UNIVERSITY of CALIFORNIA, SAN DIEGO Characterization Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exceptional Conservation of Horse–Human Gene Order on X Chromosome Revealed by High-Resolution Radiation Hybrid Mapping
Exceptional conservation of horse–human gene order on X chromosome revealed by high-resolution radiation hybrid mapping Terje Raudsepp*†, Eun-Joon Lee*†, Srinivas R. Kata‡, Candice Brinkmeyer*, James R. Mickelson§, Loren C. Skow*, James E. Womack‡, and Bhanu P. Chowdhary*¶ʈ *Department of Veterinary Anatomy and Public Health, ‡Department of Veterinary Pathobiology, College of Veterinary Medicine, and ¶Department of Animal Science, College of Agriculture and Life Science, Texas A&M University, College Station, TX 77843; and §Department of Veterinary Pathobiology, University of Minnesota, 295f AS͞VM, St. Paul, MN 55108 Contributed by James E. Womack, December 30, 2003 Development of a dense map of the horse genome is key to efforts ciated with the traits, once they are mapped by genetic linkage aimed at identifying genes controlling health, reproduction, and analyses with highly polymorphic markers. performance. We herein report a high-resolution gene map of the The X chromosome is the most conserved mammalian chro- horse (Equus caballus) X chromosome (ECAX) generated by devel- mosome (18, 19). Extensive comparisons of structure, organi- oping and typing 116 gene-specific and 12 short tandem repeat zation, and gene content of this chromosome in evolutionarily -markers on the 5,000-rad horse ؋ hamster whole-genome radia- diverse mammals have revealed a remarkable degree of conser tion hybrid panel and mapping 29 gene loci by fluorescence in situ vation (20–22). Until now, the chromosome has been best hybridization. The human X chromosome sequence was used as a studied in humans and mice, where the focus of research has template to select genes at 1-Mb intervals to develop equine been the intriguing patterns of X inactivation and the involve- orthologs. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

BMC Biology Biomed Central
BMC Biology BioMed Central Research article Open Access Normal histone modifications on the inactive X chromosome in ICF and Rett syndrome cells: implications for methyl-CpG binding proteins Stanley M Gartler*1,2, Kartik R Varadarajan2, Ping Luo2, Theresa K Canfield2, Jeff Traynor3, Uta Francke3 and R Scott Hansen2 Address: 1Department of Medicine, University of Washington, Seattle, WA, USA, 2Department of Genome Sciences, University of Washington, Seattle, WA, USA and 3Department of Genetics, Stanford University, Stanford, CA, USA Email: Stanley M Gartler* - [email protected]; Kartik R Varadarajan - [email protected]; Ping Luo - [email protected]; Theresa K Canfield - [email protected]; Jeff Traynor - [email protected]; Uta Francke - [email protected]; R Scott Hansen - [email protected] * Corresponding author Published: 20 September 2004 Received: 23 June 2004 Accepted: 20 September 2004 BMC Biology 2004, 2:21 doi:10.1186/1741-7007-2-21 This article is available from: http://www.biomedcentral.com/1741-7007/2/21 © 2004 Gartler et al; licensee BioMed Central Ltd. This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: In mammals, there is evidence suggesting that methyl-CpG binding proteins may play a significant role in histone modification through their association with modification complexes that can deacetylate and/or methylate nucleosomes in the proximity of methylated DNA. We examined this idea for the X chromosome by studying histone modifications on the X chromosome in normal cells and in cells from patients with ICF syndrome (Immune deficiency, Centromeric region instability, and Facial anomalies syndrome). -
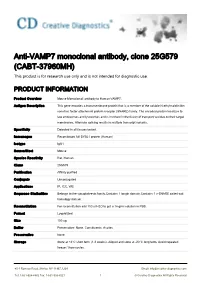
Anti-VAMP7 Monoclonal Antibody, Clone 25G579 (CABT-37960MH) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-VAMP7 monoclonal antibody, clone 25G579 (CABT-37960MH) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse Monoclonall antibody to Human VAMP7. Antigen Description This gene encodes a transmembrane protein that is a member of the soluble N-ethylmaleimide- sensitive factor attachment protein receptor (SNARE) family. The encoded protein localizes to late endosomes and lysosomes and is involved in the fusion of transport vesicles to their target membranes. Alternate splicing results in multiple transcript variants. Specificity Detected in all tissues tested. Immunogen Recombinant full SYBL1 protein (Human) Isotype IgG1 Source/Host Mouse Species Reactivity Rat, Human Clone 25G579 Purification Affinity purified Conjugate Unconjugated Applications IP, ICC, WB Sequence Similarities Belongs to the synaptobrevin family.Contains 1 longin domain.Contains 1 v-SNARE coiled-coil homology domain. Reconstitution For reconstitution add 100 ul H2O to get a 1mg/ml solution in PBS. Format Lyophilized Size 100 ug Buffer Preservative: None. Constituents: Ascites Preservative None Storage Store at +4°C short term (1-2 weeks). Aliquot and store at -20°C long term. Avoid repeated freeze / thaw cycles. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved GENE INFORMATION Gene Name VAMP7 vesicle-associated membrane protein 7 [ Homo sapiens ] Official Symbol VAMP7 Synonyms VAMP7; vesicle-associated -

