Facilitating Cross-National Comparisons of Indicators for Patient Safety at the Health-System Level in the Oecd Countries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EAACI/ESCD Skin Allergy Meeting 2017 (SAM 2017)
Clin Transl Allergy 2017, 7(Suppl 4):47 DOI 10.1186/s13601-017-0184-5 Clinical and Translational Allergy MEETING ABSTRACTS Open Access EAACI/ESCD Skin Allergy Meeting 2017 (SAM 2017) Zurich, Switzerland. 27 – 29 April 2017 Published: 15 December 2017 Thursday, 27 April 2017 O02 Assessment of aggregate consumer exposure to isothiazolinones O01 via cosmetics and detergents Methylisothiazolinone contact allergy: a real outbreak Elena Garcia Hidalgo, Natalie Von Goetz, Konrad Hungerbühler Luis Amaral1, Emidio Silva2, Marcio Oliveira3, Ana Paula Cunha4 ETH Zürich, Zürich, Switzerland 1Serviço de Imunoalergologia, Centro Hospitalar de São João E.P.E., Porto, Correspondence: Elena Garcia Hidalgo ‑ [email protected] Portugal; 2Serviço de Medicina do Trabalho e Saúde Ocupacional, Centro Clinical and Translational Allergy 2017, 7(Supple 4):O02 Hospitalar do Baixo Vouga E.P.E., Aveiro, Portugal; 3Serviço de Saúde Ocu‑ pacional, Centro Hospitalar de São João E.P.E., Porto, Portugal; 4Serviço de Background: Isothiazoliones can cause allergic contact dermati- Dermatologia, Centro Hospitalar de São João E.P.E., Porto, Portugal tis and are present in a variety of consumer products, such as cos- Correspondence: Luis Amaral ‑ [email protected] metics, detergents and do-it-yourself products. Skin sensitization Clinical and Translational Allergy 2017, 7(Supple 4):O01 is induced following dermal exposure to a sensitizer in an amount exceeding the sensitization threshold. The critical determinant of Background: Methylisothiazolinone (MI) is used as a preservative in exposure for evaluating skin sensitization risks is dose per unit area occupational, domestic products and, since 2005, in cosmetics. It is a of exposed skin. -

Hypertrichosis Terminalis
97297 Med Genet 1996;33:972-974 An autosomal dominant syndrome of acromegaloid facial appearance and generalised J Med Genet: first published as 10.1136/jmg.33.11.972 on 1 November 1996. Downloaded from Department of hypertrichosis terminalis Medical Genetics, Belfast City Hospital, Lisburn Road, Belfast BT9 7AB, Northern Ireland Alan D Irvine, Olivia M Dolan, David R Hadden, Fiona J Stewart, E Ann Bingham, A D Irvine Norman C Nevin F J Stewart N C Nevin Department of Dermatology, Royal Abstract A family with four affected subjects in three Group of Hospitals, Belfast BT12 6BA, We report a family in which a phenotype generations is reported. Affected subjects show Northern Ireland of acromegaloid facial appearance (AFA) a characteristic acromegaloid facial appearance 0 M Dolan and generalised hypertrichosis terminalis (AFA) and generalised hypertrichosis ter- E A Bingham segregates through three generations. minalis. The syndrome is inherited as an auto- Sir George E Clark Congenital hypertrichosis terminalis and somal dominant trait and appears to be fully Metabolic Unit, Royal AFA have been previously reported as in- penetrant. Acromegaloid facial appearance and Group of Hospitals, dependent autosomal dominant traits. hypertrichosis terminalis have been described Belfast BT12 6BA, Northern Ireland This is the first report to delineate an auto- in association with thickened oral mucosa and D R Hadden somal dominant transmission of the com- gingival hyperplasia.'"2 Affected patients in our Correspondence to: bined phenotype. family did not have intraoral lesions. The Dr Irvine. (JtMed Genet 1996;33:972-974) syndrome in our family appears to be discrete Received 14 May 1996 from the acromegaloid facial appearance syn- Revised version accepted for Key words: terminal hypertrichosis; acromegaloid drome,3 Gorlin-Chaudhry-Moss syndrome,4 publication 28 June 1996 facies; autosomal dominant. -

