Transmission of SARS-Cov-2 Lineage B.1.1.7 in England: Insights from Linking Epidemiological and Genetic Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Research Framework Revised.Vp
Frontispiece: the Norfolk Rapid Coastal Zone Assessment Survey team recording timbers and ballast from the wreck of The Sheraton on Hunstanton beach, with Hunstanton cliffs and lighthouse in the background. Photo: David Robertson, copyright NAU Archaeology Research and Archaeology Revisited: a revised framework for the East of England edited by Maria Medlycott East Anglian Archaeology Occasional Paper No.24, 2011 ALGAO East of England EAST ANGLIAN ARCHAEOLOGY OCCASIONAL PAPER NO.24 Published by Association of Local Government Archaeological Officers East of England http://www.algao.org.uk/cttees/Regions Editor: David Gurney EAA Managing Editor: Jenny Glazebrook Editorial Board: Brian Ayers, Director, The Butrint Foundation Owen Bedwin, Head of Historic Environment, Essex County Council Stewart Bryant, Head of Historic Environment, Hertfordshire County Council Will Fletcher, English Heritage Kasia Gdaniec, Historic Environment, Cambridgeshire County Council David Gurney, Historic Environment Manager, Norfolk County Council Debbie Priddy, English Heritage Adrian Tindall, Archaeological Consultant Keith Wade, Archaeological Service Manager, Suffolk County Council Set in Times Roman by Jenny Glazebrook using Corel Ventura™ Printed by Henry Ling Limited, The Dorset Press © ALGAO East of England ISBN 978 0 9510695 6 1 This Research Framework was published with the aid of funding from English Heritage East Anglian Archaeology was established in 1975 by the Scole Committee for Archaeology in East Anglia. The scope of the series expanded to include all six eastern counties and responsi- bility for publication passed in 2002 to the Association of Local Government Archaeological Officers, East of England (ALGAO East). Cover illustration: The excavation of prehistoric burial monuments at Hanson’s Needingworth Quarry at Over, Cambridgeshire, by Cambridge Archaeological Unit in 2008. -
Postgraduate Research Symposium Programme 23 June 2021
[Type here] School of Biomedical Engineering & Imaging Sciences Postgraduate Research Symposium Programme 23 June 2021 Organising Committe Agenda MS Teams Live Event 1 You can join Live Event 1 here. Time Speaker Title Professor Sebastien Ourselin Introduction Head of the School of Biomedical Engineering & Imaging Sciences, King's and College London Welcome 13:00 – 13:05 – 13:05 13:00 Dr Samantha Terry Senior Lecturer in Radiobiology, School of Biomedical Engineering & Imaging Sciences, King's College London Ines Costa PhD student, School of Biomedical Engineering & Imaging Sciences, King's Public Engagement College London 13:05 – 13:15 – 13:15 13:05 Aishwarya Mishra PhD student, Centre for Doctoral Training (CDT) in Smart Medical Imaging, King's College London and Imperial College London Dr Valentina Vitiello Professional Services Deputy Representative for the School DDI Committee; Diversity and Bullying Specialist Technical Operations Manager, School of Biomedical Engineering & Imaging Sciences, King's College London 13:15 – 13:25 13:25 – 13:15 Dr Stamatia Giannarou Royal Society University Research Fellow and Lecturer in Surgical Cancer Keynote Speaker Technology and Imaging at the Hamlyn Centre for Robotic Surgery, Department of Surgery and Cancer, Imperial College London Cognitive Vision in Robotic Surgery 13:25 – 14:05 – 14:05 13:25 Please refer to page 7 for further details. Student Please refer to page 4 for details. Three-Minute Thesis Presentations 14:05 – 14:35 – 14:35 14:05 Student Please refer to pages 5-6 for details. 1-Minute Poster Pitches 14:35 – 15:00 15:00 – 14:35 1 Poster Sessions The poster sessions will be taking place in two streams on the Wonder.me platform. -

