A Typhoid Fever Outbreak in a Slum of South Dumdum Municipality, West
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The 2 Train Journeys of India
Some dishes contain bones, nuts, seeds, gluten, lactose, soya sauce and food colouring. Please inform a member of staff of any dietary requirements or allergies you may have. All dishes are made with natural heat and aroma from Indian spice we are social blends. Each dish has an individual flavour and spice profile. Like, follow and share us Hints of Spice @PatriArtisan / PatriRestaurant GF: Gluten Free VG : Vegan The 2 Train Full Heat with Spice Undertone V : Vegetarian ORDERING GUIDE N : Nuts Intense Spice and Chilli Step 1. Choose your city New Delhi or CALCUTTA order left to right * Moreish - Order 1 dish each from Street Food and Classic. Food Memories journeys ** Hungry - Order 1 dish each from Street Food, Classic and Signature with one extra. Vegan Vegetarian Nuts City Specials *** Very Hungry - Order 1 each from Street Food, Classic, Pairing and two extras. Our food is prepared to authentic Indian Spice Levels and comes as soon as its ready in no particular order. OF INDIa 30.Masala Iced Karma Soda 4.50 East meets West in this dark refreshing Signature Pairing drink made using organic cola mixed Street FoodSmall Plates Grills & More for 2-3 MasterChef Curries for 2-3 with Grills or Curries with tangy chaat masala and black salt for a unforgettable love me tease Classics me twist of favours 1. Old Delhi Pani Puri (4 pcs) 4.95 7. Nawabi Seekh Kabab (3pcs) 6.50 13. Pantry Chicken Curry (GF ) 10.95 21. Bedmi Aloo (VEGAN/ GF) 6.95 Bombs (6 pcs) 6.50 (GF) (4pcs) 8.50 A simple preparation of onions, tomatoes The quintessential roadside curry for the soul, नई दिल्ली स्टेशन cooked fast and furious style inspired by the 31.Nimbu Lemon Soda 4.50 Crispy wheat(VEGAN) balls filled with chick peas and Medium triple minced skewers marinated using spicy and tangy potato curry reduced in a tango chef’s secret spice and herb mix, cooked over moving express trains and simmered with tomato masala and coriander. -

Wonder Cook Book
Cook Book Forward What is the single most important tool to win hearts…world over? Great cookery skills! With this talent, it’s easier to make friends, the kids don’t fuss over food, the guests are mighty impressed, and you become a VVIP during festivals and social gatherings! Wonder Cook Recipe Book is the celebration of 50 extraordinary cooks and their 50 extraordinarily delicious recipes. Most of these cooks have watched a lot of cookery shows and referred to countless recipe books. But not in their wildest dreams, did they imagine having their own cook book published. Wonder Cook Recipe Book is a dream come true for these gifted cooks. Find 50 mouth-watering recipes handpicked by none other than Celebrity Chef, Sanjeev Kapoor. Make sure you try each one of them and win accolades from your family and friends. “Cooking is love made visible” PS: ‘Wonder Cook’ was a culinary contest organised by AEGON Religare Life Insurance Limited. From over many hundreds of recipes received, 50 top recipes were handpicked by Mr. Sanjeev Kapoor and published through Wonder Cook Recipe book. Index Sr. No. Recipe Page No. Sr. No. Recipe Page No. 01 Bharwa Karela ka Naya Andaaz .................01 27 Bitter Gourd Prawn Masala Fry..................27 02 Chunka Pitha with Chutney ......................02 28 Eggplant Parmesan................................28 03 Wonder Moong Balls...............................03 29 Degchi Biryani .....................................29 04 Kol Posola Mansho 30 Farra with Sukhe Aloo and (Banana Stem with Chicken) ....................04 -

LUNCH MENU (11 Am to 3 Pm)
