Augmentative & Alternative Communication (AAC)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Globalization of Chinese Food ANTHROPOLOGY of ASIA SERIES Series Editor: Grant Evans, University Ofhong Kong
The Globalization of Chinese Food ANTHROPOLOGY OF ASIA SERIES Series Editor: Grant Evans, University ofHong Kong Asia today is one ofthe most dynamic regions ofthe world. The previously predominant image of 'timeless peasants' has given way to the image of fast-paced business people, mass consumerism and high-rise urban conglomerations. Yet much discourse remains entrenched in the polarities of 'East vs. West', 'Tradition vs. Change'. This series hopes to provide a forum for anthropological studies which break with such polarities. It will publish titles dealing with cosmopolitanism, cultural identity, representa tions, arts and performance. The complexities of urban Asia, its elites, its political rituals, and its families will also be explored. Dangerous Blood, Refined Souls Death Rituals among the Chinese in Singapore Tong Chee Kiong Folk Art Potters ofJapan Beyond an Anthropology of Aesthetics Brian Moeran Hong Kong The Anthropology of a Chinese Metropolis Edited by Grant Evans and Maria Tam Anthropology and Colonialism in Asia and Oceania Jan van Bremen and Akitoshi Shimizu Japanese Bosses, Chinese Workers Power and Control in a Hong Kong Megastore WOng Heung wah The Legend ofthe Golden Boat Regulation, Trade and Traders in the Borderlands of Laos, Thailand, China and Burma Andrew walker Cultural Crisis and Social Memory Politics of the Past in the Thai World Edited by Shigeharu Tanabe and Charles R Keyes The Globalization of Chinese Food Edited by David Y. H. Wu and Sidney C. H. Cheung The Globalization of Chinese Food Edited by David Y. H. Wu and Sidney C. H. Cheung UNIVERSITY OF HAWAI'I PRESS HONOLULU Editorial Matter © 2002 David Y. -

History&Perspectives
2012 CHINESE AMERICA History&Perspectives THE JOURNAL OF THE CHINESE HISTORICAL SOCIETY OF AMERICA CHINESE AMERICA HISTORY & PERSPECTIVES The Journal of the Chinese Historical Society of America 2012 CHINESE HISTORICAL SOCIETY OF AMERICA Chinese America: History & Perspectives — The Journal of the Chinese Historical Society of America Chinese Historical Society of America Museum & Learning Center 965 Clay Street San Francisco, California 94108 chsa.org Copyright © 2012 Chinese Historical Society of America. All rights reserved. Copyright of individual articles remains with the author(s). ISBN-13: 978-1-885864-47-5 ISBN-10: 1-885864-47-7 Design by Side By Side Studios, San Francisco. Permission is granted for reproducing up to fifty copies of any one article for Educa- tional Use as defined by the Digital Millennium Copyright Act. To order additional copies or inquire about large-order discounts, see order form at back or email [email protected]. Articles appearing in this journal are indexed in Historical Abstracts and America: History and Life. About the cover image: Lum Ngow with his parents in China, 1925. Photo courtesy of Lee Show Nam. 10 9 8 7 6 5 4 3 2 1 Contents THINGS MATTER Chinese American Culture Work and the Gods of Marysville 1 Jonathan H. X. Lee and Vivian-Lee Nyitray LIFE IN A CHINATOWN COLD WATER TENEMENT BUILDING 7 Lyle Jan HISTORY OF TRADITIONAL CHINESE MEDICINE IN CALIFORNIA A Perspective through the Stories of Four Acupuncturists 11 Emily S. Wu “We WERE REAL, SO THERE waS NO NEED TO BE AFRAID” Lum Ngow’s Long Detention on Angel Island 19 Judy Yung THE TWENTY-FIRST-CENTURY CHINESE AMERICA Growth and Diversity 27 Wei Li and Wan Yu About the Contributors 33 About the Editorial Committee 35 Guidelines for Manuscript Submission 37 Chinese Historical Society of America Membership Form 39 iii Things Matter Chinese American Culture Work and the Gods of Marysville Jonathan H. -

