A Mirror of Internal Malignancy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiating Between Anxiety, Syncope & Anaphylaxis
Differentiating between anxiety, syncope & anaphylaxis Dr. Réka Gustafson Medical Health Officer Vancouver Coastal Health Introduction Anaphylaxis is a rare but much feared side-effect of vaccination. Most vaccine providers will never see a case of true anaphylaxis due to vaccination, but need to be prepared to diagnose and respond to this medical emergency. Since anaphylaxis is so rare, most of us rely on guidelines to assist us in assessment and response. Due to the highly variable presentation, and absence of clinical trials, guidelines are by necessity often vague and very conservative. Guidelines are no substitute for good clinical judgment. Anaphylaxis Guidelines • “Anaphylaxis is a potentially life-threatening IgE mediated allergic reaction” – How many people die or have died from anaphylaxis after immunization? Can we predict who is likely to die from anaphylaxis? • “Anaphylaxis is one of the rarer events reported in the post-marketing surveillance” – How rare? Will I or my colleagues ever see a case? • “Changes develop over several minutes” – What is “several”? 1, 2, 10, 20 minutes? • “Even when there are mild symptoms initially, there is a potential for progression to a severe and even irreversible outcome” – Do I park my clinical judgment at the door? What do I look for in my clinical assessment? • “Fatalities during anaphylaxis usually result from delayed administration of epinephrine and from severe cardiac and respiratory complications. “ – What is delayed? How much time do I have? What is anaphylaxis? •an acute, potentially -

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -
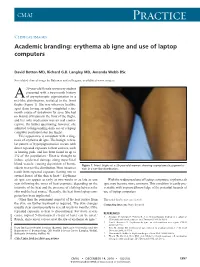
Erythema Ab Igne and Use of Laptop Computers
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Erythema Annulare Centrifugum ▪ Erythema Gyratum Repens ▪ Exfoliative Erythroderma Urticaria ▪ COMMON: 15% All Americans
Cutaneous Signs of Internal Malignancy Ted Rosen, MD Professor of Dermatology Baylor College of Medicine Disclosure/Conflict of Interest ▪ No relevant disclosures ▪ No conflicts of interest Objectives ▪ Recognize common disorders associated with internal malignancy ▪ Manage cutaneous disorders in the context of associated internal malignancy ▪ Differentiate cutaneous signs of leukemia and lymphoma ▪ Understand spidemiology of cutaneous metastases Cutaneous Signs of Internal Malignancy ▪ General physical examination ▪ Pallor (anemia) ▪ Jaundice (hepatic or cholestatic disease) ▪ Fixed erythema or flushing (carcinoid) ▪ Alopecia (diffuse metastatic disease) ▪ Itching (excoriations) Anemia: Conjunctival pallor and Pale skin Jaundice 1-12% of hepatocellular, biliary tree or pancreatic cancer PRESENT with jaundice, but up to 40-60% eventually develop it World J Gastroenterol 2003;9:385-91 For comparison CAN YOU TELL JAUNDICE FROM NORMAL SKIN? JAUNDICE Alopecia Neoplastica Most common report w/ breast CA Lung, cervix, desmoplastic mm Hair loss w/ underlying induration Biopsy = dermis effaced by tumor Ann Dermatol 26:624, 2014 South Med J 102:385, 2009 Int J Dermatol 46:188, 2007 Acta Derm Venereol 87:93, 2007 J Eur Acad Derm Venereol 18:708, 2004 Gastric Adenocarcinoma: Alopecia Ann Dermatol 2014; 26: 624–627 Pruritus: Excoriation ▪ Overall risk internal malignancy presenting as itch LOW. OR =1.14 ▪ CTCL, Hodgkin’s & NHL, Polycythemia vera ▪ Biliary tree carcinoma Eur J Pain 20:19-23, 2016 Br J Dermatol 171:839-46, 2014 J Am Acad Dermatol 70:651-8, 2014 Non-specific (Paraneoplastic) Specific (Metastatic Disease) Paraneoplastic Signs “Curth’s Postulates” ▪ Concurrent onset (temporal proximity) ▪ Parallel course ▪ Uniform site or type of neoplasm ▪ Statistical association ▪ Genetic linkage (syndromal) Curth HO. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Urticaria from Wikipedia, the Free Encyclopedia Jump To: Navigation, Search "Hives" Redirects Here
