WO 2007/054693 Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Communicable Disease Control
LECTURE NOTES For Nursing Students Communicable Disease Control Mulugeta Alemayehu Hawassa University In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education 2004 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2004 by Mulugeta Alemayehu All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. Communicable Disease Control Preface This lecture note was written because there is currently no uniformity in the syllabus and, for this course additionally, available textbooks and reference materials for health students are scarce at this level and the depth of coverage in the area of communicable diseases and control in the higher learning health institutions in Ethiopia. -
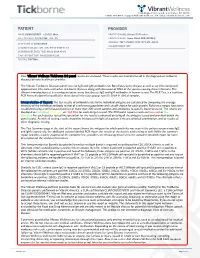
View Tickborne Diseases Sample Report
1360 Bayport Ave, Ste B. San Carlos, CA 94070 1(866) 364-0963 | [email protected] | www. vibrant-wellness.com PATIENT PROVIDER NAME: DEMO REPORT GENDER: Male PRACTICE NAME: Vibrant IT4 Practice DATE OF BIRTH: 04/14/1998 AGE: 22 PROVIDER NAME: Demo Client, DDD (999994) ADDRESS: TEST STREET, TEST CITY, KY- 42437. ACCESSION ID: 2009220006 PHLEBOTOMIST: 607 SPECIMEN COLLECTION TIME: 09-21-2020 11:14 SPECIMEN RECEIVED TIME: 09-22-2020 05:14 FINAL REPORT TIME: 09-25-2020 15:56 FASTING: FASTING Your Vibrant Wellness TickBorne 2.0 panel results are enclosed. These results are intended to aid in the diagnosis of tickborne diseases by your healthcare provider. The Vibrant Tickborne Diseases panel tests for IgG and IgM antibodies for Borreliosis/Lyme disease as well as co-infection(s) and opportunistic infections with other tick-borne illnesses along with detection of DNA of the species causing these infections. The Vibrant Immunochip test is a semiquantitative assay that detects IgG and IgM antibodies in human serum. The PCR Test is a real-time PCR Assay designed for qualitative detection of infectious group- specific DNA in clinical samples. Interpretation of Report: The test results of antibody levels to the individual antigens are calculated by comparing the average intensity of the individual antibody to that of a reference population and cut-off chosen for each protein. Reference ranges have been established using a well characterized set of more than 300 serum samples and antibodies to specific bacteria tested. The results are displayed as In Control, Moderate, or High Risk.for each antigen tested. -
![United States Patent [191 [11] Patent Number: 5,403,718 Durward Et Al](https://docslib.b-cdn.net/cover/0393/united-states-patent-191-11-patent-number-5-403-718-durward-et-al-390393.webp)
United States Patent [191 [11] Patent Number: 5,403,718 Durward Et Al
. US005403718A United States Patent [191 [11] Patent Number: 5,403,718 Durward et al. [451 Date of Patent: * Apr. 4, 1995 [54] METHODS AND ANTIBODIES FOR THE I OTHER PUBLICATIONS IMMUNE CAPTURE AND DETECHON 0F Nowinski et al, Science, 219:637-644 (11 Feb. 1983), BQRRELI-A BURGDORFERI - “Monoclonal Antibodies for Diagnosis of Infectious [76] Inventors: David W. Dorward, 401 N. 7th St; Diseases in Humans”. Tom G. Schwan, 601 S. 5th St.; . E . _ 1 E . Claude F. Garon, 904 Ponderosa Dr., Primary xammer Caro ' Bldwen all of Hamilton, Mont. 59840 [57] ABSTRACT [ * ] Notice; The portion of the term of this patent The invention relates to novel antigens associated with subsequent to Jun, 8, 2010 has been Borrelia burgdorferi which are exported (or shed) in disclaimed. vivo and whose detection is a means of diagnosing _ Lyme disease. The antigens are extracellular membrane [211 App 1' No" 929’172 vesicles and other bioproducts including the major ex [22] Filed: Aug. 11,1992 tracellular protein. The invention further provides anti bodies, monoclonal and/or polyclonal, labeled and/or Related US. Application Data unlabeled, that react with the antigens. The invention [63] Continuation-impart ofSer. No. 485 551 Feb. 27 1990 . relates to a math“ for immune capture of Speci?c mi‘ Pat No_ 5,217,871 ’ ’ ’ ’ , croorganisms for their subsequent cultivation. The in vention is also directed to a method of diagnosing Lyme clci? ------------------ -- GolN 332940 disease by detecting the antigens in a biological sample . ................................ .. , . , taken from a host using the antibodies in conventional 530/3871; 530/388.4; 530/3895 immunoassay formats. -

