Chapter 6 Neuroprotection As a Treatment for Nerve Agent Survivors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Endobj 21 0 Obj <>/Filter/Flatedecode/ID[]/Index[16 7]](https://docslib.b-cdn.net/cover/9015/endobj-21-0-obj-filter-flatedecode-id-index-16-7-69015.webp)
Endobj 21 0 Obj <>/Filter/Flatedecode/ID[]/Index[16 7]
%PDF-1.4 %âãÏÓ 16 0 obj <> endobj 21 0 obj <>/Filter/FlateDecode/ID[]/Index[16 7]/Info 15 0 R/Length 36/Prev 1529327/Root 17 0 R/Size 23/Type/XRef/W[1 2 0]>>stream hÞbbd`b`r`b`cb`>stream hÞb```f``âc```‘¨`b@ ›…£éœÌ®5zà $À Å 9 Â Ü Ì‚`.ƒlÕ ÍÄ÷ ,"† endstream endobj 17 0 obj < > endobj 18 0 obj < >>>/Rotate 0/Type/Page>> endobj 19 0 obj <>stream H‰*ä234Ò300P AsK;9—KßËÓ0QÁ%Ÿ+ À H endstream endobj 20 0 obj <>stream ÿØÿà JFIF È È ÿþ Business Office Q76ÿÛ C $.' ",#(7),01444'9=82 À@ú– ~5â¾Óµï‰V%Õ ¢¾bø‡ã?xKÄ_Ùñj:eŵÄms{24.@C†ÁÇ=ý+¼ø[©ø¯Äš$ö©`±]G †Ö;6R¤6ÕvmÜò§ØõôsØh¯– •êž ¿ñ^»áØuBïKI/ao Z>"ç†cæ|Û‡8ã¿jzògˆþ+øÓ@ÖõM"{- å°+—Xåë.å#çãå#ŽÕêi?Ål’æðƒ»¨qûHÊ‘‘ϯ·Oz ö +Ç>xÇÄ>!ÕuÍ+Äz]¶Ÿw¦y@Çs—Üy%ˆ# G-7âÄ;ZÓ|1 Yï_°&b"…OBøç=ñè3ée¢¼CRÔ¾&øvÖãT»³Ðµ»X†ù-,|ØfUï³ çŽÇ'Ž3W-|}zÿ ÛÆ’Ù[›¡È-ÑÎÎ%(y= 'ß=(Øè¯ “Åß`ðôÚÝÏ„´ûh¡·7פJ.âJcƒŒü¤‚:ž+šðïÅÏxŠþ?Mð½¬×2De ÞìF2yâ€>š¢¼'Dñ÷Šçñm—†õ¿ G¥És ²¬†äJ¬ e㨠ã$dqYÞ$ø¥¯x_UþËÕü5l&h„ÑIoz]$L‘JÔt#4ô=àº7|q¬é°ê–>Žk)”¼nº¤`°=½+sÁ?/ øRÞI"›ÄºLrFþ[£^F ·Lc=³Ï§9èk¯R òï@EPEPEPEPETº½µ³]×W0À¾²È~µ–«§_ŒÙ_ÚÜŒ•ýÌÊüœp}(JŠ¨·¶¬$+s ¹ŽB$#ÿ túGñsé Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( Š( çŠ9âxe@ñÈ¥]OBWç¼2Kðãâ@ÌB(¬oXÚyläóŽçc{ãÒ¿C+äoÚKI÷ºv¸‘'…¬å9Ç –_ǹö Kø¼÷$¶²ðfñ5Î-ܼÊ$1 ë’äç½|ýð_þÈñݧÚTEöøÛO™U—pÛ‘žà~ ¯qø §_Ë£jÓ šÑ¼Ï|EÕuR]´ý¦Û÷~ÐØy˜¹bžÄc-Mñ´ð÷Yʆâƒÿ ]’´þxrO xVÎÎá¦kÙ³svf}Íç>dþúu=k7ãgü“ícþØÿ èä gÍ¿ üa£ø3YÕoµ‰fQ-š¬1Åv•ƒg°?\z÷ÿ ƒZ™ñW†5;ûÍÒ¥ö¥rÍœ…FƯ@§åßbŽãÄ:äSD²Fl£R®¡•cAîü4 ¦¿=|[á]KÀ¾3ÒìÅóÊ%Ó0p~Àÿ úz'Â?hžÑ-nuÍ6ˆ¡"H¤»]öê -

Tinnitus Hopes Put to Sleep by Latest Auris Failure
March 14, 2018 Tinnitus hopes put to sleep by latest Auris failure Madeleine Armstrong Ketamine is best known as a horse tranquiliser or a recreational drug, but it has also been proposed as a treatment for various disorders from depression to Alzheimer’s. Hopes of developing the drug in tinnitus have been dashed by the failure of Auris’s Keyzilen in a second phase III trial. As well as leaving Auris’s future looking bleak – Keyzilen is the second of its phase III candidates to flunk in four months – the setback could also be bad news for the sparse tinnitus pipeline. According to EvaluatePharma there is only one other candidate in active clinical development, Otonomy’s OTO-313, and this uses the same mechanism of action as Keyzilen (see table below). Tinnitus pipeline Generic Project Company Pharma class Trial(s) Notes name Phase III Auris Esketamine TACTT2 Keyzilen NMDA antagonist Failed Aug 2016 Medical hydrochloride (NCT01803646) TACTT3 Failed Mar 2018 (NCT02040194) Phase I OTO- Phase I/II trial to OTO-311 abandoned in Otonomy NMDA antagonist Gacyclidine 313 start H1 2019 favour of this formulation Preclinical Auris AM-102 Undisclosed - - Medical KCNQ2 Knopp Kv7 potassium - - Program Biosciences channel modulator Source: EvaluatePharma. Both projects are psychoactive drugs targeting the NMDA receptor. Tinnitus is commonly caused by loud noise and resulting damage to the sensory hair cells in the cochlea. Initial trauma to the inner ear has been shown to trigger excess production of glutamate, which leads to the hyperactivation of NMDA receptors and, in turn, cell death. Blocking the NMDA receptor could therefore have a protective effect – but it is unclear how this mechanism would work once the damage to hair cells had been done. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Salicylate Induces Tinnitus Through Activation of Cochlear NMDA Receptors