Does Standard Chinese Mean Anything for Cantonese Vowel Variation? Holman Tse, St
University of Pittsburgh From the SelectedWorks of Holman Tse October 11, 2019 Does standard Chinese mean anything for Cantonese vowel variation? Holman Tse, St. Catherine University Creative CommonThis sL wicorke nis sliceensed under a Creative Commons CC_BY-NC-ND International License. Available at: https://works.bepress.com/holman-tse/1/ Does standard Chinese mean anything for Cantonese vowel variation? Special Session: What’s so standard about standards? NWAV 48, University of Oregon, Eugene, OR October 11, 2019 Holman Tse, PhD Dept. of English and Intl Languages St. Paul, MN 55105 HERITAGE LANGUAGE VARIATION AND CHANGE IN TORONTO [email protected] HTTP://PROJECTS.CHASS.UTORONTO.CA/NGN/HLVC https://holmantse.github.io/ “A language is a dialect with an army and a navy” – Max Weinreich • Ex: Mutually intelligible Scandinavian “languages” vs. mutually unintelligible Chinese “dialects” (ex: Mandarin vs. Cantonese) • BUT Mandarin (Standard Chinese) and Cantonese are still genetically related (Sino-Tibetan Family) and share cognate vocabulary with systematic sound correspondences • Literate Cantonese speakers universally know written Mandarin because of the writing system • With the growing global importance of Mandarin (both spoken and written), could there be apparent time influence of Mandarin vowels on Cantonese vowels in cognate vocabulary? • Hypotheses to be tested: 1. Does Cantonese /y/ converge with Mandarin /u/ in cognate vocabulary? 2. Does Cantonese /i/ converge with Mandarin /ɨ/ in cognate vocabulary? • (ERROR: /ə/ instead -

The Role of Lexical Tone, Context, and Intonation in Cantonese-Chinese
Speech Comprehension in a Tone Language: The Role of Lexical Tone, Context, and Intonation in Cantonese-Chinese Catherine Carmen Kung Colofon Font: Garamond MT Std/I.Ming (I.明體) ISBN: 978-94-6284-148-2 Printed by: ProefschriftMaken || www.proefschriftmaken.nl Cover designed by Leah Harris Dutch translation by Laurence Bruggeman, and checked by Titia Benders Cantonese translation by Carmen Kung, and checked by Jacqueline Fong Speech Comprehension in a Tone Language: The Role of Lexical Tone, Context, and Intonation in Cantonese-Chinese Proefschrift ter verkrijging van de graad van doctor aan de Radboud Universiteit Nijmegen op gezag van de rector magnificus prof. dr. J.H.J.M. van Krieken, volgens besluit van het college van decanen in het openbaar te verdedigen op dinsdag 30 oktober 2018 om 12.30 uur precies door Catherine Carmen Kung geboren op 7 november 1984 te Hong Kong Promotor: Prof. dr. Herbert Schriefers Copromotor: Dr. Dorothee Chwilla Manuscriptcommissie: Prof. dr. Mirjam Ernestus Prof. dr. Niels Schiller (Universiteit Leiden) Dr. Yiya Chen (Universiteit Leiden) Speech Comprehension in a Tone Language: The Role of Lexical Tone, Context, and Intonation in Cantonese-Chinese Doctoral Thesis to obtain the degree of doctor from Radboud University Nijmegen on the authority of the Rector Magnificus prof. dr. J.H.J.M. van Krieken, according to the decision of the Council of Deans to be defended in public on Tuesday, October 30, 2018 at 12.30 hours by Catherine Carmen Kung Born on November 7, 1984 in Hong Kong Supervisor: Prof. dr. Herbert Schriefers Co-supervisor: Dr. Dorothee Chwilla Doctoral Thesis Committee: Prof. -

Westminsterresearch
