What Do We Talk About When We Talk About Disease?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Descriptive and Comparative Study of Conceptual Metaphors in Pop and Metal Lyrics
UNIVERSIDAD DE CHILE FACULTAD DE FILOSOFÍA Y HUMANIDADES DEPARTAMENTO DE LINGÜÍSTICA METAPHORS WE SING BY: A DESCRIPTIVE AND COMPARATIVE STUDY OF CONCEPTUAL METAPHORS IN POP AND METAL LYRICS. Informe final de Seminario de Grado para optar al Grado de Licenciado en Lengua y Literatura Inglesas Estudiantes: María Elena Álvarez I. Diego Ávila S. Carolina Blanco S. Nelly Gonzalez C. Katherine Keim R. Rodolfo Romero R. Rocío Saavedra L. Lorena Solar R. Manuel Villanovoa C. Profesor Guía: Carlos Zenteno B. Santiago-Chile 2009 2 Acknowledgements We would like to thank Professor Carlos Zenteno for his academic encouragement and for teaching us that [KNOWLEDGE IS A VALUABLE OBJECT]. Without his support and guidance this research would never have seen the light. Also, our appreciation to Natalia Saez, who, with no formal attachment to our research, took her own time to help us. Finally, we would like to thank Professor Guillermo Soto, whose suggestions were fundamental to the completion of this research. Degree Seminar Group 3 AGRADECIMIENTOS Gracias a mi mamá por todo su apoyo, por haberme entregado todo el amor que una hija puede recibir. Te amo infinitamente. A la Estelita, por sus sabias palabras en los momentos importantes, gracias simplemente por ser ella. A mis tías, tío y primos por su apoyo y cariño constantes. A mis amigas de la U, ya que sin ellas la universidad jamás hubiese sido lo mismo. Gracias a Christian, mi compañero incondicional de este viaje que hemos decidido emprender juntos; gracias por todo su apoyo y amor. A mi abuelo, que me ha acompañado en todos los momentos importantes de mi vida… sé que ahora estás conmigo. -

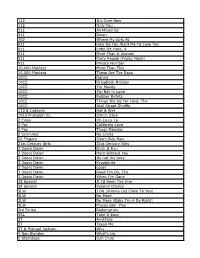
Songs by Title Karaoke Night with the Patman
Songs By Title Karaoke Night with the Patman Title Versions Title Versions 10 Years 3 Libras Wasteland SC Perfect Circle SI 10,000 Maniacs 3 Of Hearts Because The Night SC Love Is Enough SC Candy Everybody Wants DK 30 Seconds To Mars More Than This SC Kill SC These Are The Days SC 311 Trouble Me SC All Mixed Up SC 100 Proof Aged In Soul Don't Tread On Me SC Somebody's Been Sleeping SC Down SC 10CC Love Song SC I'm Not In Love DK You Wouldn't Believe SC Things We Do For Love SC 38 Special 112 Back Where You Belong SI Come See Me SC Caught Up In You SC Dance With Me SC Hold On Loosely AH It's Over Now SC If I'd Been The One SC Only You SC Rockin' Onto The Night SC Peaches And Cream SC Second Chance SC U Already Know SC Teacher, Teacher SC 12 Gauge Wild Eyed Southern Boys SC Dunkie Butt SC 3LW 1910 Fruitgum Co. No More (Baby I'm A Do Right) SC 1, 2, 3 Redlight SC 3T Simon Says DK Anything SC 1975 Tease Me SC The Sound SI 4 Non Blondes 2 Live Crew What's Up DK Doo Wah Diddy SC 4 P.M. Me So Horny SC Lay Down Your Love SC We Want Some Pussy SC Sukiyaki DK 2 Pac 4 Runner California Love (Original Version) SC Ripples SC Changes SC That Was Him SC Thugz Mansion SC 42nd Street 20 Fingers 42nd Street Song SC Short Dick Man SC We're In The Money SC 3 Doors Down 5 Seconds Of Summer Away From The Sun SC Amnesia SI Be Like That SC She Looks So Perfect SI Behind Those Eyes SC 5 Stairsteps Duck & Run SC Ooh Child SC Here By Me CB 50 Cent Here Without You CB Disco Inferno SC Kryptonite SC If I Can't SC Let Me Go SC In Da Club HT Live For Today SC P.I.M.P. -

Living with Sjögren's