Understanding Cambridge University and Its Grading Scheme
Understanding Cambridge University and its Grading Scheme Samantha Farrell-Schmitt earned her undergraduate degree in 1996 from University of Cambridge in the United Kingdom (UK). For the purposes of placing this in the context of an American review, we wish to emphasize the reputation of her university and explain the grading system used in the UK and how it roughly translates to US scores. The University of Cambridge (www.cam.ac.uk) is one of the preeminent universities in the world, founded over 800 years ago, and containing 31 constituent colleges and more than 100 academic departments. It has produced 91 Nobel Laureates, more than any other university in the world. The University of Cambridge is ranked by US News and World Report as the 6th best university in the world, ranked alongside Harvard, MIT, UC Berkeley, Stanford, and the University of Oxford (see http://www.usnews.com/education/best-global- universities/rankings). Times Higher Education ranks the university as 5th in the world, the Center for World University Rankings places it as 4th, ahead of both Princeton and Yale. Amongst the 31 colleges of the university is Homerton College, where Samantha studied. Homerton is generally regarded as the leading center for the study of Primary and Secondary Education in the UK. As a UK university, Cambridge follows a grading system different to most US colleges and universities. Thus, the scores and percentages shown on Samantha’s university transcript must be read with an understanding of this distinction. Samantha’s degree shows that she has graduated with honors (honours, to use the British spelling). -
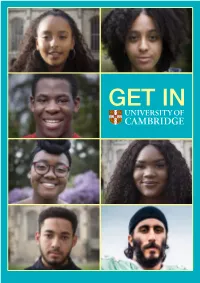
Get in They Did It
GET IN THEY DID IT WHAT’S STOPPING YOU? When you think of a Cambridge University student, who do you picture? A Black woman from a north London council estate with 41k followers on YouTube? A headscarfed Muslim student from a state school GET PAID TO STUDY in Bradford? An American Football-playing Sikh Last year, grime artist Stormzy announced The engineer? Perhaps not, but Stormzy Scholarship, a brand new studentship all of them recently made the scheme for University of Cambridge students decision to apply to study which will see four British black students provided AFRICAN CARIBBEAN SOCIETY (ACS) here, and all of them were with financial support during their degree courses. successful. The Stormzy Scholarship covers the full cost of four tuition fees and provides a maintenance grant A record 23.5% of this year’s for up to four years of any undergraduate course. new undergraduates are from The first two students started their courses last BME backgrounds - and a October, and two further students will be selected great deal of work is under for 2019 entry. way at the University to attract more. Stormzy says: “I hope this scholarship serves as a small reminder that if young black students wish to But we know - from research study at one of the best universities in the world, - that there is still a perception then the opportunity is yours for the taking – and among BME students that if funding is one of the barriers, then we can work Cambridge is ‘not for them’. towards breaking that barrier down.” So our message to any Year Separately, The Cambridge Bursary - up to £3,500 12 or 13 pupil who thinks they per year - is available to students from households might not ‘fit in’ is quite simple with an income below £42,620 on a scale linked to their household income. -

Commentary Disease Transmission Dynamics and the Evolution
Proc. Natl. Acad. Sci. USA Vol. 96, pp. 800–801, February 1999 Commentary Disease transmission dynamics and the evolution of antibiotic resistance in hospitals and communal settings Simon A. Levin*† and Viggo Andreasen‡ *Department of Ecology and Evolutionary Biology, Eno Hall, Princeton University, Princeton NJ 08544; and ‡Department of Mathematics, Roskilde University, DK-4000 Roskilde, Denmark Despite the tremendous benefits of antibiotics for dealing with sally, exercising little influence on their host under normal a wide range of pathogens, there is by now little doubt that conditions. Antibiotics are typically introduced to treat the their indiscriminate use has led to the emergence of novel true pathogens, and for them the problem of resistance resistant strains and a frightening new set of threats to public introduces questions concerning the length and intensity of health. Hospitals and other community settings provide an treatment, multidrug strategies, and patient compliance. (See, especially fertile ground for the spread of those types; in for example, refs. 2–4). Commensals provide a different sort particular, the recent emergence and proliferation of bacteria of problem, however. Under normal conditions, they live in resistant to both methicillin and vancomycin has engendered such places as the skin or upper respiratory tract, causing little serious concern, threatening the effectiveness of the last or no harm. On occasion, however, they become translocated available options for treatment of potentially fatal Staphylo- to sites that are normally sterile, such as the blood or lungs, coccus strains. where they may have serious harmful effects (6). Many viru- It seems clear that a considered and comprehensive strategy lence factors, for example in Staphylococcus aureus, are carried for antibiotic use is essential, permitting the intelligent de- on plasmids, and can be exchanged among different strains. -