3944 • The Journal of Neuroscience, May 1, 2003 • 23(9):3944–3952 Salicylate Induces Tinnitus through Activation of Cochlear NMDA Receptors Matthieu J. Guitton,1 Jean Caston,2 Je´roˆme Ruel,1 Randolph M. Johnson,3 Re´my Pujol,1 and Jean-Luc Puel1 1Institut National de la Sante´ et de la Recherche Me´dicale UR-254, Laboratoire de Neurobiologie de l’Audition–Plasticite´ Synaptique, Faculte´deMe´decine, Universite´ de Montpellier 1, 34090 Montpellier, France, 2 Unite´ Propre de Recherche et de l’Enseignement Supe´rieur 1780, Laboratoire de Neurobiologie de l’Apprentissage, Universite´ de Rouen, 76821 Mont-Saint-Aignan, France, and 3DURECT Corporation, Cupertino, California 95014 Salicylate, the active component of aspirin, is known to induce tinnitus. However, the site and the mechanism of generation of tinnitus induced by salicylate remains unclear. Here, we developed a behavioral procedure to measure tinnitus in rats. The behavioral model was based on an active avoidance paradigm in which rats had to display a motor task (i.e., to jump on a climbing pole when hearing a sound). Giving salicylate led to a decrease in the percentage of correct responses (score) and a drastic increase in the number of false positive responses (i.e., animals execute the motor task during a silent period). Presentation of the sound at a constant perceptive level prevents decrease of the score, leading to the proposal that score is related to hearing performance. In contrast, the increase of false positive responses remained unchanged. In fact, animals behaved as if they hear a sound, indicating that they are experiencing tinnitus. -

Customs Tariff - Schedule
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2020 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT, CEUT, UAT, CPTPT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

Nerve Agent - Lntellipedia Page 1 Of9 Doc ID : 6637155 (U) Nerve Agent
This document is made available through the declassification efforts and research of John Greenewald, Jr., creator of: The Black Vault The Black Vault is the largest online Freedom of Information Act (FOIA) document clearinghouse in the world. The research efforts here are responsible for the declassification of MILLIONS of pages released by the U.S. Government & Military. Discover the Truth at: http://www.theblackvault.com Nerve Agent - lntellipedia Page 1 of9 Doc ID : 6637155 (U) Nerve Agent UNCLASSIFIED From lntellipedia Nerve Agents (also known as nerve gases, though these chemicals are liquid at room temperature) are a class of phosphorus-containing organic chemicals (organophosphates) that disrupt the mechanism by which nerves transfer messages to organs. The disruption is caused by blocking acetylcholinesterase, an enzyme that normally relaxes the activity of acetylcholine, a neurotransmitter. ...