Urticaria From Wikipedia, the free encyclopedia Jump to: navigation, search "Hives" redirects here. For other uses, see Hive. Urticaria Classification and external resourcesICD-10L50.ICD- 9708DiseasesDB13606MedlinePlus000845eMedicineemerg/628 MeSHD014581Urtic aria (or hives) is a skin condition, commonly caused by an allergic reaction, that is characterized by raised red skin wheals (welts). It is also known as nettle rash or uredo. Wheals from urticaria can appear anywhere on the body, including the face, lips, tongue, throat, and ears. The wheals may vary in size from about 5 mm (0.2 inches) in diameter to the size of a dinner plate; they typically itch severely, sting, or burn, and often have a pale border. Urticaria is generally caused by direct contact with an allergenic substance, or an immune response to food or some other allergen, but can also appear for other reasons, notably emotional stress. The rash can be triggered by quite innocent events, such as mere rubbing or exposure to cold. Contents [hide] * 1 Pathophysiology * 2 Differential diagnosis * 3 Types * 4 Related conditions * 5 Treatment and management o 5.1 Histamine antagonists o 5.2 Other o 5.3 Dietary * 6 See also * 7 References * 8 External links [edit] Pathophysiology Allergic urticaria on the shin induced by an antibiotic The skin lesions of urticarial disease are caused by an inflammatory reaction in the skin, causing leakage of capillaries in the dermis, and resulting in an edema which persists until the interstitial fluid is absorbed into the surrounding cells. Urticarial disease is thought to be caused by the release of histamine and other mediators of inflammation (cytokines) from cells in the skin. -

Skin Manifestations of Illicit Drug Use Manifestações Cutâneas
RevABDV81N4.qxd 12.08.06 13:10 Page 307 307 Educação Médica Continuada Manifestações cutâneas decorrentes do uso de drogas ilícitas Skin manifestations of illicit drug use Bernardo Gontijo 1 Flávia Vasques Bittencourt 2 Lívia Flávia Sebe Lourenço 3 Resumo: O uso e abuso de drogas ilícitas é um problema significativo e de abrangência mun- dial. A Organização das Nações Unidas estima que 5% da população mundial entre os 15 e 64 anos fazem uso de drogas pelo menos uma vez por ano (prevalência anual), sendo que meta- de destes usam regularmente, isto é, pelo menos uma vez por mês. Muitos dos eventos adver- sos das drogas ilícitas surgem na pele, o que torna fundamental que o dermatologista esteja familiarizado com essas alterações. Palavras-chave: Drogas ilícitas; Drogas ilícitas/história; Drogas ilícitas/efeitos adversos; Pele; Revisão Abstract: Illicit drug use and abuse is a major problem all over the world. The United Nations estimates that 5% of world population (aged 15-64 years) use illicit drugs at least once a year (annual prevalence) and half of them use drugs regularly, that is, at least once a month. Many adverse events of illicit drugs arise on the skin and therefore dermatologists should be aware of these changes. Keywords: Street drugs; Street drugs/history; Street drugs/adverse effects; Skin; Review HISTÓRICO Há mais de cinco mil anos na Mesopotâmia, minorar o sofrimento dos condenados. região onde hoje se situa o Iraque, os poderes cal- Provavelmente seja o ópio a droga nephente à qual mantes, soníferos e anestésicos do ópio (do latim Homero se referia como “o mais poderoso destrui- opium, através do grego opion, ‘seiva, suco’) já eram dor de mágoas”.1,2 conhecidos pelos sumérios. -

Module Test № 1 on Dermatology
THE MINISTRY OF HEALTHCARE OF THE RUSSIAN FEDERATION FEDERAL STATE BUDGETARY EDUCATIONAL INSTITUTION OF HIGHER PROFESSIONAL EDUCATION PIROGOV RUSSIAN NATIONAL RESEARCH MEDICAL UNIVERSITY DEPARTMENT OF DERMATOVENEROLOGY Gaydina T.A., Dvornikov A.S., Skripkina P.A., Nazhmutdinova D.K., Heydar S.A., Arutunyan G.B., Pashinyan A.G. MODULE TEST №1 ON DERMATOLOGY FOR STUDENTS OF INSTITUTES OF HIGHER MEDICAL EDUCATION ON SPECIALTY THERAPEUTIC FACULTY DEPARTMENT OF DERMATOVENEROLOGY Moscow 2016 ISBN УДК ББК A21 Module test №1 on Dermatology for students of institutes of high medical education on specialty «Therapeutic faculty» department of dermatovenerology: manual for students for self-training//FSBEI HPE “Pirogov RNRMU” of the ministry of healthcare of the russian federation, M.: (publisher) 2016, 144 p. The manual is a part of teaching-methods on Dermatovenerology. It contains tests on Dermatology on the topics of practical sessions