Volume 35, Issue 8 September 2017 SjogrensSyndromeFoundation @SjogrensOrg Living with Sjögren’s by Darlene F. Cross, MS, LMFT patient has an illness, but a person has a life. For some of us, including many if not most Sjögren’s patients, keeping a A healthy balance between the two can be a demanding and relentless job. Realistically working to understand what we are each similarly and uniquely facing is the first step to managing the challeng- es, instead of letting the challenges manage us. Logically much of our attention is focused on the medical aspects of our illness, from the scavenger hunt of finding good answers, to putting together an effective healthcare team, to executing the treatment plan. The medical costs of illness are tangible, measurable, often helpful and sometimes not. What seems to get lost all too often is what is not tan- gible or easily measured, namely the emotional expense of living with chronic illness. While emotions did not cause the illness, they have a lot to say about how we live with it. continued page 2 t e’ve all heard it… You don’t look sick. When you live You Don’t Look Sick! with an autoimmune disease, this comment is com- How Do you Respond to this Comment? Wmon. How do you react and then respond? by Janet Church, Entrepreneur, tech-industry veteran, There are times when I’m happy to hear this comment and Sjögren’s patient and Chair-elect of the SSF Board of Directors times when I’m displeased. I do have a prepared response for this continued page 6 t In This Issue 4 You Stood Up 11 In Memory/In Honor 12 Tracking Your Symptoms 15 10 Tips for Caregivers 2 September 2017 / The Moisture Seekers “Living with Sjögren’s” continued from page 1 t Losses from Chronic Illness Time spent in waiting rooms and medical appointments is time lost Founded by Elaine K. -

Songs by Title
16,341 (11-2020) (Title-Artist) Songs by Title 16,341 (11-2020) (Title-Artist) Title Artist Title Artist (I Wanna Be) Your Adams, Bryan (Medley) Little Ole Cuddy, Shawn Underwear Wine Drinker Me & (Medley) 70's Estefan, Gloria Welcome Home & 'Moment' (Part 3) Walk Right Back (Medley) Abba 2017 De Toppers, The (Medley) Maggie May Stewart, Rod (Medley) Are You Jackson, Alan & Hot Legs & Da Ya Washed In The Blood Think I'm Sexy & I'll Fly Away (Medley) Pure Love De Toppers, The (Medley) Beatles Darin, Bobby (Medley) Queen (Part De Toppers, The (Live Remix) 2) (Medley) Bohemian Queen (Medley) Rhythm Is Estefan, Gloria & Rhapsody & Killer Gonna Get You & 1- Miami Sound Queen & The March 2-3 Machine Of The Black Queen (Medley) Rick Astley De Toppers, The (Live) (Medley) Secrets Mud (Medley) Burning Survivor That You Keep & Cat Heart & Eye Of The Crept In & Tiger Feet Tiger (Down 3 (Medley) Stand By Wynette, Tammy Semitones) Your Man & D-I-V-O- (Medley) Charley English, Michael R-C-E Pride (Medley) Stars Stars On 45 (Medley) Elton John De Toppers, The Sisters (Andrews (Medley) Full Monty (Duets) Williams, Sisters) Robbie & Tom Jones (Medley) Tainted Pussycat Dolls (Medley) Generation Dalida Love + Where Did 78 (French) Our Love Go (Medley) George De Toppers, The (Medley) Teddy Bear Richard, Cliff Michael, Wham (Live) & Too Much (Medley) Give Me Benson, George (Medley) Trini Lopez De Toppers, The The Night & Never (Live) Give Up On A Good (Medley) We Love De Toppers, The Thing The 90 S (Medley) Gold & Only Spandau Ballet (Medley) Y.M.C.A. -
112 It's Over Now 112 Only You 311 All Mixed up 311 Down