Lameness in Fattening Pigs – Mycoplasma Hyosynoviae, Osteochondropathy and Reduced Dietary Phosphorus Level As Three Infuencing Factors: a Case Report
Lameness in fattening pigs – Mycoplasma hyosynoviae, osteochondropathy and reduced dietary phosphorus level as three inuencing factors: A case report Birte Wegner Veterinary Practice Duemmerland Jörg Tenhündfeld Vetland Dr. Tenhündfeld & Kollegen Johanna Vogels Stiftung Tierarztliche Hochschule Hannover Marius Beumer Stiftung Tierarztliche Hochschule Hannover Josef Kamphues Stiftung Tierarztliche Hochschule Hannover Florian Hansmann Stiftung Tierarztliche Hochschule Hannover Hanna Rieger Stiftung Tierarztliche Hochschule Hannover Elisabeth grosse Beilage Stiftung Tierarztliche Hochschule Hannover Isabel Hennig-Pauka ( [email protected] ) University of Veterinary Medicine Hannover https://orcid.org/0000-0003-3994-5979 Case report Keywords: Locomotor disorder, mineral supply, Mycoplasma hyosynoviae, nutrition, swine Posted Date: September 25th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-35962/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/28 Version of Record: A version of this preprint was published on December 15th, 2020. See the published version at https://doi.org/10.1186/s40813-020-00184-w. Page 2/28 Abstract Background: Multiple diagnostic procedures, their results and interpretation in a case with severe lameness in fattening pigs are described. It is shown that selected diagnostic steps lead to identication of various risk factors for disease development in the affected herd. One focus of this case report is the prioritization of diagnostic steps to verify the impact of the different conditions, which nally led to the clinical disorder. Disease is the consequence of previously acting factors, and the involved diagnostic institute is the last stage in the timeline. Some diagnostic ndings might therefore no longer be signicant. -

Download WAO White Book on Allergy
WORLD ALLERGY ORGANIZATION WAWAOO WhiteWhite BookBook onon AllergyAllergy WAO White Book on Allergy World Allergy Organization (WAO) White Book on Allergy Copyright 2011 World Allergy Organization WAO White Book on Allergy Editors Prof. Ruby Pawankar, MD, PhD Prof. Giorgio Walter Canonica, MD WAO President Elect (2010-2011) WAO Past President (2010-2011) Allergy and Rhinology Allergy & Respiratory Diseases Nippon Medical School Department of Internal Medicine 1-1-5 Sendagi, Bunkyo-ku University of Genoa Tokyo 113-8603 Padiglione Maragliano, Largo Rosanna Benzi 10 JAPAN 1-16132 Genoa ITALY Prof. Stephen T. Holgate, BSc, MD, DSc, FMed Sci Prof. Richard F. Lockey, MD Member, WAO Board of Directors (2010-2011) WAO President (2010-2011) Medical Research Council Clinical Professor of Division of Allergy & Immunology Immunopharmacology Joy McCann Culverhouse Chair in Allergy & Immunology Infection, Inflammation and Immunity University of South Florida College of Medicine School of Medicine James Haley Veterans Administration Medical Center (111D) University of Southampton 13000 Bruce B. Downs Boulevard Level F, South Block Tampa, Florida 33612 Southampton General Hospital USA Tremona Road Southampton SO16 6YD United Kingdom Acknowledgement On behalf of the World Allergy Organization (WAO), the editors and authors of the WAO White Book on Allergy express their gratitude to the charity, Asthma, Allergy, Inflammation Research (AAIR) and Asian Allergy Asthma Foundation (AAAF) for their support in the production of this publication. The Editors of the White book extend their gratitude to His Excellency Dr. APJ Abdul Kalam, Former President of India and Madame Ilora Finlay Baronness of the House of Lords for their Forewords to the White Book and to the International Primary Care Respiratory Group (IPCRG) and European Federation of Allergy and Airways Diseases Patients ‘Associations (EFA) for their supporting statements. -

