Powerpoint Handout: Lab 1, Musculoskeletal Pelvis, Perineum and Urinary System Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -
MALE REPRODUCTIVE SYSTEM Male Reproduc�Ve System
Human Anatomy Unit 3 MALE REPRODUCTIVE SYSTEM Male Reproducve System • Gonads = testes – primary organ responsible for sperm producon – development/ maintenance of secondary sex characteriscs • Gametes = sperm Male Reproducve System Anatomy of the Testes • Tunica albuginea • Seminiferous tubules – highly coiled – sealed by the blood tess barrier – Site of sperm producon • located in tescular lobules Anatomy of the Testes Histology of the Testes • Intersal cells of Leydig – Intersal endocrinocytes – Located between seminiferous tubules – testosterone • Sertoli cells – Nursing cells or sustentacular cells – form the blood tess barrier – support sperm development Development of Sperm • Sperm formed by two processes – meiosis • Cell division resulng in cells with genecally varied cells with only one complete set of DNA (remember…our cells have two complete sets!) – spermatogenesis • morphological changes as sperm develop in tubule system • 64 days in humans – Can survive 3 days in female reproducve tract Development of Sperm The Long and Winding Road… • Seminiferous tubules • Rete tess • Epididymis • Vas deferens • Ejaculatory duct • Prostac urethra • Membranous urethra • Penile urethra The Epididymis • Sperm “swim school” • Comma shaped organ that arches over the posterior and lateral side of the tess • Stores spermatozoa unl ejaculaon or absorpon • Sperm stored for up to 2 weeks Vas Deferens • Extends from the epididymis • Passes posterior to the urinary bladder • Meets the spermac blood vessels to become the spermac cord • Enters -

1 Male Checklist Male Reproductive System Components of the Male
Male Checklist Male Reproductive System Components of the male Testes; accessory glands and ducts; the penis; and reproductive system the scrotum. Functions of the male The male reproductive system produces sperm cells that reproductive system can be transferred to the female, resulting in fertilization and the formation of a new individual. It also produces sex hormones responsible for the normal development of the adult male body and sexual behavior. Penis The penis functions as the common outlet for semen (sperm cells and glandular secretions) and urine. The penis is also the male copulatory organ, containing tissue that can fill with blood resulting in erection of the penis. Prepuce A fold of skin over the distal end of the penis. Circumcision is the surgical removal of the prepuce. Corpus spongiosum A spongy body consisting of erectile tissue. It surrounds the urethra. Sexual excitement can cause erectile tissue to fill with blood. As a result, the penis becomes erect. Glans penis The expanded, distal end of the corpus spongiosum. It is also called the head of the penis. Bulb of the penis The proximal end of the corpus spongiosum. Bulbospongiosus muscle One of two skeletal muscles surrounding the bulb of the penis. At the end of urination, contraction of the bulbospongiosus muscles forces any remaining urine out of the urethra. During ejaculation, contractions of the bulbospongiosus muscles ejects semen from the penis. Contraction of the bulbospongiosus muscles compresses the corpus spongiosum, helping to maintain an erection. Corpus cavernosum One of two spongy bodies consisting of erectile tissue that (pl., corpora cavernosa) form the sides and front of the penis. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Advanced Retroperitoneal Anatomy Andneuro-Anatomy of Thepelvis