WestminsterResearch http://www.westminster.ac.uk/westminsterresearch On the(re)emergence of cultural revolution imagery in China, Hong Kong and Singapore in the 21st century. Natalie Siu-Lam Wong School of Social Sciences, Humanities and Languages This is an electronic version of a PhD thesis awarded by the University of Westminster. © The Author, 2010. This is an exact reproduction of the paper copy held by the University of Westminster library. The WestminsterResearch online digital archive at the University of Westminster aims to make the research output of the University available to a wider audience. Copyright and Moral Rights remain with the authors and/or copyright owners. Users are permitted to download and/or print one copy for non-commercial private study or research. Further distribution and any use of material from within this archive for profit-making enterprises or for commercial gain is strictly forbidden. Whilst further distribution of specific materials from within this archive is forbidden, you may freely distribute the URL of WestminsterResearch: (http://westminsterresearch.wmin.ac.uk/). In case of abuse or copyright appearing without permission e-mail [email protected] ON THE (RE)EMERGENCE OF CULTURAL REVOLUTION IMAGERY IN CHINA, HONG KONG AND SINGAPORE IN THE 21 ST CENTURY NATALIE SIU-LAM WONG A thesis submitted in partial fulfilment of the requirements of the University of Westminster for the degree of Doctor of Philosophy October 2010 DECLARATION I certify that the thesis I have presented for examination for the degree of Doctor of Philosophy of the University of Westminster is solely my own work ABSTRACT This thesis interrogates the (re)emergence of Cultural Revolution imagery in the 21 st century as a cultural lens through which contemporary contradictory relations between China, Hong Kong and Singapore are revealed. -

Denise Ho (HOCC) Fandom Before and After the Coming-Out
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by King's Research Portal King’s Research Portal Document Version Peer reviewed version Link to publication record in King's Research Portal Citation for published version (APA): Li, E. C. Y. (2017). Desiring Queer, Negotiating Normal: Denise Ho (HOCC) Fandom before and after the Coming-Out. In M. Lavin, L. Yang, & J. J. Zhao (Eds.), Boys’ Love, Cosplay, and Androgynous Idols: Queer Fan Cultures in Mainland China, Hong Kong, and Taiwan (pp. 131-156). Hong Kong: University of Hong Kong Press. Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -
Ready to Learn but Nowhere to Go
SPECIAL REPORT PARENTS’ GUIDE Monday, February 25, 2013 Missed education Ready to learn but nowhere to go Is Hong Kong failing its school kids? Super schools for maths, Play boosts creativity Case studies: Teachers science and financial nous and language skills stand up and deliver Contents PARENTS’ GUIDE Monday, February 25, 2013 04 Cover story Gaps in education 08 Parents turn creative amid frustrations 10 Business gives government a pass 11 Lessons on easing class shortage woes 12 Arts Art beyond art’s sake 14 Case study: At Blooming Buds, kids learn to play 16 Play & Learn Workout for young minds 20 Finance EDITORIAL Money matters for kids Chief Editor 22 Case study: Valuing financial knowledge at HKIS Rex Aguado [email protected] Assistant Editors 24 Languages Ginn Fung [email protected] Young tongues wagging Hilda Poon [email protected] 26 Case study: Kellett welcomes early Putonghua learning Subeditor Tom Eves [email protected] 28 Maths & Sciences A head for numbers Web Editor 30 Case study: Rooting for knowledge at Garden House Carmen Tao [email protected] Editorial Co-ordinator Nick Ho [email protected] Production & Design Editor Jun Cambel [email protected] Designer Bay Leung [email protected] ADVERTISING Sales Manager Dickson Fong [email protected] Senior Sales Executives Florence Ho [email protected] Kelvin Wong [email protected] Sales Executive Rita Ng [email protected] Cover composition: Bay Leung Cover photos: SCMP and agencies Parents’ Guide is published and printed by South China Morning Post Centre Publishers Limited. -
Hong Kong? Get Tips from Your Alumni Network!
