Ulnar Tunnel Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

Ultrasound of Radial, Ulnar, and Median Nerves
Ultrasound of Radial, Ulnar, Disclosures • Consultant: Bioclinica and Median Nerves • Contractor: POCUS PRO • Advisory Board: Philips Jon A. Jacobson, M.D. • Book Royalties: Elsevier • Not relevant to this lecture Professor of Radiology See www.jacobsonmskus.com for syllabus other educational material Nerve Compression Nerve Entrapment • Experimental model (rat, sciatic nv): • US findings: – Compression causes ischemia – Nerve enlargement proximal to entrapment – First pathologic change: edema • Best appreciated transverse to nerve • Correlated with severity of axonal injury – Abnormally hypoechoic – Mild compression: demyelination • Especially the connective tissue layers – Severe compression: axonal damage – Variable enlargement or flattening at entrapment site Powell, Laboratory Investigation 1986; 55:91 Atrophy Denervation Nerve Entrapment Syndromes • Edema: hyperechoic • Fatty degeneration: • Median: – Hyperechoic – Carpal tunnel syndrome – Echogenic interfaces – Pronator teres syndrome • Atrophy: Asymptomatic – Hyperechoic with • Ulnar: decreased muscle size – Ulnar tunnel syndrome • Compare to other side! – Cubital tunnel syndrome J Ultrasound Med 1993; 2:73 Extensor Muscles: leg 1 Volar Wrist Normal Peripheral Nerve • Ultrasound appearance: – Hypoechoic nerve fascicles – Hyperechoic connective tissue • Transverse: – Honeycomb appearance Silvestri et al. Radiology 1995; 197:291 Median Nerve From: Netter’s Atlas of Human Anatomy Volar Wrist: median nerve & flexors Peripheral Nerves • More coarse compared to tendon T – Fascicular -

Ultrasound of Peripheral Nerve and Muscle
ULTRASOUND OF PERIPHERAL NERVE AND MUSCLE Steven Shook, MD Cleveland Clinic Cleveland, OH INTRODUCTION Advances in field of ultrasound over the past twenty years have generated increasing interest in utilizing the technology in neuromuscular assessment and diagnosis. High-resolution ultrasound offers a noninvasive, real- time, static and dynamic examination of the peripheral nervous system, yielding information which complements the neurological examination, electrodiagnostic testing (EDX), and other established imaging modalities such as Magnetic Resonance Imaging (MRI). ULTRASOUND BASICS Ultrasonography involves transmitting sound-wave pulses into tissue and analyzing the temporal and acoustic properties of the reflected wave, or echo. Echoes occur at tissue interfaces. Reflected energy is a product of the difference in adjacent tissue densities (acoustic impedance), as well the angle of the ultrasound beam (angle of incidence) relative to the interface.(1) A fraction of a transmitted sound-wave energy is reflected whenever there is a change in acoustic impedance within tissue. Larger differences in acoustic impedance result in more profound reflection. Unreflected sound travels deeper into the tissue, generating echos from layers at a greater depth. A portion of the ultrasound energy never returns to the transducer, either being transformed into heat (absorption), refracted or scattered at nonperpendicular tissue interfaces. When the sound wave encounters a significantly different tissue density, analysis of deeper structures is not possible. For example, ultrasound cannot evaluate structures deep to air- filled cavities or bone due to the acoustic impedance of these regions.(2) An ultrasound probe (transducer) is capable of both emitting and receiving these pulses and converting them into electrical signals for analysis. -