OH INDIA 15600 NE 8TH Street, Suite O-09 Bellevue, WA 98008 www.ohindiarestaurant.com [email protected] LUNCH MENU (11 am to 3 pm) THALIS Veg Thali $10.00 (Any 3 Veg Entrees + Daal + Rice + Naan / Roti + Papad + Sweet) Paneer Butter Masala Palak Paneer Kadhai Veggies Channa Masala Veggie of the Day Non-Veg Thali $12.00 (Any 3 Non-Veg Entrees + Daal + Rice + Naan / Roti + Papad + Sweet) Butter Chicken Chicken Khorma Chicken Dish of the day Lamb Tikka Masala Lamb Khorma Mixed Thali $11.00 (Any 2 Veg Entrees + 1 Non-Veg Entrée + Daal + Rice + Naan / Roti + Papad + Sweet) Butter Chicken Chicken Khorma Chicken Dish of the day Lamb Tikka Masala Lamb Khorma (replace Butter Naan / Tandoori Roti with Garlic Naan – add $1.00) KATHI ROLLS A delicious Indian Wrap originating in Kolkata, consisting of a flaky Laccha Paratha Bread layered with beaten eggs (optional), stuffed with marinated grilled Paneer {Indian Cottage Cheese} / Chicken / Lamb and garnished with lime juice, special blend of spices & sauces Paneer Roll $ 8.00 Chicken Roll $ 8.00 Lamb Roll $ 8.00 DESI BURGERS (served with Oh India Masala Fries) Spicy Paneer Burger $6.00 (Crumb Fried Paneer marinated in Indian spices along with melted cheese and spices served in a soft burger bun) Crispy Chilly Chicken Burger $6.00 (Crispy fried chicken breast marinated in Indian spices for that special zing, served in a soft burger bun) BIRYANI Biryani (Chicken / Goat) $12.00/13.00 (Special long grained basmati rice cooked with marinated tender bone in chicken / goat meat in layers and served -

Exploring the Popular Culture of Street Food: CASS a Journey Into the World of Taste
UGC Approval No:40934 CASS-ISSN:2581-6403 Exploring the Popular Culture of Street food: CASS A Journey into the World of Taste Amritha Vydoori S P Research Scholar, Dept. of English, University of Calicut Address for Correspondence: [email protected] ABSTRACT: Food, one of the most essential necessities of human life often tells the story of human history, its culture, economic and social conditions. Food is a marker of class and an instrument of socialization. Eating together plays a great role in building up human relations and spreading the culture of taste. Street food that are usually sold on the streets by hawkers and vendors in portable stalls and carts is one of the much sought after choice among the current generation. Street food culture is closely linked with road travels and has become a fashion statement for the riders who are on a mission to discover new tastes and to get in touch with unfamiliar places. India with its rich culinary tradition and diverse cuisine offers a wide range of tastes that stirs the appetite of a food lover. Arevival of the traditional food that caters to the needs of the modern taste is noticeable in such small streetshops and this enables the passing on of dietary wisdom from generation to generation. However, the migratory flows in this globalized era has brought about a mixing of cuisines and tastes too. A coexistence of tastes; old and new is the highlight of such food points.The finger-licking good food provided in the streets are often a mélange of exotic spices and ingredients that satisfy our olfactory senses too. -
Master Menu Sushil Ji
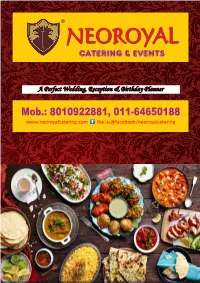
® NEORONEOROYYALAL CATERING & EVENTS A Perfect Wedding, Reception & Birthday Planner Mob.: 8010922881, 011-64650188 www.neoroyalcatering.com like us@facebook/neoroyalcatering MENU APPETIZERS Tidbit's to start with all kinds of mouth watering delicacies BEVERAGES Aerated Drinks and Mock tails to mesmerize you soul SALADS & ACCOMPANIMENTS Ornamental Platters of Fresh cut gourds and Fruits with mouth Freshening condiments MAIN COURSE Cuisines from All Corners of India and Asia to fulfill your foodie inside DESERTS & SWEETS A Sweet end to your food journey, may the sweetness remains. WELCOME DRINKS BEVERAGES Assorted Cold Drinks / ,lksVsZM dksYM fMªaDl Aam Panna / vke iUUkk Badam Milk / cknke feYd Kadhai Milk / d<+kbZ feYd Jal Jeera / ty thjk Roohafza / :gvQtk Lassi – Sweet and Salty / yLlh & LohV ,.M lkYVh Hot Coffee / gkWV dkWQh Kulhad Chai / dqYyM pk; Masala Tea / elkyk pk; Ginger Tea / ftatj pk; Elaichi Tea / byk;ph pk; Cappuccino / dSisphuks Espresso Coffee / ,Lizslks dkWQh Black Tea / Cysd pk; Lime Tea / ykbZe pk; Mock Tails / eksdVsYl APPETIZERS & SNACKS VEG PANEER TIKKA AJWAINI / iuhj fVDdk vtokbuh TANDOORI ALOO / ranwjh vkyw ALOO DILNAZ / vkyw fnyukt PANEER KARARA / iuhj djkjk PANEER TIKKA HARYALI / iuhj fVDdk gfj;kyh SEASME TOAST / lhles VksLV SPRING ROLL / fLizax jksy DRY CHILLI POTATOES / MªkbZ fpYyh iksVsVksl HONEY CHILLI POTATO / gUuh fpYyh iksVsVksl DRY MANCHURIAN / MªkbZ eUpwfj;u MASALA CHEESE FINGER / elkyk pht fQaxj SCHEZWAN CHILLY PANEER / lstoku fpYyh iuhj GOLDEN FRIED BABY CORN / xksYMu QzkbZM csch dksuZ BABY CORN CHEESE -