112 It's Over Now 112 Only You 311 All Mixed Up 311 Down 702 Where My Girls At 911 How Do You Want Me To Love You 911 Little Bit More, A 911 More Than A Woman 911 Party People (Friday Night) 911 Private Number 10,000 Maniacs More Than This 10,000 Maniacs These Are The Days 10CC Donna 10CC Dreadlock Holiday 10CC I'm Mandy 10CC I'm Not In Love 10CC Rubber Bullets 10CC Things We Do For Love, The 10CC Wall Street Shuffle 112 & Ludacris Hot & Wet 1910 Fruitgum Co. Simon Says 2 Evisa Oh La La La 2 Pac California Love 2 Pac Thugz Mansion 2 Unlimited No Limits 20 Fingers Short Dick Man 21st Century Girls 21st Century Girls 3 Doors Down Duck & Run 3 Doors Down Here Without You 3 Doors Down Its not my time 3 Doors Down Kryptonite 3 Doors Down Loser 3 Doors Down Road I'm On, The 3 Doors Down When I'm Gone 38 Special If I'd Been The One 38 Special Second Chance 3LW I Do (Wanna Get Close To You) 3LW No More 3LW No More (Baby I'm A Do Right) 3LW Playas Gon' Play 3rd Strike Redemption 3SL Take It Easy 3T Anything 3T Tease Me 3T & Michael Jackson Why 4 Non Blondes What's Up 5 Stairsteps Ooh Child 50 Cent Disco Inferno 50 Cent If I Can't 50 Cent In Da Club 50 Cent In Da Club 50 Cent P.I.M.P. (Radio Version) 50 Cent Wanksta 50 Cent & Eminem Patiently Waiting 50 Cent & Nate Dogg 21 Questions 5th Dimension Aquarius_Let the sunshine inB 5th Dimension One less Bell to answer 5th Dimension Stoned Soul Picnic 5th Dimension Up Up & Away 5th Dimension Wedding Blue Bells 5th Dimension, The Last Night I Didn't Get To Sleep At All 69 Boys Tootsie Roll 8 Stops 7 Question -

Songs by Artist
Sound Master Entertianment Songs by Artist smedenver.com Title Title Title .38 Special 2Pac 4 Him Caught Up In You California Love (Original Version) For Future Generations Hold On Loosely Changes 4 Non Blondes If I'd Been The One Dear Mama What's Up Rockin' Onto The Night Thugz Mansion 4 P.M. Second Chance Until The End Of Time Lay Down Your Love Wild Eyed Southern Boys 2Pac & Eminem Sukiyaki 10 Years One Day At A Time 4 Runner Beautiful 2Pac & Notorious B.I.G. Cain's Blood Through The Iris Runnin' Ripples 100 Proof Aged In Soul 3 Doors Down That Was Him (This Is Now) Somebody's Been Sleeping Away From The Sun 4 Seasons 10000 Maniacs Be Like That Rag Doll Because The Night Citizen Soldier 42nd Street Candy Everybody Wants Duck & Run 42nd Street More Than This Here Without You Lullaby Of Broadway These Are Days It's Not My Time We're In The Money Trouble Me Kryptonite 5 Stairsteps 10CC Landing In London Ooh Child Let Me Be Myself I'm Not In Love 50 Cent We Do For Love Let Me Go 21 Questions 112 Loser Disco Inferno Come See Me Road I'm On When I'm Gone In Da Club Dance With Me P.I.M.P. It's Over Now When You're Young 3 Of Hearts Wanksta Only You What Up Gangsta Arizona Rain Peaches & Cream Window Shopper Love Is Enough Right Here For You 50 Cent & Eminem 112 & Ludacris 30 Seconds To Mars Patiently Waiting Kill Hot & Wet 50 Cent & Nate Dogg 112 & Super Cat 311 21 Questions All Mixed Up Na Na Na 50 Cent & Olivia 12 Gauge Amber Beyond The Grey Sky Best Friend Dunkie Butt 5th Dimension 12 Stones Creatures (For A While) Down Aquarius (Let The Sun Shine In) Far Away First Straw AquariusLet The Sun Shine In 1910 Fruitgum Co. -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -

With Lead Vocal) Song Package
2389 Multiplex (with lead vocal) song package This song package is made available from CAVS Download Service . Update 2011/07/01 Title Artist 07/24 KEVON EDMONDS 98.6 KEITH 1985 BOWLING FOR SOUP (YOU DRIVE ME) CRAZY BRITNEY SPEARS 13TH, THE CURE, THE 4 MINUTES AVANT 4 SEASONS OF LONELINESS BOYZ II MEN 4TH OF JULY SHOOTER JENNINGS 99 RED BALLOONS NENA 99.9% SURE BRIAN MCCOMAS A A PICTURE OF ME (WITHOUT YOU) GEORGE JONES AARON'S PARTY (COME GET IT) CARTER, AARON ABACAB GENESIS ABC JACKSON 5 ABIDE WITH ME TRADITIONAL ABSOLUTELY (STORY OF A GIRL) NINE DAYS ACE IN THE HOLE STRAIT, GEORGE ACHY BREAKY HEART BILLY RAY CYRUS ACHY BREAKY SONG WEIRD AL YANKOVIC ADAM'S SONG BLINK 182 ADDICTED SIMPLE PLAN ADDICTED TO LOVE ROBERT PALMER ADRIENNE CALLING, THE AFFAIR OF THE HEART SPRINGFIELD, RICK AFTER CLOSING TIME HOUSTON, DAVID / MANDRELL, BARBARA AFTER ME SALIVA AFTER MIDNIGHT ERIC CLAPTON AGAINST ALL ODDS PHIL COLLINS AGAINST ALL ODDS (2000) MARIAH CAREY AGE AIN'T NOTHING BUT A NUMBER AALIYAH AIN'T LOVE A BITCH STEWART, ROD AIN'T NO MOUNTAIN HIGH ENOUGH MARVIN GAYE/T. TERRELL AIN'T NO STOPPIN' US NOW MCFADDEN & WHITEHEAD AIN'T NO SUNSHINE (1971) WITHERS, BILL AIN'T NO SUNSHINE (1972) JACKSON, MICHAEL AIN'T NO WOMAN LIKE THE ONE I'VE GOT FOUR TOPS AIN'T NOTHING LIKE THE REAL THING GILL, VINCE / KNIGHT, GLADYS AIN'T THAT A SHAME FATS DOMINO AIN'T THAT PECULIAR GAYE, MARVIN AIN'T TOO PROUD TO BEG TEMPTATIONS, THE ALFIE ALLEN, LILY ALIENS EXIST BLINK 182 ALL ALONE AM I LEE, BRENDA ALL BY MYSELF DION/ CELION ALL DOWNHILL FROM HERE NEW FOUND GLORY ALL -

Karaoke with a Message – August 16, 2019 – 8:30PM
Another Protest Song: Karaoke with a Message – August 16, 2019 – 8:30PM a project of Angel Nevarez and Valerie Tevere for SOMA Summer 2019 at La Morenita Canta Bar (Puente de la Morena 50, 11870 Ciudad de México, MX) karaoke provided by La Morenita Canta Bar songbook edited by Angel Nevarez and Valerie Tevere ( ) 18840 (Ghost) Riders In The Sky Johnny Cash 10274 (I Am Not A) Robot Marina & Diamonds 00005 (I Can't Get No) Satisfaction Rolling Stones 17636 (I Hate) Everything About You Three Days Grace 15910 (I Want To) Thank You Freddie Jackson 05545 (I'm Not Your) Steppin' Stone Monkees 06305 (It's) A Beautiful Mornin' Rascals 19116 (Just Like) Starting Over John Lennon 15128 (Keep Feeling) Fascination Human League 04132 (Reach Up For The) Sunrise Duran Duran 05241 (Sittin' On) The Dock Of The Bay Otis Redding 17305 (Taking My) Life Away Default 15437 (Who Says) You Can't Have It All Alan Jackson # 07630 18 'til I Die Bryan Adams 20759 1994 Jason Aldean 03370 1999 Prince 07147 2 Legit 2 Quit MC Hammer 18961 21 Guns Green Day 004-m 21st Century Digital Boy Bad Religion 08057 21 Questions 50 Cent & Nate Dogg 00714 24 Hours At A Time Marshall Tucker Band 01379 25 Or 6 To 4 Chicago 14375 3 Strange Days School Of Fish 08711 4 Minutes Madonna 08867 4 Minutes Madonna & Justin Timberlake 09981 4 Minutes Avant 18883 5 Miles To Empty Brownstone 13317 500 Miles Peter Paul & Mary 00082 59th Street Bridge Song Simon & Garfunkel 00384 9 To 5 Dolly Parton 08937 99 Luftballons Nena 03637 99 Problems Jay-Z 03855 99 Red Balloons Nena 22405 1-800-273-8255 -
The Memphis and Shelby County Room Music Listening Station Guide
The Memphis and Shelby County Room Music Listening Station Guide 1 The Memphis and Shelby County Room Music Listening Station Guide Instructions for Use Sign in at the Reference Desk for a pair of headphones Use this Guide to determine which album(s) you would like to listen to Power on the Receiver and the CD Changer Use the scroll wheel to select you album Push “Play” If others are waiting to listen, please limit your time to 2 hours After listening, turn off the Changer/ Receiver and return headphones to the Reference Desk Please do not open the Disc Changer or change any settings on the Changer or Receiver 2 CD Genre Artist Album Title Track Listing # Memphis blues / W. C. Handy - Tiger rag / D. J. LaRocca - Good news / Traditional spiritual, arr. Allen Todd II - A mess of blues / D. Pomus and M. Shuman - Let's stay together / Willie Mitchell, Al Green, Al Jackson - Fight song / Tom Ferguson - String quartet no.3, DRequiem : Oro Supplex/Lacrimosa ; Dies irae / John Baur - Ol' man The University 90 Years of making music river / Jerome Kern, arr. by James Richens - Allie call the beasts : Allie ; To be called Classical of Memphis in Memphis The 1 a bear / John David Peterson - Tender land : Stomp your foot upon the floor / Aaron Band University of Memphis Copland - I'm in trouble / Joe Hicks - MKG variations / Kamran Ince - Pockets : Three solos for double bass : number 1 / John Elmquist - Scherzo no.3 in c-sharp minor, op.39 / Frederic Chopin - Brass quintet : Intrada ; Finale / James Richens - Lucia di Lamermoor / Chi me frena in tal momento / Gaetano Donizetti. -