Discovery of Candidate Genes for Stallion Fertility from the Horse Y Chromosome
DISCOVERY OF CANDIDATE GENES FOR STALLION FERTILITY FROM THE HORSE Y CHROMOSOME A Dissertation by NANDINA PARIA Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2009 Major Subject: Biomedical Sciences DISCOVERY OF CANDIDATE GENES FOR STALLION FERTILITY FROM THE HORSE Y CHROMOSOME A Dissertation by NANDINA PARIA Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY Approved by: Chair of Committee, Terje Raudsepp Committee Members, Bhanu P. Chowdhary William J. Murphy Paul B. Samollow Dickson D. Varner Head of Department, Evelyn Tiffany-Castiglioni August 2009 Major Subject: Biomedical Sciences iii ABSTRACT Discovery of Candidate Genes for Stallion Fertility from the Horse Y Chromosome. (August 2009) Nandina Paria, B.S., University of Calcutta; M.S., University of Calcutta Chair of Advisory Committee: Dr. Terje Raudsepp The genetic component of mammalian male fertility is complex and involves thousands of genes. The majority of these genes are distributed on autosomes and the X chromosome, while a small number are located on the Y chromosome. Human and mouse studies demonstrate that the most critical Y-linked male fertility genes are present in multiple copies, show testis-specific expression and are different between species. In the equine industry, where stallions are selected according to pedigrees and athletic abilities but not for reproductive performance, reduced fertility of many breeding stallions is a recognized problem. Therefore, the aim of the present research was to acquire comprehensive information about the organization of the horse Y chromosome (ECAY), identify Y-linked genes and investigate potential candidate genes regulating stallion fertility. -

Chromatin Structure of the Inactive X Chromosome
CHROMATIN STRUCTURE OF THE INACTIVE X CHROMOSOME by Sandra L. Gilbert B.A. Biology and B.A. Economics University of Pennsylvania, 1990 Submitted to the Department of Biology in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Biology at the Massachusetts Institute of Technology September, 1999 © 1999 Massachusetts Institute of Technology All rights reserved Signature of Author ................................................................................ ..... .... .. .... .. .. ... HUS Department of Biology August 19,1999 MASSACHUSETTS INSTITU 1OFTECHNOLOGY '7 Ce rtifie d by ................. .................... ............ ......................................................... Phillip A. Sharp Salvador E. Luria Professor of Biology Thesis Supervisor A cce pte d by ........................................................................................ ...-- .* ... Terry Orr-Weaver Professor of Biology Chairman, Committee for Graduate Students 2 ABSTRACT X-inactivation is the unusual mode of gene regulation by which most genes on one of the two X chromosomes in female mammalian cells are transcriptionally silenced. The underlying mechanism for this widespread transcriptional repression is unknown. This thesis investigates two key aspects of the X-inactivation process. The first aspect is the correlation between chromatin structure and gene expression from the inactive X (Xi). Two features of the Xi chromatin - DNA methylation and late replication timing - have been shown to correlate with silencing -

A Strategic Research Alliance: Turner Syndrome and Sex Differences
A strategic research alliance: Turner syndrome and sex differences The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Roman, Adrianna K. San and David C. Page. “A strategic research alliance: Turner syndrome and sex differences.” American journal of medical genetics. Part C, Seminars in medical genetics 181 (2019): 59-67 © 2019 The Author(s) As Published 10.1002/AJMG.C.31677 Publisher Wiley Version Author's final manuscript Citable link https://hdl.handle.net/1721.1/125103 Terms of Use Creative Commons Attribution-Noncommercial-Share Alike Detailed Terms http://creativecommons.org/licenses/by-nc-sa/4.0/ HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Am J Med Manuscript Author Genet C Semin Manuscript Author Med Genet. Author manuscript; available in PMC 2019 March 12. Published in final edited form as: Am J Med Genet C Semin Med Genet. 2019 March ; 181(1): 59–67. doi:10.1002/ajmg.c.31677. A strategic research alliance: Turner syndrome and sex differences Adrianna K. San Roman1 and David C. Page1,2,3 1Whitehead Institute, Cambridge, MA 02142, USA 2Howard Hughes Medical Institute, Whitehead Institute, Cambridge, MA 02142 3Department of Biology, Massachusetts Institute of Technology, Cambridge, MA 02139 Abstract Sex chromosome constitution varies in the human population, both between the sexes (46,XX females and 46,XY males), and within the sexes (for example, 45,X and 46,XX females, and 47,XXY and 46,XY males). Coincident with this genetic variation are numerous phenotypic differences between males and females, and individuals with sex chromosome aneuploidy. -