Dr. Eusebio Pires (EZ) and Dr
Dr. Eusebio Pires (EZ) and Dr. Mahabuba Akhter Lorna Sundberg International Center of UVA. Saturday, 14th May 2011 Bangladesh and India are part of the Indian Subcontinent and have had a long common cultural, economic and political history. The cultures of the two countries are similar; in particular Bangladesh and India's states West Bengal and Tripura are all Bengali- speaking. However, since the partition of India in 1947, Bangladesh (formerly East Bengal and East Pakistan) became a part of Pakistan. Following the bloody Liberation War of 1971, Bangladesh gained its independence and established relations with India. The political relationship between India and Bangladesh has passed through cycles of hiccups. According to Bangla fundamentalists: 'A Bengali Hindu is culturally closer to a Bangladeshi Muslim, yet they are supposed to be "foreigners" to each other' they believe in Hindu-Muslim Bhai Bhai, which means that Bangladeshi Hindu-Muslims are brothers. Bangla cuisine refers to the Bengali cuisine prevalent in Bangladesh. The Bangladeshi cuisine incorporates many Persian-Arabic elements and the usage of meat greatly sets it apart from the cuisine in West Bengal in India. It also has considerable regional variations. A staple across the country however is rice, various kinds of lentil, which is locally known as dal & fresh waster fish is also eaten regularly. Bangladeshi food varies between very 'sweet' and mild-to extremely spicy, many tourists even from other South East Asian and Sub continental countries find the food spicy. It resembles North East Indian and South East Asian food more closely than that of any other part of the Subcontinent, most probably due to geographic and cultural proximity. -

Bacterial Load and Multi-Drug Resistance Patterns of Some Ready-To-Eat Street Foods of Dhaka City
Dhaka Univ. J. Biol. Sci. 27(1): 27-36, 2018 (January) BACTERIAL LOAD AND MULTI-DRUG RESISTANCE PATTERNS OF SOME READY-TO-EAT STREET FOODS OF DHAKA CITY MIHIR LAL SAHA*, MIST. DILARA AKTER, TAHSIN KHAN, ANEESA ANSARI AND MOHAMMAD NURUL ISLAM Department of Botany, University of Dhaka, Dhaka- 1000, Bangladesh Key words: Bacterial load, RTE street foods, Coliform bacteria, MDR, MAR index Abstract Bacterial load and drug resistance pattern associated with some ready-to-eat (RTE) street foods such as Chatpoti, Fuchka, Singara, Panipuri, Ghugni-muri, Chola and water of Dhaka South City Corporation were investigated. Most of the samples were found to be contaminated and the bacterial load ranged from 2.4 × 104 - 9.2 × 106, 1.2 × 103 - 7.3 × 105 and 1.1 × 103 - 1.6 × 106 cfu/g of aerobic heterotrophic, coliform bacteria and Staphylococcus, respectively. The highest coliform load (7.3 × 105 cfu/ml) was found in the water of Gulistan. The highest aerobic heterotrophic bacteria (9.2 × 106 cfu/g) and Staphylococcus (1.6 × 106 cfu/g) were observed in the Chatpoti of Nilkhet. Among the isolated 100 different bacterial colonies, 20 Gram-positive and 8 Gram-negative isolates were studied in details. Based on the morphological and biochemical analysis, the Gram- positive isolates were identified as Staphylococcus (9), Bacillus (4), Kurthia (3), Planococcus (1), Micrococcus (1), Listeria (1) and Renibacterium (1). Gram-negative isolates were identified as Klebsiella pneumoniae (3), Yersinia pestis (1), Y. pseudotuberculosis (1), Escherichia coli (1), Enterobacter aerogenes (1) and Plesiomonas shigelloides (1). The multi-drug resistance (MDR) pattern was found to be diverse. -

Dear Patron, the Journey of Masala Library by Jiggs Kalra Has Been an Exciting One