IS IT LYME DISEASE, Or TICK-BORNE RELAPSING FEVER?
IS IT LYME DISEASE, or TICK-BORNE RELAPSING FEVER? Webinar Presented by Joseph J. Burrascano Jr. M.D. Joined by Jyotsna Shah PhD for the Q&A January 2020 Presenters Joseph J. Burrascano Jr. M.D. • Well-known pioneer in the field of tick-borne diseases, active since 1985 • Founding member of ILADS and ILADEF • Active in physician education on all aspects of tick-borne diseases Jyotsna Shah, PhD • President & Laboratory Director of IGeneX Clinical Laboratory • Over 40 Years of Research Experience in Immunology, Molecular Biology & Microbiology • Author of Multiple Publications & Holds More Than 20 Patents • Member of ILRAD as a Post-Doctoral Scientist • Started the First DNA Sequencing Laboratory in E. Africa 2 Poll Question Before we begin, we’d like to ask a poll question. Which one of these Borrelia causes Tick-Borne Relapsing Fever (TBRF)? a) B. mayonii b) B. turicatae c) B. burgdorferi d) B. andersonii e) B. garinii 3 Poll Question Before we begin, we’d like to ask a poll question. Which one of these Borrelia causes Tick-Borne Relapsing Fever (TBRF)? a) B. mayonii - Lyme b) B. turicatae - TBRF c) B. burgdorferi - Lyme d) B. andersonii - Lyme e) B. garinii – Lyme strain in Europe 4 What is TBRF? • Has been defined by clinical presentation • Has been defined by tick vector • Has been defined by genetics • Has been defined by serotype BUT • Each of these has exceptions and limitations! 5 Clinical Presentation of Classic TBRF • “Recurring febrile episodes that last ~3 days and are separated by afebrile periods of ~7 days duration.” • “Each febrile episode involves a “crisis.” During the “chill phase” of the crisis, patients develop very high fever (up to 106.7°F) and may become delirious, agitated, tachycardic and tachypneic. -

Electronic Laboratory Reporting Use Case January 2011
ILLINOIS HEALTH INFORMATION EXCHANGE Electronic Laboratory Reporting Use Case Electronic Laboratory Reporting and Health Information Exchange Illinois Health Information Exchange Public Health Work Group January 2011 Electronic Laboratory Reporting Use Case January 2011 Table of Contents 1.0 Executive Summary……………………………………………………………………….3 2.0 Introduction…………………………………………………………………...……………..5 3.0 Scope……………………………………..………………………………………………………5 4.0 Use Case Stakeholders…………………………………………………………….….....6 5.0 Issues and Obstacles……………………………………………………………………...8 6.0 Use Case Pre-Conditions .………………….…………………………………………...8 7.0 Use Case Post-Conditions.……………………………………………………………...9 8.0 Detailed Scenarios/Technical Specifications.………………………………10 9.0 Validation and Certification………………………………………………………...12 Appendix ………………………………………………………………………………………….....13 Page 2 Electronic Laboratory Reporting Use Case January 2011 1.0 Executive Summary This Use Case is a product of the Public Health Work Group (PHWG) of the Illinois Health Information Exchange (HIE) Advisory Committee. The Illinois HIE Advisory Committee was constituted as the diverse public healthcare stakeholder body providing input and recommendations on the creation of the Illinois Health Information Exchange Authority (“the Authority”) as the Illinois vehicle for designing and implementing electronic health information exchange in Illinois. The establishment of the Authority marks the formal transition of the work of the HIE Advisory Committee and the Work Groups into alignment with the provisions of Illinois -