Randomised Trial to Compare the Immunogenicity and Safety of a CRM Or TT Conjugated Quadrivalent Meningococcal Vaccine in Teenag
Title Page Randomised trial to compare the immunogenicity and safety of a CRM or TT 1 2 conjugated quadrivalent meningococcal vaccine in teenagers who received a 3 4 5 CRM or TT conjugated serogroup C vaccine at preschool age 6 7 8 9 1,2 1,3 1 10 David A. Ishola , FFPH; Nick Andrews , PhD; Pauline Waight , BSc; Chee-Fu 11 12 Yung1,6, FFPH; Jo Southern1, PhD; Xilian Bai4, PhD; Helen Findlow4, PhD; Mary 13 14 5 5 5 4 15 Matheson , PhD; Anna England , MSc; Bassam Hallis , PhD; Jamie Findlow , PhD; 16 4 1 17 Ray Borrow , PhD; Elizabeth Miller , FRCPath. 18 19 1. Immunisation Department, Public Health England (PHE), London, UK 20 21 22 2. Department of Infection and Population Health, University College London, 23 24 London, UK 25 26 27 3. Statistics, Modelling, and Economics Department, PHE London, UK 28 29 4. Vaccine Evaluation Unit, PHE, Manchester Medical Microbiology Partnership, 30 31 32 Manchester Royal Infirmary, Manchester, UK 33 34 5. Microbiology Services, PHE, Porton Down, Salisbury, UK 35 36 6. Department of Clinical Epidemiology, Communicable Disease Centre, Tan Tock 37 38 39 Seng Hospital, Singapore. 40 41 Correspondence: David Ishola, University College London, Department of Infection 42 43 44 and Population Health, 222 Euston Road, London NW1 2DA, UK. Tel: +44 45 46 (0)7946412701. Fax: +44 (0)20 83277404. E-mail: [email protected] 47 48 49 Address for reprints: Not applicable (reprints not available). 50 51 Key words: Meningococcal, vaccine, teenagers, antibody, randomised trial 52 53 54 Abbreviated title: Teenage MenACWY booster vaccination: Randomised trial 55 56 Running head title: Teenage MenACWY booster vaccination 57 58 59 60 61 62 1 63 64 65 CONFLICTS OF INTEREST AND SOURCE OF FUNDING: 1 2 Funding and support: This report is independent research commissioned and 3 4 5 funded by the UK Department of Health Policy Research Programme (National 6 7 Vaccine Evaluation Consortium, 039/0031). -

Locations of Horseheath Records
Locations of Horseheath records Part of Horseheath Village Archives Locations of Horseheath records Cambridgeshire Archives and Local Studies Office Formerly Cambridge Record Office, this holds census, church and parish records along with over 300 other items concerning Horseheath. It is located in the Cambridgeshire County Council Offices, Shire Hall, Castle Street, Castle Hill, Cambridge CB3 0AP Tel.01223 699 399 The Cambridgeshire Collection This is located within the Cambridge Central Library and contains a wide variety of information relating to Cambridgeshire and its people. It includes books, pamphlets, magazines, maps from 1574, illustrations from the 17 th c, newspapers from 1762, press cuttings from 1960 and ephemera of all kinds. The Cambridge Antiquarian Society Photographic Archive is held in the Cambridgeshire Collection, as is the studio portrait archive of the former Cambridge photographers J Palmer Clarke and Ramsey and Muspratt. Family historians have access to many sources listing former residents of the county; directories, electoral rolls, poll books, parish register transcripts, etc. Cambridge University Library List follows. Cemeteries The Monumental Inscriptions in the graveyard of All Saints from the 15th century-1981 are recorded in Cambridgeshire Archives and Local Studies in the Council Offices, Shire Hall, Castle Hill. A copy of the original manuscript of ‘Inscriptions on gravestones and internal monuments’, by Catherine Parsons, 1897 appears in the @all Saints’ Church sewction of Horseheath Village Archives. Census The Census Records from 1841-1911 can be found in the Cambridgeshire Archives and Local Studies Office and at the Family Records Centre in London (see below). The 1881 Census is available in searchable form on www.familysearch.org. -

