Vulvar Cancer Early Detection, Diagnosis, and Staging Detection and Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -

The Cyclist's Vulva
The Cyclist’s Vulva Dr. Chimsom T. Oleka, MD FACOG Board Certified OBGYN Fellowship Trained Pediatric and Adolescent Gynecologist National Medical Network –USOPC Houston, TX DEPARTMENT NAME DISCLOSURES None [email protected] DEPARTMENT NAME PRONOUNS The use of “female” and “woman” in this talk, as well as in the highlighted studies refer to cis gender females with vulvas DEPARTMENT NAME GOALS To highlight an issue To discuss why this issue matters To inspire future research and exploration To normalize the conversation DEPARTMENT NAME The consensus is that when you first start cycling on your good‐as‐new, unbruised foof, it is going to hurt. After a “breaking‐in” period, the pain‐to‐numbness ratio becomes favourable. As long as you protect against infection, wear padded shorts with a generous layer of chamois cream, no underwear and make regular offerings to the ingrown hair goddess, things are manageable. This is wrong. Hannah Dines British T2 trike rider who competed at the 2016 Summer Paralympics DEPARTMENT NAME MY INTRODUCTION TO CYCLING Childhood Adolescence Adult Life DEPARTMENT NAME THE CYCLIST’S VULVA The Issue Vulva Anatomy Vulva Trauma Prevention DEPARTMENT NAME CYCLING HAS POSITIVE BENEFITS Popular Means of Exercise Has gained popularity among Ideal nonimpact women in the past aerobic exercise decade Increases Lowers all cause cardiorespiratory mortality risks fitness DEPARTMENT NAME Hermans TJN, Wijn RPWF, Winkens B, et al. Urogenital and Sexual complaints in female club cyclists‐a cross‐sectional study. J Sex Med 2016 CYCLING ALSO PREDISPOSES TO VULVAR TRAUMA • Significant decreases in pudendal nerve sensory function in women cyclists • Similar to men, women cyclists suffer from compression injuries that compromise normal function of the main neurovascular bundle of the vulva • Buller et al. -