Vector-Borne Disease Flyer
Do You Have Patients That Suffer from Chronic Pain and Fatigue? Medical Diagnostic Laboratories offers State-of-the-art Vector-Borne Disease Testing • Comprehensive vector-borne test menu including Lyme disease and viral & bacterial coinfections • Detection by DNA-based Polymerase Chain Reaction (PCR) and serology-based IgG/IgM • C6 Peptide ELISA testing for Borrelia burgdorferi • CDC and alternative interpretation of bands provided for Borrelia burgdorferi Immunoblot • Test additions available up to 30 days after collection • No refrigeration required before or after collection • 5-10 days turnaround time • Affordable patient pricing for non-insured patients • We file all insurances including Medicare, Medicaid, PPOs and HMOs • Founded in 1997 as a vector-borne & Lyme testing laboratory • Testing available for patients of all ages A DIVISION OF • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • TM Medical Diagnostic Laboratories, L.L.C. CLINICAL www.mdlab.com • 877.269.0090 DIAGNOSTICS 7/2019 Vector-Borne Diseases TICK-BORNE DISEASES Anaplasmosis & Ehrlichiosis 439 Anaplasma phagocytophilum lgG/lgM by IFA (serum required) 411 Ehrlichia chaff eensis (HME) & Anaplasma phagocytophilum (HGE) by Real-Time PCR 456 Ehrlichia ewingii (HME) by Real-Time PCR Babesiosis 431 Babesia duncani (WA-1) by Real-Time PCR 410 Babesia microti by Real-Time PCR 440 Babesia microti IgG/IgM by IFA (serum required) Borreliosis - Lyme disease 424 Borrelia afzelii (Europe) by Real-Time PCR 441 Borrelia afzelii (Europe) by Western -

Bacteriology
SECTION 1 High Yield Microbiology 1 Bacteriology MORGAN A. PENCE Definitions Obligate/strict anaerobe: an organism that grows only in the absence of oxygen (e.g., Bacteroides fragilis). Spirochete Aerobe: an organism that lives and grows in the presence : spiral-shaped bacterium; neither gram-positive of oxygen. nor gram-negative. Aerotolerant anaerobe: an organism that shows signifi- cantly better growth in the absence of oxygen but may Gram Stain show limited growth in the presence of oxygen (e.g., • Principal stain used in bacteriology. Clostridium tertium, many Actinomyces spp.). • Distinguishes gram-positive bacteria from gram-negative Anaerobe : an organism that can live in the absence of oxy- bacteria. gen. Bacillus/bacilli: rod-shaped bacteria (e.g., gram-negative Method bacilli); not to be confused with the genus Bacillus. • A portion of a specimen or bacterial growth is applied to Coccus/cocci: spherical/round bacteria. a slide and dried. Coryneform: “club-shaped” or resembling Chinese letters; • Specimen is fixed to slide by methanol (preferred) or heat description of a Gram stain morphology consistent with (can distort morphology). Corynebacterium and related genera. • Crystal violet is added to the slide. Diphtheroid: clinical microbiology-speak for coryneform • Iodine is added and forms a complex with crystal violet gram-positive rods (Corynebacterium and related genera). that binds to the thick peptidoglycan layer of gram-posi- Gram-negative: bacteria that do not retain the purple color tive cell walls. of the crystal violet in the Gram stain due to the presence • Acetone-alcohol solution is added, which washes away of a thin peptidoglycan cell wall; gram-negative bacteria the crystal violet–iodine complexes in gram-negative appear pink due to the safranin counter stain. -

Borrelia Infection in Latin America
REVISTA DE INVESTIGACIÓN CLÍNICA Contents available at PubMed www .clinicalandtranslationalinvestigation .com PERMANYER Rev Inves Clin. 2018;70:158-63 BRIEF REVIEW Borrelia Infection in Latin America Alejandro Robles1, James Fong2 and Jorge Cervantes2,3* 1Department of Internal Medicine, 2Paul L. Foster School of Medicine and 3Department of Medical Education, Texas Tech University Health Sciences Center, El Paso, TX, USA ABSTRACT Lyme disease (LD) is a multisystemic inflammatory disease caused by pathogenic spirochetes, belonging to the genospecies complex Borrelia burgdorferi sensu lato (B.b.s.l.). Around the world, distinct species of Ixodes tick vectors transmit different species of Borrelia. Despite the rising recognition and occurrence of tick-borne disease in Latin America, serology has proven to be inconclusive in detecting suspected LD cases. Recently, new B.b.s.l. strains or new related species have been described in Brazil, Uruguay, and Chile. This could explain the lack of confirmatory tests, such as indeterminate Western blots (WBs) and polymerase chain reactions, in detecting suspected LD cases in this region of the world. Future studies will need to determine the extension of novel B.b.s.l. species infections in ticks, reservoirs, and humans in Latin America. The existence of these new Borrelia genomic species should prompt the development of innovative diagnostic and clinical approaches. (REV INVES CLIN. 2018;70:158-63) Key words: Lyme disease. Borrelia. Latin America. LYME DISEASE (LD) - multisystemic inflammatory disease caused by patho- GLOBAL DISTRIBUTION genic spirochetes of the Borrelia burgdorferi sensu lato (B.b.s.l.) complex. LD is the most common vector-borne illness in the United States, and a major zoonosis in Europe and LD was first described nearly 40 years ago after an China1,2. -