Valacyclovir Reduced Genital Herpes Transmission in Couples Discordant for Herpes Simplex Virus Type 2 Infection Corey L, Wald A, Patel R, Et Al
146 THERAPEUTICS Evid Based Med: first published as 10.1136/ebm.9.5.146 on 30 September 2004. Downloaded from Valacyclovir reduced genital herpes transmission in couples discordant for herpes simplex virus type 2 infection Corey L, Wald A, Patel R, et al. Once-daily valacyclovir to reduce the risk of transmission of genital herpes. N Engl J Med 2004;350:11–20. Clinical impact ratings GP/FP/Primary care wwwwwwq Infectious diseases wwwwwqq ............................................................................................................................... In heterosexual couples who are serologically discordant for herpes simplex virus type 2 (HSV-2) infection, does once Q daily valacyclovir reduce the sexual transmission of genital herpes? METHODS MAIN RESULTS The table shows the results. Design: randomised placebo controlled trial. CONCLUSION In heterosexual couples discordant for herpes simplex virus type 2 infection, valacyclovir reduced transmission of infection. Allocation: concealed.* Commentary Blinding: blinded {participants, healthcare providers, data revious studies have shown that antiviral drugs can reduce the collectors, data analysts, and outcome assessors}À.* frequency of recurrence and subclinical shedding of viral particles.1 Follow up period: 8 months. P This important, large, well designed trial by Corey et al is the first to show an effect on the transmission of HSV-2 infection to an uninfected partner. In this study, the reduction in transmission was limited; 62 partners had Setting: 96 sites in the US, Canada, Europe, Latin America, and to take the drug daily for 8 months to prevent 1 infection, and 57 partners Australia. had to take the drug daily to prevent overall acquisition of HSV-2 infection. 2 independent predictors were found in addition to the drugs: Participants: 1498 couples >18 years who were women as the susceptible partners (hazard ratio [HR] 3.3) and duration immunocompetent, heterosexual, monogamous, in good health, of HSV-2 infection ,2 years (HR 2.9). -

The NHS's Role in the Public's Health
The NHS’s role in the public’s health A report from the NHS Future Forum Workstream members Vicky Bailey ‐ Chair, NHS’s role in the public’s health group Chief Operating Officer, Principia Rushcliffe Clinical Commissioning Group Ash Soni ‐ Chair, NHS’s role in the public’s health group Community Pharmacist; Clinical Network Lead, NHS Lambeth Dr Charles Alessi Senior GP Partner, The Churchill Practice Dr Frank Atherton President, Association of Directors of Public Health; Director of Public Health, North Lancashire Cluster Ratna Dutt Chief Executive, Race Equality Foundation Paul Farmer Chief Executive, Mind Moira Gibb Chief Executive, London Borough of Camden; Chair, Social Work Task Force Chris Long Chief Executive, Humber Cluster Claire Marshall Head of Professions, Heatherwood and Wexham Park Hospitals NHS Foundation Trust Dr Tim Riley Chief Executive, Wellstate Group Ltd Tom Riordan Chief Executive, Leeds City Council Dr Robina Shah Chair, Stockport NHS Foundation Trust Professor Jimmy Steele Head of School and Professor of Oral Health Services Research, School of Dental Sciences, Newcastle University Gill Walton Director of Midwifery, Portsmouth Hospitals NHS Trust Contents Contents.........................................................................................................................2 Foreword........................................................................................................................3 Terms used in this report...............................................................................5 -