APRIL 21-23 • 2016 • ST. LOUIS, MISSOURI, USA Advanced Retroperitoneal Anatomy and Neuro-Anatomy of the Pelvis Hands-on Cadaver Workshop with Focus on Complication Prevention in Minimally Invasive Surgery in Endometriosis, Urogynecology and Oncology WITH ICAPS FACULTY Nucelio Lemos, MD, PhD (Course Chair) Adrian Balica, MD (Course Co-Chair) Eugen Campian, MD, PhD Vadim Morozov, MD Jonathon Solnik, MD, FACOG, FACS An offering through: Practical Anatomy & Surgical Education Department of Surgery, Saint Louis University School of Medicine http://pa.slu.edu COURSE DESCRIPTION • Demonstrate the topographic anatomy of the pelvic sidewall, CREDIT DESIGNATION: This theoretical and cadaveric course is designed for both including vasculature and their relation to the ureter, autonomic Saint Louis University designates this live activity for a maximum intermediate and advanced laparoscopic gynecologic surgeons and somatic nerves and intraperitoneal structures; of 20.5 AMA PRA Category 1 Credit(s) ™. and urogynecologists who want to practice and improve their • Discuss steps of safe laparoscopic dissection of the pelvic ureter; laparoscopic skills and knowledge of retroperitoneal anatomy. • Distinguish and apply steps of safe and effective pelvic nerve Physicians should only claim credit commensurate with the The course will be composed of 3 full days of combined dissection and learn the landmarks for nerve-sparing surgery. extent of their participation in the activity. theoretical lectures on Surgical Anatomy and Pelvic Neuroanatomy with hands on practice of laparoscopic and ACCREDITATION: REGISTRATION / TUITION FEES transvaginal dissection. Saint Louis University School of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) Early Bird (up to Dec. 31st) ...........US ....$2,295 COURSE OBJECTIVES to provide continuing medical education for physicians. -

The Reproductive System
27 The Reproductive System PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • Overview of the Male Reproductive System • Testis • Epididymis • Ductus deferens • Ejaculatory duct • Spongy urethra (penile urethra) • Seminal gland • Prostate gland • Bulbo-urethral gland © 2012 Pearson Education, Inc. Figure 27.1 The Male Reproductive System, Part I Pubic symphysis Ureter Urinary bladder Prostatic urethra Seminal gland Membranous urethra Rectum Corpus cavernosum Prostate gland Corpus spongiosum Spongy urethra Ejaculatory duct Ductus deferens Penis Bulbo-urethral gland Epididymis Anus Testis External urethral orifice Scrotum Sigmoid colon (cut) Rectum Internal urethral orifice Rectus abdominis Prostatic urethra Urinary bladder Prostate gland Pubic symphysis Bristle within ejaculatory duct Membranous urethra Penis Spongy urethra Spongy urethra within corpus spongiosum Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Scrotum Testis © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body -

Male Reproductive System
MALE REPRODUCTIVE SYSTEM DR RAJARSHI ASH M.B.B.S.(CAL); D.O.(EYE) ; M.D.-PGT(2ND YEAR) DEPARTMENT OF PHYSIOLOGY CALCUTTA NATIONAL MEDICAL COLLEGE PARTS OF MALE REPRODUCTIVE SYSTEM A. Gonads – Two ovoid testes present in scrotal sac, out side the abdominal cavity B. Accessory sex organs - epididymis, vas deferens, seminal vesicles, ejaculatory ducts, prostate gland and bulbo-urethral glands C. External genitalia – penis and scrotum ANATOMY OF MALE INTERNAL GENITALIA AND ACCESSORY SEX ORGANS SEMINIFEROUS TUBULE Two principal cell types in seminiferous tubule Sertoli cell Germ cell INTERACTION BETWEEN SERTOLI CELLS AND SPERM BLOOD- TESTIS BARRIER • Blood – testis barrier protects germ cells in seminiferous tubules from harmful elements in blood. • The blood- testis barrier prevents entry of antigenic substances from the developing germ cells into circulation. • High local concentration of androgen, inositol, glutamic acid, aspartic acid can be maintained in the lumen of seminiferous tubule without difficulty. • Blood- testis barrier maintains higher osmolality of luminal content of seminiferous tubules. FUNCTIONS OF SERTOLI CELLS 1.Germ cell development 2.Phagocytosis 3.Nourishment and growth of spermatids 4.Formation of tubular fluid 5.Support spermiation 6.FSH and testosterone sensitivity 7.Endocrine functions of sertoli cells i)Inhibin ii)Activin iii)Follistatin iv)MIS v)Estrogen 8.Sertoli cell secretes ‘Androgen binding protein’(ABP) and H-Y antigen. 