requiring single or multiple choice anser. The manual can be used to develop skills of students during practical sessions. It also can be used in the electronic version at testing for knowledge. The manual is compiled according to FSES on specialty “therapeutic faculty”, working programs on dermatovenerology. The manual is intended for foreign students of 3-4 courses on specialty “therapeutic faculty” and physicians for professional retraining. Authors: Gaydina T.A. – candidate of medical science, assistant of dermatovenerology department of therapeutic faculty Pirogov RNRMU Dvornikov A.S. – M.D., professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Skripkina P.A. – candidate of medical science, assistant professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Nazhmutdinova D.K. – candidate of medical science, assistant professor of dermatovenerology department of therapeutic faculty Pirogov RNRMU Heydar S.A. -
Quick Tips on Recognizing Cutaneous Manifestations of Systemic Disease
FEATURE ARTICLE 2.0 Quick Tips on Recognizing Contact Hours Cutaneous Manifestations of Systemic Disease Jennifer Cittadino ABSTRACT: Although many skin manifestations are isolated This article will concentrate on nonmalignant cutaneous to a dermatological disorder, some skin manifestations can manifestations of systemic disease. The body systems will berelatedtoadeeper,moresystemicissue.Theskinis be reviewed, and their associated skin manifestations will be related to other body systems and functions. The impor- discussed. Some of the skin manifestations can be seen in tance of being able to recognize these dermatological multiple systemic disorders, such as erythema nodosum, manifestations and associate them with potential systemic which can be seen in pulmonary disorders, collagen and disease can be a critical diagnostic tool for the practitioner. vascular disorders, and gastrointestinal disorders. Pictures Sometimes, these skin manifestations can be the first sign will be provided when possible. of an internal disease. Although challenging, recognition, prompt diagnosis, and treatment can alter the course of a CARDIOVASCULAR AND PULMONARY SYSTEM life-threatening illness. There are several general cutaneous signs of cardiovascular Key words: Cutaneous, Dermatology, Systemic, Skin disease that may commonly be seen. These findings may include edema, cyanosis, clubbing of the nails, and corneal he skin is the largest organ in the body and one arcus. The corneal arcus appears as a gray-white ring around of the most visible body systems. The skin has the cornea and correlates with age and cholesterol levels. a reciprocal relationship between what is visu- A diagonal earlobe crease is also reported to be a marker for alized on the surface and what is occurring coronary artery disease (Uliasz & Lebwohl, 2008). -

Etiology, Classification, and Treatment of Urticaria
CONTINUING MEDICAL EDUCATION Etiology, Classification, and Treatment of Urticaria Kjetil Kristoffer Guldbakke, MD; Amor Khachemoune, MD, CWS GOAL To understand urticaria to better manage patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Discuss the clinical classification of urticaria. 2. Recognize how to diagnose urticaria. 3. Identify treatment options. CME Test on page 50. This article has been peer reviewed and approved Einstein College of Medicine is accredited by by Michael Fisher, MD, Professor of Medicine, the ACCME to provide continuing medical edu- Albert Einstein College of Medicine. Review date: cation for physicians. December 2006. Albert Einstein College of Medicine designates This activity has been planned and imple- this educational activity for a maximum of 1 AMA mented in accordance with the Essential Areas PRA Category 1 CreditTM. Physicians should only and Policies of the Accreditation Council for claim credit commensurate with the extent of their Continuing Medical Education through the participation in the activity. joint sponsorship of Albert Einstein College of This activity has been planned and produced in Medicine and Quadrant HealthCom, Inc. Albert accordance with ACCME Essentials. Drs. Guldbakke and Khachemoune report no conflict of interest. The authors discuss off-label use of colchi- cine, cyclophosphamide, cyclosporine, dapsone, intravenous immunoglobulin, methotrexate, montelukast sodium, nifedipine, plasmapheresis, rofecoxib, sulfasalazine, tacrolimus, thyroxine, and zafirlukast. Dr. Fisher reports no conflict of interest. Urticaria is among the most common skin dis- autoimmune mechanisms are now recognized as a eases. It can be acute, chronic, mediated by a cause of chronic urticaria. A search of the PubMed physical stimulus, or related to contact with an database (US National Library of Medicine) for urticant. -