--------- --- -·---- - --- -·-- --- --- Contents • 1 Overview • 2 Biological Effects • 2.1 Mechanism of Action • 2.2 Antidotes • 3 Classes • 3.1 G-Series • 3.2 V-Series • 3.3 Novichok Agents • 3.4 Insecticides • 4 History • 4.1 The Discovery ofNerve Agents • 4.2 The Nazi Mass Production ofTabun • 4.3 Nerve Agents in Nazi Germany • 4.4 The Secret Gets Out • 4.5 Since World War II • 4.6 Ocean Disposal of Chemical Weapons • 5 Popular Culture • 6 References and External Links --------------- ----·-- - Overview As chemical weapons, they are classified as weapons of mass destruction by the United Nations according to UN Resolution 687, and their production and stockpiling was outlawed by the Chemical Weapons Convention of 1993; the Chemical Weapons Convention officially took effect on April 291997. Poisoning by a nerve agent leads to contraction of pupils, profuse salivation, convulsions, involuntary urination and defecation, and eventual death by asphyxiation as control is lost over respiratory muscles. -
Warning: the Following Lecture Contains Graphic Images
What the новичок (Novichok)? Why Chemical Warfare Agents Are More Relevant Than Ever Matt Sztajnkrycer, MD PHD Professor of Emergency Medicine, Mayo Clinic Medical Toxicologist, Minnesota Poison Control System Medical Director, RFD Chemical Assessment Team @NoobieMatt #ITLS2018 Disclosures In accordance with the Accreditation Council for Continuing Medical Education (ACCME) Standards, the American Nurses Credentialing Center’s Commission (ANCC) and the Commission on Accreditation for Pre-Hospital Continuing Education (CAPCE), states presenters must disclose the existence of significant financial interests in or relationships with manufacturers or commercial products that may have a direct interest in the subject matter of the presentation, and relationships with the commercial supporter of this CME activity. The presenter does not consider that it will influence their presentation. Dr. Sztajnkrycer does not have a significant financial relationship to report. Dr. Sztajnkrycer is on the Editorial Board of International Trauma Life Support. Specific CW Agents Classes of Chemical Agents: The Big 5 The “A” List Pulmonary Agents Phosgene Oxime, Chlorine Vesicants Mustard, Phosgene Blood Agents CN Nerve Agents G, V, Novel, T Incapacitating Agents Thinking Outside the Box - An Abbreviated List Ammonia Fluorine Chlorine Acrylonitrile Hydrogen Sulfide Phosphine Methyl Isocyanate Dibotane Hydrogen Selenide Allyl Alcohol Sulfur Dioxide TDI Acrolein Nitric Acid Arsine Hydrazine Compound 1080/1081 Nitrogen Dioxide Tetramine (TETS) Ethylene Oxide Chlorine Leaks Phosphine Chlorine Common Toxic Industrial Chemical (“TIC”). Why use it in war/terror? Chlorine Density of 3.21 g/L. Heavier than air (1.28 g/L) sinks. Concentrates in low-lying areas. Like basements and underground bunkers. Reacts with water: Hypochlorous acid (HClO) Hydrochloric acid (HCl). -
CAS Number Index
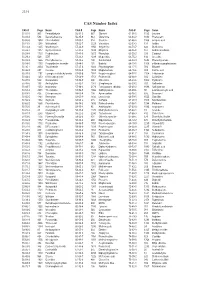
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Chemical Weapon
Awareness incapacitates, though they operate more through excited state (e.g., muscle contraction). The eventual interactions outside the central nervous system. exhaustion of muscles leads to respiratory failure and death. Chemical Weapon A separate class of nerve agents is related to Tetrodotoxin, frequently abbreviated as TTX, which is a potent 3- Lethal agents neurotoxin with unknown antidote. Tetrodotoxin blocks action potentials in nerves by binding to the voltage-gated, minutes after removal. Casualty effects are not anticipated These substances are for producing chemical casualties fast sodium channels in nerve cell membranes, essentially