Spring 2017 Special Edition: House Staff
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peace Envoy Moves Stir New End-War Speculation WASHINGTON (AP) - Some Diplomats Here and in an Uneasy Thieu That Presi- Paris Monday, Will Confer the Paris Talks
Police Probe Triple SEE STORY PACE 2 The Weather ,v Sunny and pleasant today,' THEDAILY FINAL clear and cool tonight Tomor- row fair and a little warmer. Red Bank, Freehold Long Branch EDITION 30 PACES Monniouth County's Outstanding Home Newspaper VOL. 95 NO. 37 RED BANK, NJ. WEDNESDAY. AIJGUST 16.1972 TEN CENTS iiiiiiiuiiNiiniiiiiiii Cahill Plans Low-Key Role In Republican Convention By JAMES U.RUBIN the up-coming gathering of ture soundly defeated his tax culties may be a liability. expect this," said Cahill, who the GOP ranks in Miami reform program. "The President will be twice has attended con- TRENTON (AP) - Gov. Beach. Cahill is the chairman of the judged on what he has done in ventions as'an observer. William T. Cahill, anticipating When plans for the con- Nixon-Agnew campaign in the last four years as Bill "They recognize there is no an uneventful Republican Na- vention were made at the re- New Jersey, a key north- Cahill will be judged on his contest. It's a recognition that tional Convention, says be will cent National Governors Con- eastern state and the eighth record;" the governor said. the overwhelming number of play a subdued, low-key role ference, Cahill said, "1 knew largest in the nation. Furthermore, he remarked, Republicans are satisfied with in Miami Beach next week. at the time the President However, he is leaving the "The people in this state know the administration." Cahill, the chairman of New would be toe candidate and day-to-day chores of manag- Bill Cahill for what he is. -
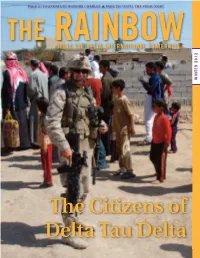
2012 Winter Vol 136 No 1
PAGE 8 | FOUNDATION HONORS CHARLES p PAGE 38 | UNTIL THE FINAL SNAP THE RAINBOW DELTA TAU DELTA INTERNATIONAL FRATERNITY WINTER 2012 The Citizens of Delta Tau Delta In partnership with 36 other fraternities and sororities committed to ending bullying and hazing on college campuses CONTENTS THE RAINBOW | VOLUME 136, NO. 1 | WINTER 2012 28 Cover Story Think Green We the Citizens, of Delta Tau Delta 5 Fraternity Headlines Insert topics he Expansions for Fall 2012 Delaware and UCSB Receive Charters Quinnipiac Brothers Grow ‘Staches for Cash PERIODICAL STATEMENT The Rainbow (ISSN 1532-5334) is published twice annually for $10 per year by Delta Tau Delta Fraternity at 10000 Allisonville Road, 10 A Lifetime of Service Fishers, Indiana 46038-2008; Telephone 1-800- MAGAZINE MISSION DELTSXL; http://www.delts.org. Periodical Insert topics Ken File Reflects on His Time Serving Delta Tau Delta p Inform members of the events, postage paid at Fishers, Indiana and at activities and concerns of inter- additional mailing offices. POSTMASTER: Send re address changes to Delta Tau Delta Fraternity, est to members of the Fraternity. 10000 Allisonville Road, Fishers, Indiana 12 Annual Report p Attract and involve members of 46038-2008. Canada Pub Agree #40830557. the Fraternity via appropriate Canada return to: Station A, P.O. Box 54, coverage, information and opin- Windsor, ON N9A 6J5 [email protected] ion stories. STATEMENT OF OWNERSHIP p Educate present and potential 1. Publication Title –THE RAINBOW; 14 Alumni in the News members on pertinent issues, 2. Publication No.–1532-5334; 3. Filing Date– Sept. 25, 2008; 4. Issue Frequency–Biannual; Insert topi persons, events and ideas so 5. -

Fostering Healthy Neighborhoods
Fostering Healthy Neighborhoods RESEARCH BRIEF Alignment across the community development, health and financial well-being sectors. A PROJECT AND REPORT LED BY Build Healthy Places Network Prosperity Now Financial Health Network Table of Contents 3 Overview 7 Key Findings 13 Conclusion 14 Appendix A – Examples of Existing Work 18 Appendix B – Public Health and Healthcare Sectors Overview 24 Appendix C – Community Development Sector Overview 27 Appendix D – Financial Well-being Sector Overview 30 Appendix E – Interviews 30 Appendix F – Focus Groups 32 Appendix G – List of Resources Support for this report was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the Foundation. Research and writing contributor Paul DeManche 2 FOSTERING HEALTHY NEIGHBORHOODS | 3 Overview Substantial evidence links financial well-being and health. As income and wealth increase or decrease, so does health. Individuals and families with more wealth and higher incomes are better able to access the material and physical conditions that facilitate good health and are less likely to suffer from the mental and physical effects of financial stress caused by income volatility, insufficient savings, and unmanageable debt. The physical, social, and economic conditions FIGURE 1. FRAMEWORK FOR in our neighborhoods have a significant impact NEIGHBORHOODS THAT SUPPORT on both our health and financial well-being HEALTH AND FINANCIAL because they shape the opportunities we have WELLBEING and the choices that are available -