WANT TO WORK IN HONG KONG? GET TIPS FROM YOUR ALUMNI NETWORK! Young professionals and graduate employers from the Birmingham alumni community share their experiences of living and working in Hong Kong. With more than 300,000 alumni, there are This guide will take you through the process of Birmingham graduates across the globe. moving to Hong Kong, with insights from alumni Hong Kong is one of the most popular who have already made the move. It will cover destinations for our alumni, with almost 3,000 what to plan before leaving, how to find and based there. apply for jobs and how to integrate into society. THE BASICS In case you haven’t started POPULATION your research yet, let our 7.23 MILLION alumni talk you through the basics of life in Hong Kong. MAIN EMERGENCY Hong Kong is a city of diversity and people NATIONALITY NUMBERS from everywhere in the world live here. Alexander Buencamino (MSc Money, Banking CHINESE (94%) 999 (POLICE, and Finance, 1994) AMBULANCE, FIRE) MAIN INTERNET DOMAIN TRANSPORT CURRENCY www.... PUBLIC TRANSPORT HONG KONG DOLLAR .HK (HKD OR HK$) The metro system (MTR) is frequent and reliable, and you can get virtually anywhere within an hour. CANTONESE Desiree Ho (LLB Law, 2012) MAIN LANGUAGES AND ENGLISH There are excellent opportunities for travelling in Asia. Transport is easy and People in Hong Kong very affordable. There is also the benefit of speak excellent being able to leave the city as Hong Kong Since English is English, but we still is 75% countryside. widely adopted in need to be mindful Jennifer Greaves (BSc Psychology, 2007) Hong Kong it is very of our accents, pace easy to get around and the specific and ask for help. -
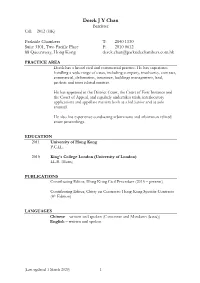
Derek J Y Chan Barrister Call: 2012 (HK)
Derek J Y Chan Barrister Call: 2012 (HK) Parkside Chambers T: 2840 1130 Suite 3101, Two Pacific Place F: 2810 0612 88 Queensway, Hong Kong [email protected] PRACTICE AREA Derek has a broad civil and commercial practice. He has experience handling a wide range of cases, including company, insolvency, contract, commercial, defamation, insurance, buildings management, land, probate and trust related matters. He has appeared in the District Court, the Court of First Instance and the Court of Appeal, and regularly undertakes trials, interlocutory applications and appellate matters both as a led junior and as sole counsel. He also has experience conducting arbitrations and arbitration-related court proceedings. EDUCATION 2011 University of Hong Kong P.C.LL. 2010 King’s College London (University of London) LL.B. (Hons) PUBLICATIONS Contributing Editor, Hong Kong Civil Procedure (2015 – present) Contributing Editor, Chitty on Contracts: Hong Kong Specific Contracts (4 th Edition) LANGUAGES Chinese – written and spoken (Cantonese and Mandarin (basic)) English – written and spoken (Last updated 1 March 2020) 1 SELECTED CASES Companies and insolvency Re Sit Kwong Lam [2019] HKCA 1220 – Bankruptcy Petition / Arbitration Clause (led by Victor Dawes SC) Long Hai Hong v Liu Dan & Others [2019] HKCFI 1827 – Common law derivative action / Resisting striking out application Re Merdeka Financial Services Group Ltd [2018] HKCFI 163 – Winding up / Non-Hong Kong company / Validation Order Re Global Eco Resource Ltd [2018] HKCFI 1658 – Shareholders’ -

Infinite Univer Se 蕭勤-無限宇宙
HSIAO CHIN – INFINITE UNIVERSE 蕭勤-無限宇宙 HK0880 A SELLING EXHIBITION 展售會 SOTHEBY’S S|2 GALLERY | 蘇富比S|2藝術空間 5/F ONE PACIFIC PLACE | 太古廣場1座5樓 88 QUEENSWAY, HONG KONG | 香港金鐘道88號 OPENING HOURS 開放時間 10 SEP - 9 OCT 2019 | 2019年9月10日至 10月9日 MONDAY – FRIDAY 10AM – 6PM | 星期一至五 早上10時至下午6時 SATURDAY 11AM – 5PM | 星期六 早上11時至下午5時 CLOSED ON SUNDAYS AND PUBLIC HOLIDAYS | 星期日及公眾假期休息 ENQUIRIES 查詢 [email protected] +852 2822 5566 SOTHEBYS.COM/ HSIAOCHIN Supported by 全力支持 Following this spring’s solo exhibition at the Musée Guimet in in face of the actuality of these ideas, I wanted to seek the 繼今年春天法國巴黎吉美博物館為我舉行個展後,我非常高興在今秋應邀於香港蘇富比S|2藝術空間舉 Paris, I was delighted to be invited to hold a solo exhibition at conceptual purity and the point where creativity derived from 行個人展覽。特別感謝香港蘇富比郭東杰先生及黃傑瑜先生,為我定下今次展覽主題—《無限宇宙》。 Sotheby's S|2 Gallery in Hong Kong this fall. I would particularly amid the turmoil. Punto is the point and the basis of all matters, 今次展出包括自1960年代初我在意大利米蘭創立「龐圖國際藝術運動」以來的一些比較具代表性的作 like to thank Mr Felix Kwok and Mr Jonathan Wong from which signifies both the beginning and the end; it is rigorous, 品。