. Multiple venous punctures are often more clinically useful as compared to those utilized to obtain the sample which can be distressing to parents and their newborns. obtained immediately after birth. New practice guidelines from CDC and the American Academy of Pediatrics (AAP) The evidence reviewed is consistent across all of support a CBC to be performed at 6-12 hours of life for low-risk, well-appearing the research and provides a compelling indication infants (Merck Manual, 2019).