Chromosome Territory Reorganization in a Human Disease with Altered DNA Methylation
Chromosome territory reorganization in a human disease with altered DNA methylation Maria R. Matarazzo*, Shelagh Boyle†, Maurizio D’Esposito*‡, and Wendy A. Bickmore†‡ *Institute of Genetics and Biophysics ‘‘Adriano Buzzati Traverso,’’ Consiglio Nazionale delle Ricerche, Via P. Castellino 111, 80131 Naples, Italy; and †Medical Research Council Human Genetics Unit, Institute of Genetics and Molecular Medicine, University of Edinburgh, Crewe Road, Edinburgh EH4 2XU, United Kingdom Edited by Mark T. Groudine, Fred Hutchinson Cancer Research Center, Seattle, WA, and approved September 4, 2007 (received for review April 2, 2007) Chromosome territory (CT) organization and chromatin condensa- nodeficiency centromeric instability facial anomalies (ICF) syn- tion have been linked to gene expression. Although individual drome patients (14) lead to loss of DNA methylation at specific genes can be transcribed from inside CTs, some regions that have genomic sites (15, 16). Prominent sites of hypomethylation in constitutively high expression or are coordinately activated loop ICF are satellite DNAs in the juxtacentromeric heterochromatin out from CTs and decondense. The relationship between epige- at chromosome regions 1qh, 16qh, and 9qh, and aberrant netic marks, such as DNA methylation, and higher-order chromatin association of the satellite II-rich 1qh and 16qh regions has been structures is largely unexplored. DNMT3B mutations in immuno- seen in nuclei of ICF cells (17). Sites on the female inactive X deficiency centromeric instability facial anomalies (ICF) syndrome chromosome (Xi), especially CpG islands, are also hypomethy- result in loss of DNA methylation at particular sites, including CpG lated in ICF syndrome. This does not reflect a chromosome-wide islands on the inactive X chromosome (Xi). -

DNA Methylation in Transcriptional Repression of Two Differentially Expressed X-Linked Genes, GPC3 and SYBL1
Proc. Natl. Acad. Sci. USA Vol. 96, pp. 616–621, January 1999 Genetics DNA methylation in transcriptional repression of two differentially expressed X-linked genes, GPC3 and SYBL1 i REID HUBER*†‡,R.SCOTT HANSEN§,MARIA STRAZZULLO¶,GINA PENGUE ,RICHARD MAZZARELLA**, MICHELE D’URSO¶,DAVID SCHLESSINGER*, GIUSEPPE PILIA††,STANLEY M. GARTLER§,§§, AND MAURIZIO D’ESPOSITO¶ *Laboratory of Genetics, National Institute on Aging, National Institutes of Health, Baltimore, MD 21224; Departments of §Medicine and §§Genetics, University of Washington, Seattle, WA 98195; ¶International Institute of Genetics and Biophysics, 80125 Naples, Italy; iDepartment of Internal Medicine and **Institute for Biomedical Computing, Washington University, St. Louis, MO 63110; and ††Instituto di Ricerca, Talassemie e Anemie Mediterranee, 09100 Cagliari, Italy Contributed by Stanley M. Gartler, November 9, 1998 ABSTRACT Methylation of CpG islands is an established 5-azacytidine results in the transcriptional activation of many transcriptional repressive mechanism and is a feature of repressed genes (7). silencing in X chromosome inactivation. Housekeeping genes Although the way in which methylation may influence that are subject to X inactivation exhibit differential methyl- transcription is beginning to be understood (8), the degree to ation of their CpG islands such that the inactive alleles are which it is necessary andyor sufficient for repression in various hypermethylated. In this report, we examine two contrasting cases remains unknown. To analyze the influence of methyl- X-linked genes with CpG islands for regulation by DNA ation on transcription further, we have compared the extent methylation: SYBL1, a housekeeping gene in the Xq pseudo- and effects of methylation on two genes, each of which is autosomal region, and GPC3, a tissue-specific gene in Xq26 repressed strongly by two distinct mechanisms. -