dear patron, the journey of masala library by jiggs kalra has been an exciting one. when we first started the flagship in october 2013 in mumbai, we did not know how the patrons would react; but within a week our apprehensions were laid to rest. since then it has received adulation from our patrons and worldwide critics alike. the new masala library by jiggs kalra, has been termed version 4.0 because of its significant leap in vision and technique. it is a true gastronomic journey through india and the subcontinent. our chefs have travelled all across the country, including the north-east, to research the local cuisine and the myriad of ancient techniques that exist across this great landscape. we have incorporated post-modern and post-molecular techniques fused with these ancient methods, to create an experience that is perhaps a world first. we have devoted over a year in research and extensive food trials to come up with this menu. chef saurabh udinia, the team and i, have tried to ensure a comprehensive representation of the culinary legacy of the indian subcontinent through this menu. we have invested our passion, marrying it with our love for the cuisine - all under the mentorship of mr. jiggs kalra. the finest way to experience masala library by jiggs kalra is through the chef’s tasting menu. we suggest you surrender yourselves to our finest selection of dishes in the 12 course signature menu. despite the number of courses, it has been carefully designed to make you feel optimally satiated at the end of the experience. -

To Health, Nutrition, and Diabetes Indian Foods: AAPI's Guide
Indian Foods: AAPI’s Guide To Health, Nutrition, and Diabetes © American Association of Physicians of Indian Origin Photographs by Amish Thakkar; Cover page designed by Ranjita Misra Indian Foods: AAPI’s Guide To Nutrition, Health and Diabetes By The Subcommittee of the Public Health Committee of AAPI Nirmala Abraham Theja Mahalingaiah Padmini Balagopal Suraj Mathema Rita (Shah) Batheja Ranjita Misra Nimesh Bhargava Chhaya Patel Sharmila Chatterjee Sudha Raj Keya Deshpande Nirmala Ramasubramanian Madhu Gadia Janaki Sengupta Karmeen Kulkarni Geeta Sikand Allied Publishers Private Limited New Delhi l Mumbai l Kolkata l Chennai l Nagpur Ahmedabad l Bangalore l Hyderabad l Lucknow ! ! "#$%&'()*!+!,--,!.%!//01! ! /22!&'()*3!&434&5467!8&'**49!$4&:'33'#9!:;3*!.4!34<;&46! =&#:!//01!*#!;34!#&!&4$<4!>9%!$>&*!#=!*)'3!.##?24*7! 0;.2'3)46!'9!")499>'@!196'>!.%!/22'46!0;.2'3)4&3@!05*7!A*67!! >96!6'3*&'.;*46!.%!//01@!BC/! ! ! ! ! !"#$%&'())*+(,-.(&% ! ! ! ! !"#$#%&'(")*+,* /:'3)!D)>??>&! ! -#./&*('%/*0/)1%2/0*+,* E>9F'*>!G'3&>! ! ! ! ! ! ! !&12$/0*'$* ")499>'!G'<&#!0&'9*!H0I!A*67! ")499>!J!,K7! ! ! ! ! ! !3+41)"/0*+,* "/0/%"123456! G>9>('9(!L'&4<*#&! 788954%:;<89=35>=%:6?/%@?4/! MNO@!/99>!C>2>'@!")499>'!P--!--,! ! ! ! ! D)4!/:4&'<>9!/33#<'>*'#9!#=!0)%3'<'>93!#=!196'>9!Q&'('9!H//01I! OM8!R--!,,96!C*&44*@!C;'*4!R--/@! Q>?.&##?!D4&&><4@!1A!P-OSOJTTK-@!B7C7/! CONTENTS "#$%&'$! (! )'*+,-.$/0$1$+23! (44! 5,#$-,#/! 46! 7+2#,/8'24,+! !!!"#$%&'%(!)$*&'*!9! :$!;43$&3$! !!+,,-%&!./%0#&12&'*&32*2&4*5!<! =,#2>!7+/4&+!?8434+$! !!1%#$"&+%#.%&1!&'*&4*5!@! =$A&.4!?8434+$! -

IISERBPR/Cosa/EOI/Mess Catering/2018-19/02 June 01, 2018
IISERBPR/CoSA/EOI/Mess Catering/2018-19/02 June 01, 2018 EXPRESSION OF INTEREST FOR PROVIDING MESS CATERING SERVICES AT IISER BERHAMPUR Expression of Interest (EOI) is invited from the Mess vendors/Caterers of repute to run the mess of Students’ Mess Committee, IISER Berhampur situated at Berhampur, District Ganjam, Odisha, Pin-760010. The mess will run on cooperative basis by the students. Institute will provide space and necessary infrastructure facilities. EOI is solicited for selection of mess service providers. 1. About Students’ Mess Committee. Committee is elected/selected by hostel residents of IISER Berhampur that manages and monitors the running of the hostel mess, on behalf of the residents. It consists of students’ representatives and it works under the supervision of the Warden-In- Charge. The mess is run on contributory basis by the user, i.e. the students. The Committee is in the process of selecting a catering contractor for Mess at, Boy’s Hostels and Girl’s Hostels, at one place with distribution points. The facility consists of a kitchen and a dining hall. The caterer who is awarded the contract is also expected to run the cafeteria cum canteen under the mess premises. 