Digital Clubbing
Review Article Digital clubbing Malay Sarkar, D. M. Mahesh1, Irappa Madabhavi2 Department of Pulmonary Medicine, Indira Gandhi Medical College, Shimla, 1Department of Endocrinology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, 2Post Graduate Student (Medicine), Indira Gandhi Medical College, Shimla, India ABSTRACT Digital clubbing is an ancient and important clinical signs in medicine. Although clubbed fingers are mostly asymptomatic, it often predicts the presence of some dreaded underlying diseases. Its exact pathogenesis is not known, but platelet‑derived growth factor and vascular endothelial growth factor are recently incriminated in its causation. The association of digital clubbing with various disease processes and its clinical implications are discussed in this review. KEY WORDS: Cancer, digital clubbing, hypertrophic osteoarthropathy, megakaryocytes, vascular endothelial growth factor Address for correspondence: Dr. Malay Sarkar, Department of Pulmonary Medicine, Indira Gandhi Medical College, Shimla ‑ 171 001, India. E‑mail: [email protected] INTRODUCTION long bones and occasional painful joint enlargement. It was initially known as hypertrophic pulmonary Digital clubbing is characterized by a focal bulbous osteoarthropathy (HPOA) based on the fact that majority enlargement of the terminal segments of the fingers of cases of HOA are due to malignant thoracic tumors. and/or toes due to proliferation of connective tissue The term “pulmonary” was later abandoned as it was between nail matrix and the distal phalanx. It results in realized that the skeletal syndrome may occur in several increase in both anteroposterior and lateral diameter of non‑pulmonary diseases and even may occur without the nails.[1] Clubbed fingers are also known as watch‑glass any underlying illness. -
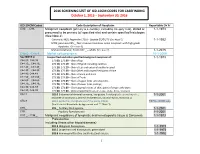
2016 SCREENING LIST of ICD-10CM CODES for CASEFINDING October 1, 2015 – September 30, 2016
2016 SCREENING LIST OF ICD-10CM CODES FOR CASEFINDING October 1, 2015 – September 30, 2016 ICD-10-CM Codes Code Description of Neoplasm Reportable Dx Yr C00._- C96._ Malignant neoplasm (primary & secondary; excluding category C44), stated or 1-1-1973 presumed to be primary (of specified site) and certain specified histologies (See Note 2) Carcinoid, NOS; Appendix C18.0 - Update 01/01/15 (See Note 5) 1-1-1992 MCN; pancreas C25._; Non-invasive mucinous cystic neoplasm with high grade dysplasia. (See note 6) Mature teratoma; Testis C62._ – adults (See note 7) 1-1-2015 C4a.0_-C4a.9_ Merkel cell carcinoma 10-1-2009 See NOTE 4 Unspecified and other specified malignant neoplasm of : 1-1-1973 C44.00.-C44.09 173.00, 173.09 – Skin of Lip C44.10_, C44.19_ 173.10, 173.19 – Skin of Eyelid including canthus C44.20_, C44.29_ 173. 20, 173.29 – Skin of Ear and external auditory canal C44.30_, C44.39_ 173.30, 173.39 – Skin Other and unspecified parts of face C44.40, C44.49 173. 40, 173.49 – Skin of Scalp and neck C44.50_, C44.59_ 173.50, 173.59 – Skin of Trunk C44.60_, C44.69_ 173. 60, 173.69 – Skin of Upper limb and shoulder, C44.70_, C44.79_ 173.70, 173.79 – Skin of Lower limb and hip; C44.80, C44.89 173.80, 173.89 – Overlapping lesions of skin, point of origin unknown; C44.90, C44.99 173.90, 173.99 - Sites unspecified (excludes Labia, Vulva, Penis, Scrotum) C54.1 182.0 Endometrial stromal sarcoma, low grade; Endolymphatic stromal myosis ; 1-1-2001 Endometrial stromatosis, Stromal endometriosis, Stromal myosis, NOS (C54.1) C56.9 183.0 Borderline malignancies -

Percutaneous Conchotome Muscle Biopsy. a Useful Diagnostic and Assessment Tool CHRISTINA DORPH, INGER NENNESMO, and INGRID E
Percutaneous Conchotome Muscle Biopsy. A Useful Diagnostic and Assessment Tool CHRISTINA DORPH, INGER NENNESMO, and INGRID E. LUNDBERG ABSTRACT. Objective. To evaluate the diagnostic yield, performance simplicity, and safety of the percutaneous conchotome muscle biopsy technique for clinical and research purposes in an outpatient rheuma- tology clinic. Methods. Biopsies taken by rheumatologists in an outpatient clinic during 1996 and 1997 were eval- uated for histopathological and clinical diagnoses. Results. A total of 149 biopsies were performed on 122 patients. Physicians learned the method easily. Samples were of adequate size and quality to allow for diagnostics. In total 106 biopsies were taken due to different diagnostic suspicions: 24 polymyositis (PM) or dermatomyositis (DM); 43 PM, DM, or vasculitis in addition to another rheumatic condition; 19 systemic vasculitis; and 20 myalgias. Criteria for definite or probable PM/DM were fulfilled in 21 patients, 18 with positive biopsies. Thirteen patients received vasculitis as clinical diagnosis, 3 with positive biopsies. No patient with myalgia had a biopsy with inflammatory changes. Fifteen of 43 rebiopsies performed to assess disease activity had signs of active inflammation. In 48% there were changes in immuno- suppressive therapy after biopsy results. Four complications occurred; one was a serious subfascial hematoma. Conclusion. The percutaneous conchotome muscle biopsy technique gives a good size sample that allows for diagnostic evaluation and has a high yield in patients with myositis. It is a simple proce- dure, easy to learn and to perform, with a low complication rate and minimum discomfort for the patient. The method can preferably be used as a diagnostic tool and to perform repeated biopsies to assess the effect of a given therapy for both clinical and research purposes. -