to exceed 24-hours nor require medical attention. They without regard to long-term consequences or loss of life. preventing any affected nerve cells from firing by blocking include: They cause injuries that require medical treatment. the channels used in the process. a- Tear agents: These sensory irritants produce immediate pain to the a- Blister agents: a- G series: these are low volatility nerve agents that are eyes and irritate mucous membranes (also known as A blister agent is a chemical compound that irritates and typically used from a non-persistent to semi-persistent lachrymatory agent or lachrymator). causes injury to the skin. These substances also attack effect. Dr. Alice Gerges Geagea the eyes, or any other tissue they contact. • Tabun (GA) Director of Health Education b- Vomiting agents: • Vesicants: the vesicants are substances that produce • Sarin (GB) Lebanese Health Society These sensory irritants are also termed sternators or large fluid-filled blisters on the skin: • Soman (GD) nose irritants. They irritate the mucous membranes to • Nitrogen mustards • Cyclosarin (GF) produce congestion, coughing, sneezing and eventually • Sulfur mustards A Chemical Weapon Agent (CWA) is a device that nausea. -

Medical Aspects of Chemical Warfare
Medical Diagnostics Chapter 22 MEDICAL DIAGNOSTICS † ‡ § BENEDICT R. CAPACIO, PHD*; J. RICHARD SMITH ; RICHARD K. GORDON, PHD ; JULIAN R. HAIGH, PHD ; JOHN ¥ ¶ R. BARR, PHD ; AND GENNADY E. PLATOFF JR, PHD INTRODUCTION NERVE AGENTS SULFUR MUSTARD LEWISITE CYANIDE PHOSGENE 3-QUINUCLIDINYL BENZILATE SAMPLE CONSIDERATIONS Summary * Chief, Medical Diagnostic and Chemical Branch, Analytical Toxicology Division, US Army Medical Research Institute of Chemical Defense, 3100 Rickets Point Road, Aberdeen Proving Ground, Maryland 21010-5400 † Chemist, Medical Diagnostic and Chemical Branch, Analytical Toxicology Division, US Army Medical Research Institute of Chemical Defense, 3100 Rickets Point Road, Aberdeen Proving Ground, Maryland 21010-5400 ‡ Chief, Department of Biochemical Pharmacology, Biochemistry Division, Walter Reed Army Institute of Research, 503 Robert Grant Road, Silver Spring, Maryland 20910-7500 § Research Scientist, Department of Biochemical Pharmacology, Biochemistry Division, Walter Reed Army Institute of Research, 503 Robert Grant Road, Silver Spring, Maryland 20910-7500 ¥ Lead Research Chemist, Centers for Disease Control and Prevention, 4770 Buford Highway, Mailstop F47, Atlanta, Georgia 30341 ¶ Colonel, US Army (Retired); Scientific Advisor, Office of Biodefense Research, National Institute of Allergies and Infectious Disease, National Institutes of Health, 6610 Rockledge Drive, Room 4069, Bethesda, Maryland 20892-6612 691 Medical Aspects of Chemical Warfare INTRODUCTION In the past, issues associated with chemical war- an -

744 Hydrolysis of Chiral Organophosphorus Compounds By
[Frontiers in Bioscience, Landmark, 26, 744-770, Jan 1, 2021] Hydrolysis of chiral organophosphorus compounds by phosphotriesterases and mammalian paraoxonase-1 Antonio Monroy-Noyola1, Damianys Almenares-Lopez2, Eugenio Vilanova Gisbert3 1Laboratorio de Neuroproteccion, Facultad de Farmacia, Universidad Autonoma del Estado de Morelos, Morelos, Mexico, 2Division de Ciencias Basicas e Ingenierias, Universidad Popular de la Chontalpa, H. Cardenas, Tabasco, Mexico, 3Instituto de Bioingenieria, Universidad Miguel