NIH Public Access Author Manuscript Hepatology
NIH Public Access Author Manuscript Hepatology. Author manuscript; available in PMC 2012 December 11. Published in final edited form as: Hepatology. 2007 August ; 46(2): 548–557. doi:10.1002/hep.21682. Genome-level analysis of genetic regulation of liver gene expression networks $watermark-text $watermark-text $watermark-text Daniel Gatti1,¶, Akira Maki1,¶, Elissa J. Chesler2,¶, Roumyana Kirova2, Oksana Kosyk1, Lu Lu3, Kenneth F. Manly, Yanhua Qu3, Robert W. Williams3, Andy Perkins4, Michael A. Langston4, David W. Threadgill5,&, and Ivan Rusyn1,&,* Daniel Gatti: [email protected]; Akira Maki: [email protected]; Elissa J. Chesler: [email protected]; Roumyana Kirova: [email protected]; Oksana Kosyk: [email protected]; Lu Lu: [email protected]; Kenneth F. Manly: [email protected]; Yanhua Qu: [email protected]; Robert W. Williams: [email protected]; Andy Perkins: [email protected]; Michael A. Langston: [email protected]; David W. Threadgill: [email protected] 1Department of Environmental Sciences and Engineering, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina 27599 2Life Sciences Division, Oak Ridge National Laboratory, P.O. Box 2008, Oak Ridge, TN 37831 3Department of Anatomy and Neurobiology, University of Tennessee Health Science Center, Memphis, TN 38163 4Department of Computer Science, University of Tennessee, Knoxville, TN 37996 5Department of Genetics, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina 27599 Abstract Liver is the primary site for metabolism of nutrients, drugs and chemical agents. While metabolic pathways are complex and tightly regulated, genetic variation among individuals, reflected in variation in gene expression levels, introduces complexity into research on liver disease. -

Meta-Analysis of Gene Expression in Individuals with Autism Spectrum Disorders
Meta-analysis of Gene Expression in Individuals with Autism Spectrum Disorders by Carolyn Lin Wei Ch’ng BSc., University of Michigan Ann Arbor, 2011 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF Master of Science in THE FACULTY OF GRADUATE AND POSTDOCTORAL STUDIES (Bioinformatics) The University of British Columbia (Vancouver) August 2013 c Carolyn Lin Wei Ch’ng, 2013 Abstract Autism spectrum disorders (ASD) are clinically heterogeneous and biologically complex. State of the art genetics research has unveiled a large number of variants linked to ASD. But in general it remains unclear, what biological factors lead to changes in the brains of autistic individuals. We build on the premise that these heterogeneous genetic or genomic aberra- tions will converge towards a common impact downstream, which might be reflected in the transcriptomes of individuals with ASD. Similarly, a considerable number of transcriptome analyses have been performed in attempts to address this question, but their findings lack a clear consensus. As a result, each of these individual studies has not led to any significant advance in understanding the autistic phenotype as a whole. The goal of this research is to comprehensively re-evaluate these expression profiling studies by conducting a systematic meta-analysis. Here, we report a meta-analysis of over 1000 microarrays across twelve independent studies on expression changes in ASD compared to unaffected individuals, in blood and brain. We identified a number of genes that are consistently differentially expressed across studies of the brain, suggestive of effects on mitochondrial function. In blood, consistent changes were more difficult to identify, despite individual studies tending to exhibit larger effects than the brain studies. -

Variability in Interpreting and Reporting Copy Number Changes Detected by Array-Based Technology in Clinical Laboratories Karen D
ARTICLE Variability in interpreting and reporting copy number changes detected by array-based technology in clinical laboratories Karen D. Tsuchiya, MD1, Lisa G. Shaffer, PhD2, Swaroop Aradhya, PhD3, Julie M. Gastier-Foster, PhD4, Ankita Patel, PhD5, M. Katharine Rudd, PhD6, Julie Sanford Biggerstaff, PhD7, Warren G. Sanger, PhD8, Stuart Schwartz, PhD9,10, James H. Tepperberg, PhD9, Erik C. Thorland, PhD11, Beth A. Torchia, PhD2, and Arthur R. Brothman, PhD12 Purpose: The purpose of this study was to assess the variability in in normal control populations, determination of the clinical interpretation and reporting of copy number changes that are detected significance of individually rare CNCs can be much more by array-based technology in the clinical laboratory. Methods: Thirteen difficult. different copy number changes, detected by array comparative genomic Recently, approaches for evaluating the pathogenicity of 1–3 hybridization, that have not been associated with an abnormal pheno- CNCs in the diagnostic setting have been proposed. One of type in the literature were evaluated by directors from 11 different the most useful criteria for distinguishing a benign from a clinical laboratories to determine how they would interpret and report pathogenic CNC is whether it is de novo or inherited. In the findings. Results: For none of the thirteen copy number changes general, with the exception of CNCs that demonstrate variable was there complete agreement in the interpretation of the clinical expressivity and decreased penetrance, de novo CNCs are more significance of the deletion or duplication. For some cases, the inter- likely to be pathogenic compared with CNCs inherited from a pretations ranged from normal to abnormal.