Article & Appendix
Case Report and Genetic Sequence Analysis of Candidatus Borrelia kalaharica, Southern Africa Katarina Stete,1 Siegbert Rieg,1 Gabriele Margos, Georg Häcker, Dirk Wagner, Winfried V. Kern, Volker Fingerle Tickborne relapsing fever caused by Borrelia species is geographic regions, and they have traditionally been di- rarely reported in travelers returning from Africa. We report vided into Old World and New World Borrelia. So far, ≈15 a case of a 71-year-old woman who sought treatment at Borrelia species have been described to cause TBRF in hu- University Medical Center in Freiburg, Germany, in 2015 mans worldwide (1). In Africa, TBRF has been traditionally with recurrent fever after traveling to southern Africa. We attributed to B. crocidurae in western Africa, B. hispanica detected spirochetes in Giemsa-stained blood smears. in northern Africa, and B. duttonii in eastern Africa (1,4). Treatment with doxycycline for suspected tickborne relaps- ing fever was successful. Sequence analyses of several loci Because microscopy is currently the standard method (16S rRNA, flagellin, uvrA) showed high similarity to the re- for diagnosis of TBRF in most countries in Africa, diagno- cently described Candidatus Borrelia kalaharica, which was sis does not usually include differentiation of species. With found in a traveler returning from the same region earlier the advent of molecular diagnostic methods, scientists can that year. We provide additional information regarding the identify species by sequencing different loci of Borrelia genetic relationship of Candidatus B. kalaharica. Sequence DNA from blood, such as the 16S rRNA gene, the flagel- information for an additional 6 housekeeping genes enables lin gene (flaB), or the glpQ gene (5,6). -

What's New in Tick-Borne Disease?
What’s New In Tick-borne Disease? Lyme Disease Relapsing Fever and beyond… Marc Roger Couturier, Ph.D., D(ABMM) Medical Director, Infectious Disease and Immunology ARUP Laboratories Associate Professor of Pathology University of Utah Objectives 1. Understand the epidemiology of tick-borne diseases and the ticks that vector the diseases. 2. Recognize the growing list of tick-borne diseases. 3. Recall the testing available for detection of tick-borne diseases. Anatomy of the tick… 3 Hard Shell Tick (Ixodid) vs Soft Shell (Agasid) https://www.cdc.gov/dpdx/ticks/index.html Hard Ticks-Life Cycle https://www.cdc.gov/dpdx/ticks/index.html Ixodid Ticks – male vs. female female male https://www.cdc.gov/dpdx/ticks/index.html Hard Shelled Ticks of the Northeast Ixodes scapularis “Deer tick or black-legged tick” Rhipicephalus sanguineus “Brown dog tick” Dermacentor variabilis Amblyomma americanum “American Dog Tick” “Lonestar Tick” https://www.cdc.gov/dpdx/ticks/index.html Amblyomma americanum Amblyomma americanum • Ehrlichia ewingii Human monocytic ehrlichiosis • Ehrlichia chaffeensis • Francisella tularensis • STARI (Southern Tick Associated Rash Illness) • Heartland virus Rhipicephalus sanguineus Rhipicephalus sanguineus • Rickettsia rickettsii (Rocky mountain spotted fever) **In the southern USA only** Dermacentor variabilis Dermacentor variabilis. • Ehrlichia spp. (Human monocytic ehrlichiosis) • Rickettsia rickettsii (Rocky mountain spotted fever) • Francisella tularensis (Tularemia) Ixodes scapularis Ixodes scapularis • Borrelia burgdorferi -