Frequency and Criticality of Diagnoses in Family Medicine Practices: from the National Ambulatory Medical Care Survey (NAMCS)
J Am Board Fam Med: first published as 10.3122/jabfm.2018.01.170209 on 12 January 2018. Downloaded from ORIGINAL RESEARCH Frequency and Criticality of Diagnoses in Family Medicine Practices: From the National Ambulatory Medical Care Survey (NAMCS) Michael R. Peabody, PhD, Thomas R. O’Neill, PhD, Keith L. Stelter, MD, MMM, and James C. Puffer, MD Background: Family medicine is a specialty of breadth, providing comprehensive health care for the individual and the family that integrates the broad scope of clinical, social, and behavioral sciences. As such, the scope of practice (SOP) for family medicine is extensive; however, over time many family phy- sicians narrow their SOP. We sought to provide a nationally representative description of the most com- mon and the most critical diagnoses that family physicians see in their practice. Methods: Data were extracted from the 2012 National Ambulatory Medical Care Survey (NAMCS) to select all ICD-9 codes reported by family physicians. A panel of family physicians then reviewed 1893 ICD-9 codes to place each code into an American Board of Family Medicine Family Medicine Certifica- tion Examination test plan specifications (TPS) category and provide a rating for an Index of Harm (IoH). Results: An analysis of all 1893 ICD-9 codes seen by family physicians in the 2012 NAMCS found that 198 ICD-9 codes could not be assigned a TPS category, leaving 1695 ICD-9 codes in the dataset. Top 10 lists of ICD-9 codes by TPS category were created for both frequency and IoH. Conclusions: This study provides a nationally representative description of the most common diag- copyright. -

Urticaria from Wikipedia, the Free Encyclopedia Jump To: Navigation, Search "Hives" Redirects Here
Urticaria From Wikipedia, the free encyclopedia Jump to: navigation, search "Hives" redirects here. For other uses, see Hive. Urticaria Classification and external resourcesICD-10L50.ICD- 9708DiseasesDB13606MedlinePlus000845eMedicineemerg/628 MeSHD014581Urtic aria (or hives) is a skin condition, commonly caused by an allergic reaction, that is characterized by raised red skin wheals (welts). It is also known as nettle rash or uredo. Wheals from urticaria can appear anywhere on the body, including the face, lips, tongue, throat, and ears. The wheals may vary in size from about 5 mm (0.2 inches) in diameter to the size of a dinner plate; they typically itch severely, sting, or burn, and often have a pale border. Urticaria is generally caused by direct contact with an allergenic substance, or an immune response to food or some other allergen, but can also appear for other reasons, notably emotional stress. The rash can be triggered by quite innocent events, such as mere rubbing or exposure to cold. Contents [hide] * 1 Pathophysiology * 2 Differential diagnosis * 3 Types * 4 Related conditions * 5 Treatment and management o 5.1 Histamine antagonists o 5.2 Other o 5.3 Dietary * 6 See also * 7 References * 8 External links [edit] Pathophysiology Allergic urticaria on the shin induced by an antibiotic The skin lesions of urticarial disease are caused by an inflammatory reaction in the skin, causing leakage of capillaries in the dermis, and resulting in an edema which persists until the interstitial fluid is absorbed into the surrounding cells. Urticarial disease is thought to be caused by the release of histamine and other mediators of inflammation (cytokines) from cells in the skin. -

Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence
3 Scientific and Medical Aspects of Apheresis: Issues and Evidence 3 ● Scientific and Medical Aspects of Apheresis: Issues and Evidence Various types of apheresis procedures have paucity of high-quality research, conclusions been performed on a clinical basis for many years, about the safety, efficacy, and effectiveness of but the number of patients and types of diseases apheresis are necessarily limited, although some treated have risen significantly in the last 5 years. tentative conclusions and directions for treatment This increase is partially due to increased under- can be discerned. standing of the disease and partially due to engi- The present chapter analyzes the methodolog- neering advances in equipment technologies. By ical problems in conducting apheresis research and almost any standard, treatment by apheresis is still examines available evidence of the safety, ef- in relatively early stages of development—there ficacy, and effectiveness of apheresis. Following are no ideal protocols based on a thorough un- a discussion of methodological issues, several derstanding of reasons for its efficacy. Never- major reviews of apheresis research will be sum- theless, there is an increasing flow of clinical data, marized and evaluated. This chapter will further sometimes describing dramatic patient improve- include the findings of a primary literature review ment, supporting the view that apheresis is a and assessment of apheresis in the treatment of rapidly emerging technology with significant three diseases—namely, hemolytic uremic syn- promise (117). Such evidence of treatment effec- drome, acquired Factor-VIII inhibitor, and Guil- tiveness’ is even today, however, often based on lain-Barré syndrome— where preliminary reports unsystematically collected data. -

Are Serum Aluminum Levels a Risk Factor in the Appearance of Spontaneous Pneumothorax?
Turk J Med Sci 2010; 40 (3): 459-463 Original Article © TÜBİTAK E-mail: [email protected] doi:10.3906/sag-0901-11 Are serum aluminum levels a risk factor in the appearance of spontaneous pneumothorax? Serdar HAN1, Rasih YAZKAN2, Bülent KOÇER3,*, Gültekin GÜLBAHAR3, Serdal Kenan KÖSE4, Koray DURAL3, Ünal SAKINCI3 Aim: To investigate the relationship between aluminum and spontaneous pneumothorax (SP) development. Materials and methods: A patient group and a control group were formed with 100 individuals in each. The serum aluminum levels of the groups were determined and statistically compared. Results: The mean serum aluminum levels were 5.6 ± 2.4 μg/L (1.6-11.9) and 23.2 ± 15.4 μg/L (2-81) in the control and SP groups, respectively (P < 0.001). The specificity and sensitivity of the measurement of aluminum level were 74.4% and 86.4% in the SP group. The risk of SP development was found to be 18 times higher in individuals with high serum levels of aluminum compared to that in individuals with low serum levels of aluminum. Conclusion: A high level of aluminum is a risk factor for the development of SP. Key words: Aluminum, pneumothorax, public health Spontan pnömotoraks gelişiminde serum aluminyum seviyeleri bir risk faktörü müdür? Amaç: Bu çalışmada spontan pnömotoraks (SP) gelişimi ile serum aluminyum düzeyleri arasındaki ilişkinin analiz edilmesi amaçlandı. Yöntem ve gereç: Yüz SP hastasından oluşan hasta grubunun yanı sıra 100 kişiden oluşan sağlıklı kontrol grubu çalışmaya dahil edildi. Gruplar serum aluminyum düzeyleri açısından istatistiksel olarak kıyaslandı. Bulgular: Ortalama serum aluminyum düzeyleri SP ve kontrol grupları için sırasıyla 5,6 ± 2,4 μg/L (1,6-11,9) ve 23,2 ± 15,4 μg/L (2-81) bulundu (P < 0,001). -

Code Description
Code Description 0061 Chronic intestinal amebiasis without mention of abscess 0062 Amebic nondysenteric colitis 0063 Amebic liver abscess 0064 Amebic lung abscess 00642 West Nile fever with other neurologic manifestation 00649 West Nile fever with other complications 0065 Amebic brain abscess 0066 Amebic skin ulceration 0068 Amebic infection of other sites 0069 Amebiasis, unspecified 0070 Other protozoal intestinal diseases, balantidiasis (Infection by Balantidium coli) 0071 Other protozoal intestinal diseases, giardiasis 0072 Other protozoal intestinal diseases, coccidiosis 0073 Other protozoal intestinal diseases, trichomoniasis 0074 Other protozoal intestinal diseases, cryptosporidiosis 0075 Other protozoal intestional disease cyclosporiasis 0078 Other specified protozoal intestinal diseases 0079 Unspecified protozoal intestinal disease 01000 Primary tuberculous infection, unspecified 01001 Primary tuberculous infection bacteriological or histological examination not done 01002 Primary tuberculous infection, bacteriological or histological examination results unknown 01003 Primary tuberculous infection, tubercle bacilli found by microscopy 01004 Primary tuberculous infection, tubercle bacilli found by bacterial culture 01005 Primary tuberculous infection, tubercle bacilli confirmed histolgically 01006 Primary tuberculous infection, tubercle bacilli found by other methods 01010 Tuberculous pleurisy in primary progressive tuberculosis unspecified 01011 Tuberculous pleurisy bacteriological or histological examination not done 01012 Tuberculous