Local Heat Urticaria
Volume 23 Number 12 | December 2017 Dermatology Online Journal || Case Presentation DOJ 23 (12): 10 Local heat urticaria Forrest White MD, Gabriela Cobos MD, and Nicholas A Soter MD Affiliations: 1 New York University Langone Health, New York Abstract PHYSICAL EXAMINATION: A brisk, mechanical stroke elicited a linear wheal. Five minutes after exposure We present a 38-year-old woman with local heat to hot water, she developed well-demarcated, urticaria confirmed by heat provocation testing. Heat erythematous blanching wheals that covered the urticaria is a rare form of physical urticaria that is distal forearm and entire hand. triggered by exposure to a heat source, such as hot water or sunlight. Although it is commonly localized Conclusion and immediate, generalized and delayed onset forms Physical or inducible urticarias are a group of exist. Treatment options include antihistamines urticarias that are triggered by various external and heat desensitization. A brisk, mechanical stroke physical stimuli, such as mechanical stimuli, pressure, elicited a linear wheal. Five minutes after exposure cold, light, or temperature change. Urticarias due to hot water, she developed well-demarcated, to temperature change include heat urticaria (HU), erythematous blanching wheals that covered the cholinergic urticaria, and cold urticaria. distal forearm and entire hand. HU is a rare form of chronic inducible urticaria, with Keywords: urticaria, local heat urticaria, physical approximately 60 reported cases [1]. In HU, contact urticaria with a heat source such as hot water, sunlight, hot air, radiant heat, or hot objects results in wheal formation Introduction HISTORY: A 38-year-old woman presented to the Skin and Cancer Unit for the evaluation of recurrent, intensely pruritic eruptions that were precipitated by exposure to heat, which included hot water and sunlight. -

(MPN) Symptoms
RECOGNIZING SYMPTOMS RECOGNIZING YOUR MPN SYMPTOMS The MPN LANDMARK SURVEY* is a large-scale analysis of patients with myeloproliferative neoplasms (MPNs) and Healthcare Professionals (HCPs) who treat these rare, chronic blood cancers (813 patients; 457 hematologists/oncologists). The results from LANDMARK provide new information that validates previous findings about the effect of MPN symptoms and their impact on the lives of patients, even those with low-risk MPNs. Fatigue is a symptom of particular note. Across diseases it was reported as the most common and severe symptom, and the one that patients most wanted to resolve. Symptoms such as fatigue can be vague and challenging to quantify. It is difficult to measure tiredness and its impact on daily life. In addition to physical symptoms, patients in the survey reported emotional difficulties—feeling irritable, angry or depressed. Many patients surveyed suffered with their MPN symptoms for a year or more before diagnosis. LANDMARK helps to confirm that MPN symptoms have a significant, negative impact on daily activities and quality of life, often resulting in limited or canceled family and/or social activities. For some, it means having to miss days from work, reduce hours, or even leave their job. These issues create stress, anxiety, and financial hardship for MPN patients. This information is intended to help patients validate the impact of MPN symptoms and know that they are not alone. SYMPTOM RECOGNITION Patients in the survey often did not recognize the connection between certain symptoms they were experiencing and their MPN. For example, patients with MPNs often have difficulty sleeping; however, some patients who reported this symptom did not realize it was related to their MPN.