Practice of Medicine Infections
PRACTICE OF MEDICINE INFECTIONS Dr. Sunila MD (Hom) Medical Officer,Department of Homeopathy Govt of Kerala Infection: Lodging & multiplication of the organisms in or on the tissues of host. Primary infection: Initial infection of a host by a parasite. Reinfection: Subsequent infections by the same parasite in the same host. Secondary infection: Infection by another organism in a person suffering from an infectious disease. Nosocomial infection: Cross infections occurring in hospitals. Superinfections: Infections caused by a commensal bacterium in patients who receive intensive chemotherapy. Opportunistic infections: Organisms that ordinarily do not cause disease in healthy persons may affect individuals with diminished resistance. Latent infections: When a pathogen remains in a tissue without producing any disease, but leads to disease when the host resistance is lowered. Commonest infective disease: common cold. PYREXIA OF UNKNOWN ORIGION (PUO) When the temperature is raised above 38.3°C for more than 2 weeks without the cause being detected by physical examination or laboratory tests → PUO (FUO) Etiology a) Occult tuberculosis b) Chronic suppurative lesions of the liver, pelvic organs, urinary tract, peritoneum, gall bladder, brain, lungs, bones & joints & dental sepsis (occasionally). c) Viral infections: Viral hepatitis Infectious mononucleosis Cytomegalovirus infection Aids d) Connective tissue disorders: Giant cell arteritis. RA Rheumatic fever SLE PAN (polyarteritis nodosa) e) Chronic infections: Syphilis Hepatic amoebiasis Cirrhosis liver Malaria Filariasis Leprosy Brucellosis Sarcoidosis f) Haematological malignancies Leukemia Lymphoma Multiple myeloma g) Other malignant lesions: Tumours of lungs, kidney etc. h) Allergic conditions www.similima.com Page 1 i) Miscellaneous conditions: Hemolytic anaemia, dehydration in infants etc. j) Factitious fever: Self induced fever in patients with psychological abnormalities. -

Emerging Tickborne Diseases
CDC PUBLIC HEALTH GRAND ROUNDS Emerging Tickborne Diseases AAccessible version: https://youtu.be/al5EM3yh--0 March 21, 2017 Expanding Diversity and Distribution of Tickborne Diseases Rebecca Eisen, PhD Research Biologist Division of Vector-Borne Diseases National Center for Emerging and Zoonotic Infectious Diseases The Basics of Tickborne Diseases All known tickborne infectious diseases are diseases of animals that can be transmitted to humans via a tick vector (e.g., zoonoses) ● Ticks can maintain the pathogens through transmission to their offspring ● Ticks can acquire infection through feeding on infectious hosts Humans are incidental hosts, infected by the bite of infected ticks Ticks Can Transmit Diverse Types of Bacteria in the United States Bacterial Diseases (9) Pathogens (14) Tick Genera (5) Anaplasmosis Anaplasma phagocytophilum Ixodes spp. Borrelia miyamotoi disease Borrelia miyamotoi Ixodes spp. Ehrlichia chaffeensis Amblyomma spp. Ehrlichiosis Ehrlichia ewingii Ixodes spp. Ehrlichia muris eauclarensis Borrelia burgdorferi Lyme disease Ixodes spp. Borrelia mayonii Rickettsia parkeri rickettsiosis Rickettsia parkeri Amblyomma spp. Dermacentor spp. Rocky Mountain spotted fever Rickettsia rickettsii Rhipicephalus spp. Pacific Coast tick fever Rickettsia philipii Dermacentor spp. Borrelia hermsii Relapsing fever Borrelia parkeri Ornithodoros spp. Borrelia turicatae Amblyomma spp. Tularemia Francisella tularensis Dermacentor spp. Eisen RJ, Kugeler KJ, Eisen L et al. (2017) ILAR J, in press. Other Types of Pathogens Ticks Can Transmit Diseases (4) Pathogens (4) Tick Genera (3) Viruses Colorado tick fever virus Colorado tick fever Dermacentor spp. (Coltivirus) Heartland virus Heartland virus disease Amblyomma spp. (Phlebovirus) Powassan virus Powassan encephalitis Ixodes spp. (Flavivirus) Protozoa Babesiosis Babesia microti Ixodes spp. Eisen RJ, Kugeler KJ, Eisen L et al.