2. Eligibility Criteria: a) The bids should be sent to the committee in two separate sealed envelopes labeled Technical Bid” and “Financial Bid” respectively. The two envelopes should be put inside a bigger envelope labeled EXPRESSION OF INTEREST FOR MESS at Boy’s Hostels and Girl’s Hostels, of IISER Berhampur. The Technical Bid will contain your application along with all the documents in the prescribed format listed below. -
AAPI's Guide to Nutrition, Health and Diabetes
Indian Foods: AAPI’s Guide To Nutrition, Health and Diabetes SECOND EDITION Edited by RANJITA MISRA Professor & Research Director Center for the Study of Health Disparities (CSHD) Member, Intercollegiate Faculty of Nutrition Texas A&M University Contributors Nirmala Abraham Theja Mahalingaiah Padmini Balagopal Suraj Mathema Rita (Shah) Batheja Ranjita Misra Nimesh Bhargava Chhaya Patel Sharmila Chatterjee Thakor G Patel Madhu Gadia Sudha Raj Wahida Karmally Nirmala Ramasubramanian Keya Deshpande Karwankar Janaki Sengupta Karmeen Kulkarni Geeta Sikand Allied Publishers Private Limited New Delhi Mumbai Kolkata Chennai Nagpur Ahmedabad Bangalore Hyderabad Lucknow i Copyright © 2011 by AAPI All rights reserved. Written permission must be secured from AAPI to use or reproduce any part of this book. ISBN: 978 --- 81 --- 8424 --- 687687687 --- 222 Cover page designed by Ranjita Misra Photographs in the cover page were contributed by Wahida Karmally, Gerald Lemole, Nutrilite Health Institute, Kunal Patel, TG Patel and Parul Todai Reviewers Padmini Balagopal, Rita Batheja Wahida Karmally, Karmeen Kulkarni, Ranjita MisraMisra,, TG PatelPatel,,,, SudSudhaha Raj and Nirmala Ramasubramanian Published by Sunil Sachdev M/s. Allied Publishers Pvt. Ltd., 751, Anna Salai, Chennai – 600 002. The American Association of Physicians of Indian Origin (AAPI) 600 Enterprise Drive, Suite 108 Oak Brook, IL 60523 ii Contents Preface v TG Patel, MD, MACP Acknowledgements vii TG Patel, MD, MACP Forward ix Ajeet Singhvi, MD, FACG Chapter 1 Introduction 1 Dr. Sudha Raj, PhD, RD Chapter 2 Epidemiology, Risks and complications of Diabetes 6 Dr. Ranjita Misra, PhD, CHES & TG Patel, MD, MACP Chapter 3 Preventing Heart Disease in Asian Indians 11 Dr. Geeta Sikand, MA, RD, FADA, CDE, CLS Chapter 4 Renal Diet 23 Chhaya Patel, MA, RD, CSR Chapter 5 East Indian (Odia and Bengali) Cuisine 36 Dr. -
School Kids and Street Food
Contents A WALK WITH THE STREET ENTREPRENEUR A Golden Street food of TNAU Back gate LETTER TO THE VENDOR National Association of Street Vendors of India Do street foods need license? School kids and street food Top 10 street foods of world DAY OUT TO HEAVEN On a long straight road, I was struck in traffic, In my busy schedule, the day started quite terrific; The traffic seemed to deal a big questionnaire, That made my little vehicle froze stationary; My eyes had a glance at the roadside vendors, That tempted me to think that it might be tenders; “Oh it may not be”, my sound heart revealed, My mind pierced to find the facts concealed; Parking my vehicle in the “NO PARKING” zone, I neared one of the vendors with a humble tone; The lickonomics of the crowd induced me to taste, The hot idly and puri flickered that it will never go waste; My curiosity raised its height with the first bite, Making me to taste all the endowed items till night; That busy day never appeared to be a vain, Thinking that the whole eve had a huge gain; Street foods made me tour India from North to South, That the spice of dignity dwelled in my mouth; Leaving the place, I decided that the heaven is on Earth, And this day for street foods is sufficient for my birth; I started glorifying my diary with the events pretty beautiful, It’s my time for me to be highly thankful. Thank you God for my day with street foods….