9.Sertoli cell contributes formation of blood testis barrier. LEYDIG CELL • Leydig cells are present near the capillaries in the interstitial space between seminiferous tubules. • They are rich in mitochondria & endoplasmic reticulum. • Leydig cells secrete testosterone,DHEA & Androstenedione. • The activity of leydig cell is different in different phases of life. -
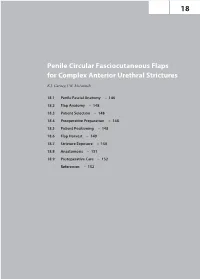
Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures K.J
18 Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures K.J. Carney, J.W. McAninch 18.1 Penile Fascial Anatomy – 146 18.2 Flap Anatomy – 148 18.3 Patient Selection – 148 18.4 Preoperative Preparation – 148 18.5 Patient Positioning – 148 18.6 Flap Harvest – 149 18.7 Stricture Exposure – 150 18.8 Anastomosis – 151 18.9 Postoperative Care – 152 References – 152 146 Chapter 18 · Penile Circular Fasciocutaneous Flaps for Complex Anterior Urethral Strictures Surgical reconstruction of complex anterior urethral stric- Buck’s fascia is a well-defined fascial layer that is close- tures, 2.5–6 cm long, frequently requires tissue-transfer ly adherent to the tunica albuginea. Despite this intimate techniques [1–8]. The most successful are full-thickness association, a definite plane of cleavage exists between the free grafts (genital skin, bladder mucosa, or buccal muco- two, permitting separation and mobilization. Buck’s fascia sa) or pedicle-based flaps that carry a skin island. Of acts as the supporting layer, providing the foundation the latter, the penile circular fasciocutaneous flap, first for the circular fasciocutaneous penile flap. Dorsally, the described by McAninch in 1993 [9], produces excel- deep dorsal vein, dorsal arteries, and dorsal nerves lie in a lent cosmetic and functional results [10]. It is ideal for groove just deep to the superficial lamina of Buck’s fascia. reconstruction of the distal (pendulous) urethra, where The circumflex vessels branch from the dorsal vasculature the decreased substance of the corpus spongiosum may and lie just deep to Buck’s fascia over the lateral aspect jeopardize graft viability. -

By Dr.Ahmed Salman Assistant Professorofanatomy &Embryology My Advice to You Is to Focus on the Diagrams That I Drew
The University Of Jordan Faculty Of Medicine REPRODUCTIVE SYSTEM By Dr.Ahmed Salman Assistant ProfessorofAnatomy &embryology My advice to you is to focus on the diagrams that I drew. These diagrams cover the Edited by Dana Hamo doctor’s ENTIRE EXPLANATION AND WHAT HE HAS MENTIONED Quick Recall : Pelvic brim Pelvic diaphragm that separates the true pelvis above and perineum BELOW Perineum It is the diamond-shaped lower end of the trunk Glossary : peri : around, ineo - discharge, evacuate Location : it lies below the pelvic diaphragm, between the upper parts of the thighs. Boundaries : Anteriorly : Inferior margin of symphysis pubis. Posteriorly : Tip of coccyx. Anterolateral : Fused rami of pubis and ischium and ischial tuberosity. Posterolateral : Sacrotuberous ligaments. Dr.Ahmed Salman • Same boundaries as the pelvic Anteriorly: outlet. inferior part of • If we drew a line between the 2 symphysis pubis ischial tuberosities, the diamond shape will be divided into 2 triangles. Anterior and Anterior and Lateral : Lateral : •The ANTERIOR triangle is called ischiopubic ischiopubic urogenital triangle ramus The perineum ramus •The POSTERIOR triangle is called has a diamond anal triangle shape. ischial tuberosity Posterior and Posterior and Lateral : Lateral : Urogenital sacrotuberous sacrotuberous tri. ligament ligament Anal tri. Posteriorly : tip of coccyx UROGENITAL TRI. ANAL TRI. Divisions of the Perineum : By a line joining the anterior parts of the ischial tuberosities, the perineum is divided into two triangles : Anteriorly :Urogenital -