更有一系列近年在米蘭以玻璃馬賽克與另一位義大利藝術工作者共同創作的多幅馬賽克作品。 Sotheby's Hong Kong for setting the title of this exhibition: simple, affirmative, permanent, and constructive. 我們先來談談PUNTO(點)龐圖國際藝術運動: ‘Infinite Universe’. The exhibition will include some of my most Some of the important elements in my work will touch the iconic works since the early 1960s, when I founded Movimento viewer; they have been described as full of universal feeling and 二戰後盛行之歐洲非形象主義及美國行動繪畫,已在60年代失去原創精神及生命力,此兩大派別著重創 Punto in Milan. It will also feature a series of my recent glass love, due to the combination of life experiences and ideas in my 作的行動與情緒在作品中呈現。我認為視覺藝術創作應強調深層思考與觀察,否則藝術無長久存在的社 mosaic works, made in Milan with another Italian artist. -

The Transnational History of a Chinese Family Ii Acknowledgments Acknowledgments Iii the Transnational History of a Chinese Family
Acknowledgments i The Transnational History of a Chinese Family ii Acknowledgments Acknowledgments iii The Transnational History of a Chinese Family IMMIGRANT LETTERS, FAMILY BUSINESS, AND REVERSE MIGRATION h HAIMING LIU Rutgers University Press New Brunswick, New Jersey, and London iv Acknowledgments Library of Congress Cataloging-in-Publication Data Liu, Haiming, 1953– The transnational history of a Chinese family : immigrant letters, family business, and reverse migration / Haiming Liu. p. cm. Includes bibliographical references and index. ISBN 0-8135-3596-4 (hardcover : alk. paper) — ISBN 0-8135-3597-2 (pbk. : alk. paper) 1. Chang family. 2. Chinese Americans—California—Biography. 3. California— Emigration and immigration—History. 4. China—Emigration and immigration—History. I. Title. F870.C5L58 2005 304.8'73051'0922—dc22 2004023483 A British Cataloging-in-Publication record for this book is available from the British Library. Copyright © 2005 by Haiming Liu All rights reserved No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical, or by any information storage and retrieval system, without written permission from the publisher. Please contact Rutgers University Press, 100 Joyce Kilmer Avenue, Piscataway, NJ 08854–8099. The only exception to this prohibition is “fair use” as defined by U.S. copyright law. Manufactured in the United States of America Acknowledgments v To my own family vi Acknowledgments Acknowledgments vii CONTENTS Acknowledgments ix Note on Romanization xiii Introduction -

“Do You Hear the People Sing” “Lift Your Umbrella”? Understanding Hong Kong’S Pro-Democratic Umbrella Movement Through Youtube Music Videos
China Perspectives 2016/4 | 2016 The Health System and Access to Healthcare in China “Do You Hear the People Sing” “Lift Your Umbrella”? Understanding Hong Kong’s Pro-democratic Umbrella Movement through YouTube Music Videos Tim Rühlig Electronic version URL: http://journals.openedition.org/chinaperspectives/7125 DOI: 10.4000/chinaperspectives.7125 ISSN: 1996-4617 Publisher Centre d'étude français sur la Chine contemporaine Printed version Date of publication: 1 December 2016 Number of pages: 59-68 ISSN: 2070-3449 Electronic reference Tim Rühlig, « “Do You Hear the People Sing” “Lift Your Umbrella”? », China Perspectives [Online], 2016/4 | 2016, Online since 01 December 2017, connection on 10 December 2020. URL : http:// journals.openedition.org/chinaperspectives/7125 ; DOI : https://doi.org/10.4000/chinaperspectives. 7125 © All rights reserved Article China perspectives “Do You Hear the People Sing” “Lift Your Umbrella”? Understanding Hong Kong’s Pro-democratic Umbrella Movement through YouTube Music Videos TIM RÜHLIG ABSTRACT: Around the world, music serves as an important element of mobilisation for social movements. Singing songs is not only a peaceful protest technique but also helps to construct a protest identity locating and relating the social movement to its political and social environment. Most importantly, a social movement is to a significant extent remembered through its music, and this determines its future impact on local (contentious) politics. Against this backdrop, this article seeks to understand Hong Kong’s Umbrella Movement through four YouTube music videos, analysing the lyrics, music, and video imagery in order to carve out core elements and values of the Umbrella Movement. Especially given the importance of Hong Kong’s identity as a “global” city with a cosmopolitan culture and past, the peaceful nature of the movement and the rise of a xenophobic localism in the shape of sarcasm are emphasised.