Articulationes Membri Thoracici • 1. Articulatio
ARTICULATIONES MEMBRI THORACICI • 1. ARTICULATIO HUMERI-art. simplex, art. spheroidea (but functions as a hinge joint) movement: eq, Ru only flexion, extension is possible, in ca: rotation, abduction, adduction also between scapula (cavitas glenoidalis) and humerus (caput) Capsula articularis Recessus: cranial and caudal recesses Labrum glenoidale Ligg. glenohumeralia (eq, ca)- tickened part of the capsule (capsular ligament) in the med. and lat. walls in ca, and cranially in eq Lig. coracohumerale (eq, Ru)- capsular ligament between scapula (tub. supraglenoidale) and humerus (tub. majus, minus) No collateral ligaments! Instead of them: laterally m. infraspinatus (1), medially m. subscapularis (5) ca: part of the joint capsule surrounds the tendon of m. biceps brachii (9) and forms vagina synovialis intertubercularis eq, bo: bursa intertubercularis (=bursa bicipitalis) under the tendor of the m. biceps brachii (may communicate with the joint cavity of the shoulder joint in horse) • 2.ARTICULATIO CUBITI-art. composita, ginglymus (hinge joint) movement: extension and flexion between humerus (condyle), radius (caput), ulna (insisura trochlearis) Articulatio humeroulnaris Articulatio humeroradialis Capsula articularis Recessus: recessus cranialis, large recessus caudalis Lig. collaterale cubiti mediale- from epicondylus med. to radius (in ca also to ulna) Lig. collaterale cubiti laterale- from epicondylus lat. to radius (in ca, Ru also to ulna) Lig. olecrani (ca)- capsular ligament from fossa olecrani of humerus to olecranon •3. ARTICULATIO RADIOULNARIS PROXIMALIS- art. simplex, art. trochoidea movement: ca: rotational movements are possible (pronatio, supinatio) eq, Ru: no movement! between radius (circumferentia articularis radii) and ulna (incisura radialis ulnae) Lig. anulare radii (ca)- encircles the head of the radius, running under the collateral ligaments Membrana interossea antebrachii (ca) (in eq, Ru it is ossified) • 4. -
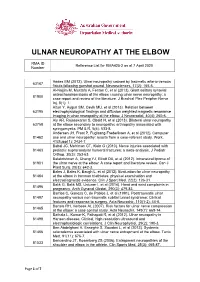
Reference List for RMA425-2 As at 7 April 2020 Number
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014). -

COVID-19 Mrna Pfizer- Biontech Vaccine Analysis Print
COVID-19 mRNA Pfizer- BioNTech Vaccine Analysis Print All UK spontaneous reports received between 9/12/20 and 22/09/21 for mRNA Pfizer/BioNTech vaccine. A report of a suspected ADR to the Yellow Card scheme does not necessarily mean that it was caused by the vaccine, only that the reporter has a suspicion it may have. Underlying or previously undiagnosed illness unrelated to vaccination can also be factors in such reports. The relative number and nature of reports should therefore not be used to compare the safety of the different vaccines. All reports are kept under continual review in order to identify possible new risks. Report Run Date: 24-Sep-2021, Page 1 Case Series Drug Analysis Print Name: COVID-19 mRNA Pfizer- BioNTech vaccine analysis print Report Run Date: 24-Sep-2021 Data Lock Date: 22-Sep-2021 18:30:09 MedDRA Version: MedDRA 24.0 Reaction Name Total Fatal Blood disorders Anaemia deficiencies Anaemia folate deficiency 1 0 Anaemia vitamin B12 deficiency 2 0 Deficiency anaemia 1 0 Iron deficiency anaemia 6 0 Anaemias NEC Anaemia 97 0 Anaemia macrocytic 1 0 Anaemia megaloblastic 1 0 Autoimmune anaemia 2 0 Blood loss anaemia 1 0 Microcytic anaemia 1 0 Anaemias haemolytic NEC Coombs negative haemolytic anaemia 1 0 Haemolytic anaemia 6 0 Anaemias haemolytic immune Autoimmune haemolytic anaemia 9 0 Anaemias haemolytic mechanical factor Microangiopathic haemolytic anaemia 1 0 Bleeding tendencies Haemorrhagic diathesis 1 0 Increased tendency to bruise 35 0 Spontaneous haematoma 2 0 Coagulation factor deficiencies Acquired haemophilia -

Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know
Anaesthesia & Critical Care Medicine Journal ISSN: 2577-4301 Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know Kamel I* and Huck E Review Article Lewis Katz School of Medicine at Temple University, USA Volume 4 Issue 3 Received Date: June 20, 2019 *Corresponding author: Ihab Kamel, Lewis Katz School of Medicine at Temple Published Date: August 01, 2019 University, MEHP 3401 N. Broad street, 3rd floor outpatient building ( Zone-B), DOI: 10.23880/accmj-16000155 Philadelphia, United States, Tel: 2158066599; Email: [email protected] Abstract Peripheral nerve injury is a rare but significant perioperative complication. Despite a variety of investigations that include observational, experimental, human cadaveric and animal studies, we have an incomplete understanding of the etiology of PPNI and the means to prevent it. In this article we reviewed current knowledge pertinent to perioperative upper extremity peripheral nerve injury and optimal intraoperative patient positioning. Keywords: Nerve Fibers; Proprioception; Perineurium; Epineurium; Endoneurium; Neurapraxia; Ulnar Neuropathy Abbreviations: PPNI: Perioperative Peripheral Nerve 2018.The most common perioperative peripheral nerve Injury; MAP: Mean Arterial Pressure; ASA CCP: American injuries involve the upper extremity with ulnar Society of Anesthesiology Closed Claims Project; SSEP: neuropathy and brachial plexus injury being the most Somato Sensory Evoked Potentials frequent [3,4]. In this article we review upper extremity PPNI with regards to anatomy and physiology, Introduction mechanisms of injury, risk factors, and prevention of upper extremity PPNI. Perioperative peripheral nerve injury (PPNI) is a rare complication with a reported incidence of 0.03-0.1% [1,2]. Anatomy and Physiology of Peripheral PPNI is a significant source of patient disability and is the Nerves second most common cause of anesthesia malpractice claims [3,4]. -

Electrophysiological Features of Ulnar Tunnel Syndrome Caused By
hysical M f P ed l o ic a in n r e International Journal of Physical u & o R J l e a h n a Nobuta et al., Int J Phys Med Rehabil 2018, 6:6 b o i t i l i a ISSN: 2329-9096t a n r Medicine & Rehabilitation DOI: 10.4172/2329-9096.1000494 t i e o t n n I Research Article Open Access Electrophysiological Features of Ulnar Tunnel Syndrome Caused by Ganglion–A Descriptive Study Shingo Nobuta1*, Kazuaki Sonofuchi2 and Eiji Itoi3 1Department of Orthopaedic Surgery, Tohoku Rosai Hospital, Sendai, Japan 2Goto Orthopaedic Clinic, Sendai, Japan 3Department of Orthopaedic Surgery, Tohoku University School of Medicine, Sendai, Japan *Corresponding author: Shingo Nobuta, MD, PhD, Department of Orthopaedic Surgery, Tohoku Rosai Hospital 4-3-21 Dainohara, Aoba-ku, Sendai, Miyagi 981-8563, Japan, Tel: +81-22-275-1111; Fax: +81-22-275-7541; E mail : [email protected] Received date: October 31, 2018; Accepted date: November 20, 2018; Published date: November 22, 2018 Copyright: ©2018 Nobuta S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Objective: Ulnar tunnel syndrome (UTS) is an uncommon ulnar neuropathy. Clinical and electrophysiological diagnosis of UTS is difficult. The purposes of this study were to assess the diagnostic value of the nerve conduction measurements for UTS caused by ganglion, and to investigate the electrophysiological features of UTS. -

Skeleton of Hand Skeleton of the Hand with Bone Numbering Skeleton Of
Info 6001 Sliding joints at the shoulder allow all natural movements. 6008 Skeleton of hand True to life casting of a skeleton of the human hand. All hand bones are individual- ly mobile-mounted on wire. Ref.no. 6001 With stand Ref.no. 6001S (see image below) 6016 6021 Skeleton of the hand with bone numbering Model as 6001, but with additional numbe- Skeleton of arm with shoulder Skeleton of arm with shoulder ring of the individual hand bones. girdle girdle and muscle marking Ref.no. 6002 (not pictured) True to life casting of a skeleton of the True to life casting of a skeleton of the human arm. The rolling movements of the human arm. The rolling movements of the bones of the lower arm (pronation and bones of the lower arm (pronation and supination) and movements of the hand supination) and movements of the hand Hand with lower arm joint can be demonstrated. The hand is joint can be demonstrated. The hand is True to life casting of a skeleton of the mobilemounted on wire. mobile-mounted on wire. Including marking human hand. All hand bones are individual- Ref.no. 6016 of muscle origins and insertion points. ly mobile-mounted on wire. With radius and Ref.no. 6021 ulna. The rolling movements of the bones Skeleton of arm of the lower arm (pronation and supinati- Model as 6016, but without shoulder girdle. on) and movements of the hand joint can Ref.no. 6012 Skeleton of arm with muscle be demonstrated. marking Ref.no. 6008 Model as 6021, but without shoulder girdle Ref.no. -