Hernandez, Elche, Alicante, Spain TABLE OF CONTENTS 1. Abstract 2. Introduction 2.1. Organophosphorus compounds (OPs) and their toxicity 2.2. Metabolism and treatment of OP intoxication 2.3. Chiral OPs 3. Stereoselective hydrolysis 3.1. Stereoselective hydrolysis determines the toxicity of chiral compounds 3.2. Hydrolysis of nerve agents by PTEs 3.2.1. Hydrolysis of V-type agents 3.3. PON1, a protein restricted in its ability to hydrolyze chiral OPs 3.4. Toxicity and stereoselective hydrolysis of OPs in animal tissues 3.4.1. The calcium-dependent stereoselective activity of OPs associated with PON1 3.4.2. Stereoselective hydrolysis commercial OPs pesticides by alloforms of PON1 Q192R 3.4.3. PON1, an enzyme that stereoselectively hydrolyzes OP nerve agents 3.4.4. PON1 recombinants and stereoselective hydrolysis of OP nerve agents 3.5. The activity of PTEs in birds 4. Conclusions 5. Acknowledgments 6. References 1. ABSTRACT Some organophosphorus compounds interaction of the racemic OPs with these B- (OPs), which are used in the manufacturing of esterases (AChE and NTE) and such interactions insecticides and nerve agents, are racemic mixtures have been studied in vivo, ex vivo and in vitro, using with at least one chiral center with a phosphorus stereoselective hydrolysis by A-esterases or atom. -

Enzymatic Degradation of Organophosphorus Pesticides and Nerve Agents by EC: 3.1.8.2
catalysts Review Enzymatic Degradation of Organophosphorus Pesticides and Nerve Agents by EC: 3.1.8.2 Marek Matula 1, Tomas Kucera 1 , Ondrej Soukup 1,2 and Jaroslav Pejchal 1,* 1 Department of Toxicology and Military Pharmacy, Faculty of Military Health Sciences, University of Defence, Trebesska 1575, 500 01 Hradec Kralove, Czech Republic; [email protected] (M.M.); [email protected] (T.K.); [email protected] (O.S.) 2 Biomedical Research Center, University Hospital Hradec Kralove, Sokolovska 581, 500 05 Hradec Kralove, Czech Republic * Correspondence: [email protected] Received: 26 October 2020; Accepted: 20 November 2020; Published: 24 November 2020 Abstract: The organophosphorus substances, including pesticides and nerve agents (NAs), represent highly toxic compounds. Standard decontamination procedures place a heavy burden on the environment. Given their continued utilization or existence, considerable efforts are being made to develop environmentally friendly methods of decontamination and medical countermeasures against their intoxication. Enzymes can offer both environmental and medical applications. One of the most promising enzymes cleaving organophosphorus compounds is the enzyme with enzyme commission number (EC): 3.1.8.2, called diisopropyl fluorophosphatase (DFPase) or organophosphorus acid anhydrolase from Loligo Vulgaris or Alteromonas sp. JD6.5, respectively. Structure, mechanisms of action and substrate profiles are described for both enzymes. Wild-type (WT) enzymes have a catalytic activity against organophosphorus compounds, including G-type nerve agents. Their stereochemical preference aims their activity towards less toxic enantiomers of the chiral phosphorus center found in most chemical warfare agents. Site-direct mutagenesis has systematically improved the active site of the enzyme. These efforts have resulted in the improvement of catalytic activity and have led to the identification of variants that are more effective at detoxifying both G-type and V-type nerve agents.