Pregnancy and Cesarean Delivery After Multimodal Therapy for Vulvar Carcinoma: a Case Report
MOLECULAR AND CLINICAL ONCOLOGY 5: 583-586, 2016 Pregnancy and cesarean delivery after multimodal therapy for vulvar carcinoma: A case report KUNIAKI TORIYABE1,2, HARUKI TANIGUCHI2, TOKIHIRO SENDA2,3, MASAKO NAKANO2, YOSHINARI KOBAYASHI2, MIHO IZAWA2, HIROHIKO TANAKA2, TETSUO ASAKURA2, TSUTOMU TABATA1 and TOMOAKI IKEDA1 1Department of Obstetrics and Gynecology, Mie University Graduate School of Medicine, Tsu, Mie 514-8507; 2Department of Obstetrics and Gynecology, Mie Prefectural General Medical Center, Yokkaichi, Mie 510-8561; 3Department of Obstetrics and Gynecology, Kinan Hospital, Mihama, Mie 519-5293, Japan Received November 4, 2015; Accepted September 12, 2016 DOI: 10.3892/mco.2016.1021 Abstract. Reports of pregnancy following treatment for vulvectomy, may have an increased incidence of caesarean vulvar carcinoma are extremely uncommon, as the main delivery (2). In the literature, vulvar scarring following radical problem of subsequent pregnancy is vulvar scarring following vulvectomy was the major reason for pregnant women under- radical surgery. We herein report the case of a patient who was going caesarean section (2-7). To date, no cases of pregnancy diagnosed with stage I squamous cell carcinoma of the vulva following vulvar carcinoma have been reported in patients at the age of 17 years and was treated with multimodal therapy, who had undergone surgery and radiotherapy. including neoadjuvant chemotherapy, wide local excision with We herein describe a case in which caesarean section was bilateral inguinal lymph node dissection and adjuvant radio- performed due to the presence of extensive vulvar scarring therapy. The patient became pregnant spontaneously 9 years following multimodal therapy for vulvar carcinoma, including after her initial diagnosis and the antenatal course was good, chemotherapy, surgery and radiotherapy. -
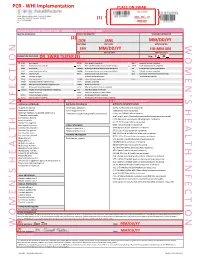
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Vaginal and Vulvar Cancer 10.1136/Ijgc-2020-ESGO.178
Int J Gynecol Cancer: first published as 10.1136/ijgc-2020-ESGO.177 on 4 December 2020. Downloaded from Abstracts 520 LONG TERM FOLLOW UP AFTER DIAGNOSIS OF Introduction/Background Since the introduction of the S2K GESTATIONAL TROPHOBLASTIC DISEASE AWMF guideline-based sentinel node biopsy technique in uni- focal vulvar cancer (diameter of <4 cm) and unsuspicious Pedro Corvelo Freitas, Beatriz Mira, António Guimarães, Ana Opinião, Hugo Nunes, Ana Francisca Jorge, Fátima Vaz, António Moreira. Instituto Português de Oncologia de Lisboa groin lymph nodes, the morbidity rate of patients has signifi- Francisco Gentil cantly decreased in Germany. The groin recurrence rate after IFL is vary from 0% to 5.8%, in contrast to 2.3% (95% CI, 10.1136/ijgc-2020-ESGO.176 0.6% to 5%) in unifocal vulvar cancer vs 3% (95% CI, 1% to 6%) in multifocal vulvar cancer after SLNB only, as sug- Introduction/Background The spectrum of Gestational tropho- gested in the GRoningen INternational Study on Sentinel blastic disease (GTD) ranges from pre-malignant conditions of node in Vulvar cancer (GROINSS-V-I) in 2008. Current guide- complete (CHM) and partial (PHM) hydatidiform moles to the lines suggest that in cases of metastasis of unilateral sentinel malignant invasive mole, choriocarcinoma (CC) and very rare lymph node (SLN) biopsy (B), groin node dissection, namely placental site trophoblastic tumour/epithelioid trophoblastic inguinofemoral lymphadenectomy (IFL), should be performed tumour (PSTT/ETT). Gestational trophoblastic neoplasia (GTN) bilaterally. However, a publication by Woelber et al. in Ger- are highly responsive to chemotherapy (CT) and with appropri- many and and Nica et al. -
Pembrolizumab in Vaginal and Vulvar Squamous Cell Carcinoma: a Case Series from a Phase II Basket Trial Jefrey A
www.nature.com/scientificreports OPEN Pembrolizumab in vaginal and vulvar squamous cell carcinoma: a case series from a phase II basket trial Jefrey A. How 1, Amir A. Jazaeri 1, Pamela T. Soliman1, Nicole D. Fleming1, Jing Gong2, Sarina A. Piha‑Paul2, Filip Janku 2, Bettzy Stephen 2 & Aung Naing 2* Vaginal and vulvar squamous cell carcinoma (SCC) are rare tumors that can be challenging to treat in the recurrent or metastatic setting. We present a case series of patients with vaginal or vulvar SCC who were treated with single‑agent pembrolizumab as part of a phase II basket clinical trial to evaluate efcacy and safety. Two cases of recurrent and metastatic vaginal SCC, with multiple prior lines of systemic chemotherapy and radiation, received pembrolizumab. One patient had signifcant reduction (81%) in target tumor lesions prior to treatment discontinuation at cycle 10 following confrmed progression of disease with new metastatic lesions (stable disease by irRECIST criteria). In contrast, the other patient with vaginal SCC discontinued treatment after cycle 3 due to disease progression. Both patients had PD‑L1 positive vaginal tumors and tolerated treatment well. One case of recurrent vulvar SCC with multiple surgical resections and prior progression on systemic carboplatin had a 30% reduction in her target tumor lesions following pembrolizumab treatment with a PD‑L1 positive tumor. Treatment was discontinued for grade 3 mucositis after cycle 5. Pembrolizumab may provide some clinical beneft to some patients with vaginal or vulvar SCC and is overall safe to utilize in this population. Future studies are needed to evaluate the efcacy of pembrolizumab in these rare tumor types and to identify predictive biomarkers of response. -

Chronic Infections of the Vulva Or Vagina
Chronic Infection Persistent or recurrent vaginal infections may cause daily or episodic symptoms of itching, irritation or burning. Not all women have persistent discharge from the vagina. Research supports that approximately 5% of women will suffer from recurrent infections. The most common recurrent infections are: 1. Yeast 2. Bacterial Vaginosis 3. Trichomonas Yeast Infection Yeast infections are common; approximately 20% of all women will experience one in their lifetime. Diabetes, pregnancy, antibiotic use and immuno-suppression are risk factors that predispose women to yeast infections. Yeast infections are not sexually transmitted. Although most women worry that their partner may be a source of re- infectivity, the penis is not a reservoir. In addition, a diet high in refined sugar does not put a woman at risk for recurrence. For some women with chronic yeast infections, the symptoms may flare at the same time during the menstrual cycle. Some experience burning with urination or vaginal dryness. Intercourse may be painful. Recurrent infection is defined as 4 infections/year. Diagnosis is made from history and physical exam. Usually a special fungal culture is obtained to identify the yeast organism. If an acute infection is occurring, this is treated aggressively for 7-14days. Treatment is administered either orally or vaginally. Boric acid, a natural acid compound, can be used to effectively treat some resistant strains of yeast. Suppression may follow after treatment for the acute infection and may be recommended for up to 6 months. Most experience relief with long-term treatment, although the recurrence rate after suppression can be as high as 30%. -