Cubital Tunnel Syndrome Guidance
CUBITAL TUNNEL SYNDROME GUIDANCE Author Louise Ross ([email protected]) Organisation NHS Greater Glasgow and Clyde Created 15/04/2016 15:32:54 Modified 26/10/2016 16:17:15 Modified By Louise Ross This pathway can be viewed at http://www.ckp.scot.nhs.uk/Published/Viewer.aspx?id=1743 Copyright © NHS Greater Glasgow and Clyde 2012. All rights reserved Cubital Tunnel Syndrome Guidance Author: Louise Ross CUBITAL TUNNEL SYNDROME GUIDANCE AHP Exit/ Parallel Serious Red Flags Routes Pathology Cubital Tunnel Syndrome Post Operatively Mild - Moderate Signs Moderate - Severe Signs and and Symptoms Symptoms 1st Line Management Place on hold/ Review in 6/52 Discharge Escalate 2nd Line Management Review Discharge Escalate Surgical Opinion/ List for surgery Post Operative Key More Infomation Decision Discharge Intervention Red Flag Self-Management Default Page 1/9 Cubital Tunnel Syndrome Guidance Author: Louise Ross GENERAL RELATED INFORMATION FOR PATHWAY Copyright Information Copyright © NHS Greater Glasgow and Clyde, 2013-2016, All rights reserved Page 2/9 Cubital Tunnel Syndrome Guidance Author: Louise Ross SPECIFIC RELATED INFORMATION FOR PATHWAY SECTIONS RED FLAGS Pathways Related pathway: MSK Foot and Ankle Red Flags NHSGGC SERIOUS PATHOLOGY Pathways Related pathway: Serious Pathology AHP EXIT/ PARALLEL ROUTES Pathways Related pathway: exit routes x 6 CUBITAL TUNNEL SYNDROME Information Description Cubital tunnel syndrome occurs due to compression of the ulnar nerve at the elbow. It is the second most common nerve compression and causes para/anaesthesia of the little and ulnar half of the ring finger with weakness of small muscles of the hand and/or the thumb. -

Peripheral Nerve Disorders
CLINICAL GUIDELINES PND Imaging Policy Version 1.0 Effective February 14, 2020 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies: This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2017 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2019 eviCore healthcare. All rights reserved. PND Imaging Guidelines V1.0 Peripheral Nerve Disorders (PND) Imaging Guidelines Abbreviations for Peripheral Nerve Disorders Imaging Guidelines 3 PN-1: General Guidelines 4 PN-2: Focal Neuropathy 5 PN-3: Polyneuropathy 7 PN-4: Brachial Plexus 8 PN-5: Lumbar and Lumbosacral Plexus 9 PN-6: Muscle Disorders 10 PN-7: Magnetic Resonance Neurography (MRN) 13 PN-8: Amyotrophic Lateral Sclerosis (ALS) 14 PN-9: Peripheral Nerve Sheath Tumors (PNST) 15 PN-10: Nuclear Imaging 16 ______________________________________________________________________________________________________ -

Fractures of Hamate: a Clinical Overview
MUSCULOSKELETAL SURGERY (2019) 103:15–21 https://doi.org/10.1007/s12306-018-0543-y REVIEW Fractures of hamate: a clinical overview G. Mouzopoulos1 · C. Vlachos1 · L. Karantzalis1 · K. Vlachos1 Received: 28 June 2017 / Accepted: 20 May 2018 / Published online: 29 May 2018 © Istituto Ortopedico Rizzoli 2018 Abstract Hamate fractures are exceedingly rare clinical entities. However, the diagnosis and treatment of these injuries are often delayed and can severely handicap the performance of afected laborers or athletes. This review focuses on fractures of the hamate and provides an update on the current consensus as to mechanism, diagnosis, management, and complications after such injuries. Keywords Hamate · Hook · Fracture Epidemiology the hook of the hamate [2]. If the grip is relaxed or control is lost, the fracture occurs at the end of a poor swing, as Fractures of the hamate usually occur through the hook centrifugal force is transmitted through the handle of the or body of the bone [1]. Type I fractures involve the hook racquet against the hook [7]. In golfers or baseball players, of the hamate and further are subdivided into three sub- a dubbed shot or a checked swing will fracture the hamulus types involving: base, waist, and avulsion (tip). Fractures because the butt of the club or bat will strike the hook. It has located at the base and proximal third (76%) of the hook also been described in polo and ice hockey [8]. are presented more frequently than fractures located at the Fall on an outstretched hand causing sudden forcible mid-third (13%) or the distal third (11%).