Dave Stamey Cover by Greg Locke Kids Welcome, Food Vendors, Beer Tent, Dealership Hours T Mark Your Calendar - Brandtoberfest Here October 8Th
AUG. 4-10, 2016 FACEBOOK.COM/WHATZUPFORTWAYNE WWW.WHATZUP.COM 2 ----------------------------------------------------------------------------------- www.whatzup.com ---------------------------------------------------------------August 4, 2016 whatzup Volume 21, Number 1 o much to see and do, so little space in which to explain it all to you. You can get an idea of just how much there is just by glancing down at the contents below – every kind of rock n’ roll you could possibly imag- Sine along with comedy, community theatre and much more. Kudos to the Fort Wayne folks who have made this plethora of entertainment options possible – because in 20 years of publishing northeast Indiana’s free- distribution arts and entertainment weekly, we’ve never seen a summer quite like this one. What’s most impressive is that it’s obvious these folks are nowhere close to being done. Witness a new column from Steve Penhollow, Fort Forward, which will keep whatzup readers apprised of the many community and cultural enhancements in various stages of development. His inaugural column features various community leaders’ attempt to create a “destination festival” (think Lollapalooza) in downtown Fort Wayne. So whether your bag is KISS, Jim Gaffigan, Ratt, cowboy singers, tributes to pop stars, dinner theater or – well, you get the gist – you’re going to find something worth doing in these pages. The next step is to go out and do it. All we ask in return for bringing you all this is for you to tell ’em whatzup sent you. inside the issue • features FORT FORWARD ............................. 14 Creating a ‘Destination Festival’ ROAD NOTEZ .................................. 16 KISS ..............................................................4 Rock N’ Roll Road Warriors FLIX ................................................ -

Top Songs of the 2000'S.Pages
Top Songs of the 2000ʼs 1. Somebody Told Me - 21. White People For 40. Read My Mind - The The Killers Peace - Against Me! Killers 2. In The End - Linkin 22. I'm Shipping Up to 41. Rooftops - Park Boston - Dropkick Lostprophets 3. Los Angeles is Burning Murphys 42. Maybe Tomorrow - - Bad Religion 23. Falling Down - Stereophonics 4. Headstrong - Trapt Atreyu 43. Far Behind - Social 5. Thrash Unreal - 24. Fix You - Coldplay Distortion Against Me! 25. Knights of Cydonia - 44. Big Casino - Jimmy 6. Viva La Vida - Coldplay Muse Eat World 7. All These Things That 26. Somewhere Else - 45. A Different Kind of I've Done - The Killers Razorlight Pain - Cold 8. One Step Closer - 27. I Believe in a Thing 46. Straight Out of Line - Linkin Park Called Love - The Godsmack 9. The '59 Sound - Darkness 47. Somewhere I Belong Gaslight Anthem 28. Human - The Killers - Linkin Park 10. Mr. Brightside - The 29. Audience of One - 48. We're All To Blame - Killers Rise Against Sum 41 11. Walk Away - 30. America - Razorlight 49. Sex On Fire - Kings of Dropkick Murphys 31. Smokers Outside the Leon 12. Re-Education Hospital Doors - Editors 50. Anthem - Zebrahead (Through Labor) - Rise 32. Island in the Sun - 51. Dashboard - Modest Against Weezer Mouse 13. Munich - Editors 33. Crawling - Linkin 52. Beverly Hills - Weezer 14. Use Somebody - Park 53. Take Me Out - Franz Kings of Leon 34. Who's Gonna Save Ferdinand 15. Clocks - Coldplay Us - The Living End 54. Savior - Rise Against 16. When You Were 35. Sunshine Highway - 55. In the Morning - Young - The Killers Dropkick Murphys Razorlight 17.