Msc Management
Programme Specification (Master’s Level) MSc Management This document provides a definitive record of the main features of the programme and the learning outcomes that a typical student may reasonably be expected to achieve and demonstrate if s/he takes full advantage of the learning opportunities provided. This programme specification is intended as a reference point for prospective students, current students, external examiners and academic and support staff involved in delivering the programme and enabling student development and achievement. Programme Information Programme Title Management Award(s) MSc Programme Code N1UF Awarding Institution Imperial College London Teaching Institution Imperial College London Faculty Imperial College Business School Department Imperial College Business School Mode and Period of Study 1 calendar year full-time (12 months) Cohort Entry Points Annually in September Relevant QAA Benchmark Statement(s) and/or Master’s Degrees in Business and Management other external reference points Total Credits ECTS: 90 CATS: 180 FHEQ Level Level 7 EHEA Level 2nd cycle External Accreditor(s) AMBA, EQUIS, AACSB International Specification Details Student cohorts covered by specification 2016/17 entry Person responsible for the specification Veronica Russell, Teaching & Quality Manager Date of introduction of programme October 2005 Date of programme specification/revision September 2016 Page 1 of 11 Description of Programme Contents The MSc in Management is offered over 12 months full-time. The programme content reflects the contemporary and relevant management skills necessary for managing in turbulent environments. In particular the programme will equip the participants with conceptual and practical skills, and enable them to analyse and solve challenging problems. The programme combines academic rigour and practical relevance. -

Cambridgeshire Archaeology JIGSAW “Piecing Together Cambridgeshire’S Past
Cambridgeshire County Council JIGSAW Project Final report 2007 Cambridgeshire Archaeology JIGSAW “piecing together Cambridgeshire’s Past Final Report April 2007 Prepared By The Market Research Group (MRG), Bournemouth University, On Behalf Of Cambridgeshire County Council www.themarketresearchgroup.co.uk Page a Cambridgeshire County Council JIGSAW Project Final report 2007 Contents Executive Summary ........................................................................ 1 1.0: Background .............................................................................. 3 1.1: The Market Research Group (MRG)........................................ 3 1.2: Cambridgeshire County Council .............................................. 4 2.0: Research Aims & Objectives................................................... 6 3.0: Outline Methodology................................................................ 8 3.1: Audience Research - Existing Users ....................................... 8 3.2: Audience Research - Potential Users ...................................... 9 3.3: Audience Research – JIGSAW Focus Groups ...................... 11 4.0: Findings –Cambridgeshire Archaeology users results...... 12 5.0: Findings – Potential users or non user survey ................... 39 6.0: Findings – Castle celebration event (non users) ................ 79 7.0: Findings - Schools – qualitative results............................. 101 8.0: Findings – Focus group results.......................................... 116 8.1: Users and non users focus groups -

H 955 Great Britain
Great Britain H 955 BACKGROUND: The heading Great Britain is used in both descriptive and subject cataloging as the conventional form for the United Kingdom, which comprises England, Northern Ireland, Scotland, and Wales. This instruction sheet describes the usage of Great Britain, in contrast to England, as a subject heading. It also describes the usage of Great Britain, England, Northern Ireland, Scotland, and Wales as geographic subdivisions. 1. Great Britain vs. England as a subject heading. In general assign the subject heading Great Britain, with topical and/or form subdivisions, as appropriate, to works about the United Kingdom as a whole. Assign England, with appropriate subdivision(s), to works limited to that country. Exception: Do not use the subdivisions BHistory or BPolitics and government under England. For a work on the history, politics, or government of England, assign the heading Great Britain, subdivided as required for the work. References in the subject authority file reflect this practice. Use the subdivision BForeign relations under England only in the restricted sense described in the scope note under EnglandBForeign relations in the subject authority file. 2. Geographic subdivision. a. Great Britain. Assign Great Britain directly after topics for works that discuss the topic in relation to Great Britain as a whole. Example: Title: History of the British theatre. 650 #0 $a Theater $z Great Britain $x History. b. England, Scotland, Northern Ireland, and Wales. Assign England, Scotland, Northern Ireland, or Wales directly after topics for works that limit their discussion to the topic in relation to one of the four constituent countries of Great Britain.