6Th Advanced Retroperitoneal Anatomy and Neuro-Anatomy of the Pelvis
Session I Theoretical Lectures will be given in Portuguese and Session II Lectures in English. Session I, June 9-10 will be presented in Portugese. Optional English and Portuguese speaking Faculty are available for the practical part of both sessions. Course Description SESSION I SESSION II SESSION III This theoretical and cadaveric course is designed for both intermediate and JUNE 9 - JUNE 13 advanced laparoscopic gynecologic surgeons and urogynecologists who want to ST. LOUIS, MISSOURI, USA Tuesday, June 9 7:30 am - 5:00 pm Wednesday, June 10 7:30 am - 5:00 pm Thursday, June 11 7:30 am - 5:00 pm Friday, June 12 7:30 am - 5:00 pm Saturday, June 13 7:30 am - 4:00 pm practice and improve their laparoscopic skills and knowledge of retroperitoneal 2020 From Books to Practice Simulcast: Parallel Theoretical From Books to Practice Simulcast: Parallel Theoretical anatomy. ➢ Pelvic Neuroanatomy and the Nerve Sparing Surgical ➢ Pelvic Neuroanatomy and the Nerve Sparing Surgical ➢ Hands-on Cadaver Lab: Presentations and Live Dissection Presentations and Live Dissection The course will be composed of 2 full days of combined theoretical lectures on Concept Concept Dissection of Lateral Pelvic Sidewall, Ureter, Vessels; ➢ The Avascular Spaces of the Pelvis Surgical Anatomy and Pelvic Neuroanatomy with hands on practice of laparoscopic From Books to Practice Simulcast: Parallel Theoretical ➢ The Avascular Spaces of the Pelvis From Books to Practice Simulcast: Parallel Theoretical Development of the Obturator Space and Identification and transvaginal dissection and a third optional dissection-only day, with a new 6th Advanced Retroperitoneal Anatomy Presentations and Live Dissection ➢ Diaphragmatic Anatomy and Strategies for Diaphragmatic Presentations and Live Dissection ➢ Diaphragmatic Anatomy and Strategies for Diaphragmatic of Obturator, Sciatic, and Pudendal Nerves; Identification specimen. -

Lab #23 Anal Triangle
THE BONY PELVIS AND ANAL TRIANGLE (Grant's Dissector [16th Ed.] pp. 141-145) TODAY’S GOALS: 1. Identify relevant bony features/landmarks on skeletal materials or pelvic models. 2. Identify the sacrotuberous and sacrospinous ligaments. 3. Describe the organization and divisions of the perineum into two triangles: anal triangle and urogenital triangle 4. Dissect the ischiorectal (ischioanal) fossa and define its boundaries. 5. Identify the inferior rectal nerve and artery, the pudendal (Alcock’s) canal and the external anal sphincter. DISSECTION NOTES: The perineum is the diamond-shaped area between the upper thighs and below the inferior pelvic aperture and pelvic diaphragm. It is divided anatomically into 2 triangles: the anal triangle and the urogenital (UG) triangle (Dissector p. 142, Fig. 5.2). The anal triangle is bounded by the tip of the coccyx, sacrotuberous ligaments, and a line connecting the right and left ischial tuberosities. It contains the anal canal, which pierced the levator ani muscle portion of the pelvic diaphragm. The urogenital triangle is bounded by the ischiopubic rami to the inferior surface of the pubic symphysis and a line connecting the right and left ischial tuberosities. This triangular space contains the urogenital (UG) diaphragm that transmits the urethra (in male) and urethra and vagina (in female). A. Anal Triangle Turn the cadaver into the prone position. Make skin incisions as on page 144, Fig. 5.4 of the Dissector. Reflect skin and superficial fascia of the gluteal region in one flap to expose the large gluteus maximus muscle. This muscle has proximal attachments to the posteromedial surface of the ilium, posterior surfaces of the sacrum and coccyx, and the sacrotuberous ligament.