Incidence and Cost of Anal, Penile, Vaginal and Vulvar Cancer in Denmark Jens Olsen1*, Tine Rikke Jørgensen2, Kristian Kofoed3 and Helle Kiellberg Larsen3
Olsen et al. BMC Public Health 2012, 12:1082 http://www.biomedcentral.com/1471-2458/12/1082 RESEARCH ARTICLE Open Access Incidence and cost of anal, penile, vaginal and vulvar cancer in Denmark Jens Olsen1*, Tine Rikke Jørgensen2, Kristian Kofoed3 and Helle Kiellberg Larsen3 Abstract Background: Besides being a causative agent for genital warts and cervical cancer, human papillomavirus (HPV) contributes to 40-85% of cases of anal, penile, vaginal and vulvar cancer and precancerous lesions. HPV types 16 & 18 in particular contribute to 74-93% of these cases. Overall the number of new cases of these four cancers may be relatively high implying notable health care cost to society. The aim of this study was to estimate the incidence and the health care sector costs of anal, penile, vaginal and vulvar cancer. Methods: New anogenital cancer patients were identified from the Danish National Cancer Register using ICD-10 diagnosis codes. Resource use in the health care sector was estimated for the year prior to diagnosis, and for the first, second and third years after diagnosis. Hospital resource use was defined in terms of registered hospital contacts, using DRG (Diagnosis Related Groups) and DAGS (Danish Outpatient Groups System) charges as cost estimates for inpatient and outpatient contacts, respectively. Health care consumption by cancer patients diagnosed in 2004–2007 was compared with that by an age- and sex-matched cohort without cancer. Hospital costs attributable to four anogenital cancers were estimated using regression analysis. Results: The annual incidence of anal cancer in Denmark is 1.9 per 100,000 persons. The corresponding incidence rates for penile, vaginal and vulvar cancer are 1.7, 0.9 and 3.6 per 100,000 males/females, respectively. -

Vaginal Cancer, Risk Factors, and Prevention Risk Factors for Vaginal
cancer.org | 1.800.227.2345 Vaginal Cancer, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for vaginal cancer. ● Risk Factors for Vaginal Cancer ● What Causes Vaginal Cancer? Prevention There's no way to completely prevent cancer. But there are things you can do that might help lower your risk. Learn more here. ● Can Vaginal Cancer Be Prevented? Risk Factors for Vaginal Cancer A risk factor is anything that affects your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. But having a risk factor, or even many, does not mean that you will get the disease. And 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 some people who get the disease may not have any known risk factors. Scientists have found that certain risk factors make a woman more likely to develop vaginal cancer. But many women with vaginal cancer don’t have any clear risk factors. And even if a woman with vaginal cancer has one or more risk factors, it’s impossible to know for sure how much that risk factor contributed to causing the cancer. Age Squamous cell cancer of the vagina occurs mainly in older women. It can happen at any age, but few cases are found in women younger than 40. Almost half of cases occur in women who are 70 years old or older. -
NCCN Guidelines for Penile Cancer from Version 1.2019 Include
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Penile Cancer Version 2.2019 — May 13, 2019 NCCN.org Continue Version 2.2019, 05/13/19 © 2019 National Comprehensive Cancer Network® (NCCN®), All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN. NCCN Guidelines Index NCCN Guidelines Version 2.2019 Table of Contents Penile Cancer Discussion *Thomas W. Flaig, MD †/Chair Harry W. Herr, MD ϖ Sumanta K. Pal, MD † University of Colorado Cancer Center Memorial Sloan Kettering Cancer Center City of Hope National Medical Center *Philippe E. Spiess, MD, MS ϖ/Vice Chair Christopher Hoimes, MD † Anthony Patterson, MD ϖ Moffitt Cancer Center Case Comprehensive Cancer Center/ St. Jude Children’s Research Hospital/ University Hospitals Seidman Cancer Center The University of Tennessee Neeraj Agarwal, MD ‡ † and Cleveland Clinic Taussig Cancer Institute Health Science Center Huntsman Cancer Institute at the University of Utah Brant A. Inman, MD, MSc ϖ Elizabeth R. Plimack, MD, MS † Duke Cancer Institute Fox Chase Cancer Center Rick Bangs, MBA Patient Advocate Masahito Jimbo, MD, PhD, MPH Þ Kamal S. Pohar, MD ϖ University of Michigan Rogel Cancer Center The Ohio State University Comprehensive Stephen A. Boorjian, MD ϖ Cancer Center - James Cancer Hospital Mayo Clinic Cancer Center A. Karim Kader, MD, PhD ϖ and Solove Research Institute UC San Diego Moores Cancer Center Mark K. Buyyounouski, MD, MS § Michael P. Porter, MD, MS ϖ Stanford Cancer Institute Subodh M. Lele, MD ≠ Fred Hutchinson Cancer Research Center/ Fred & Pamela Buffett Cancer Center Sam Chang, MD ¶ Seattle Cancer Care Alliance Vanderbilt-Ingram Cancer Center Joshua J.