Why Investigative Journalism Matters
Credits © 2015 by The Boston Globe All rights reserved under the Pan-American and International Copyright Conventions. This book may not be reproduced in whole or in part, in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system now known or hereafter in- vented, without written permission from the publisher. 1 Spotlight is launched On September 27, 1970, The Boston Globe announced in the newspaper the creation of a “special, three-man investigative team” that would provide deeper coverage on the stories driving the discus- sions of the day. The team was modeled after the “Insight” team that worked at the Sunday Times of London, which had gained recognition as a leading investigative newspaper authority. The Globe’s announcement got straight to the point for its readers. “The team’s mission will be to reconstruct major news events as rapidly and comprehensively as possible, with an emphasis on the ‘why’ rather than the ‘what’ of an event. The unit will also seek to expose public corruption and malfeasance. Articles by the team will appear under the signature of “Spotlight.” Almost a half-century later, that mission endures, as Spotlight remains the oldest, continuously op- erating investigative unit at a newspaper in the United States. With its aggressive coverage of the Catholic church, the healthcare industry, the shady world of taxicabs, and the unregulated college housing crisis, to name a few examples, the Spotlight team embodies investigative journalism at its best. Spotlight gives a voice to the voiceless, by shining a light into corners of our society that demand accountability. -

The Testimony of William Bulger Hearin
THE NEXT STEP IN THE INVESTIGATION OF THE USE OF INFORMANTS BY THE DEPARTMENT OF JUSTICE: THE TESTIMONY OF WILLIAM BULGER HEARING BEFORE THE COMMITTEE ON GOVERNMENT REFORM HOUSE OF REPRESENTATIVES ONE HUNDRED EIGHTH CONGRESS FIRST SESSION JUNE 19, 2003 Serial No. 108–41 Printed for the use of the Committee on Government Reform ( Available via the World Wide Web: http://www.gpo.gov/congress/house http://www.house.gov/reform U.S. GOVERNMENT PRINTING OFFICE 89–004 PDF WASHINGTON : 2003 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2250 Mail: Stop SSOP, Washington, DC 20402–0001 VerDate 11-MAY-2000 09:36 Oct 02, 2003 Jkt 000000 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 D:\DOCS\89004 HGOVREF1 PsN: HGOVREF1 COMMITTEE ON GOVERNMENT REFORM TOM DAVIS, Virginia, Chairman DAN BURTON, Indiana HENRY A. WAXMAN, California CHRISTOPHER SHAYS, Connecticut TOM LANTOS, California ILEANA ROS-LEHTINEN, Florida MAJOR R. OWENS, New York JOHN M. MCHUGH, New York EDOLPHUS TOWNS, New York JOHN L. MICA, Florida PAUL E. KANJORSKI, Pennsylvania MARK E. SOUDER, Indiana CAROLYN B. MALONEY, New York STEVEN C. LATOURETTE, Ohio ELIJAH E. CUMMINGS, Maryland DOUG OSE, California DENNIS J. KUCINICH, Ohio RON LEWIS, Kentucky DANNY K. DAVIS, Illinois JO ANN DAVIS, Virginia JOHN F. TIERNEY, Massachusetts TODD RUSSELL PLATTS, Pennsylvania WM. LACY CLAY, Missouri CHRIS CANNON, Utah DIANE E. WATSON, California ADAM H. PUTNAM, Florida STEPHEN F. LYNCH, Massachusetts EDWARD L. SCHROCK, Virginia CHRIS VAN HOLLEN, Maryland JOHN J. -

Conflict of Interest, Ethics Among Tops
In this issue: car care supplement I m t r n a l M e m b e r M e m b e r MATAWAN , NEW JERSEY, Thursday, May 25, 1972 Single Copy Fifteen Cants' 103rd YEAR M |h WEEK National Newspaper Association N e w Je r s e y Press Association BEADLESTON SPEAKER Conflict of interest, ethics among tops MATAWAN - Sen. Alfred “ accomplishments’' in the would be state-operated and Also mentioned were the package, saying passage N. Beadlcston, Republican legislature during this year, away from the local tracks so making the New Jersey would ‘‘take money out of the majority leader spoke discussed what would be as to not hurt their business Parole Board a full-time right hand pockct and put less yesterday at the Matawan debated at the "improperly as had been done in New York board of three men instead of into the left hand pocket” . Chamber of Commerce termed special session" in off-track betting; ratification a five man parttime board in Included in the package is a election luncheon at Don June, the lax reform addition to bills lo help personal income tax and a Quixote Inn where he package, and answered some rehabilitate parolees; a statewide real estate tax. discussed some of the major <|uestions from the floor. constitutional amendment Sen. Beadleston said the KICK-OFF DINNER-The Hasilian Father of Mariapocli, Malawan, held a building fund legislation in the senate this Listed were adoption of a making 1 state attorney measures would “ put a kick-off dinner Saturday night at the Magnolia Inn attended by more than ISO people. -

Saving Seabiscuit: an Argument for the Establishment of a Federal Equine Sports Commission
Volume 28 Issue 1 Article 4 2-3-2021 Saving Seabiscuit: An Argument for the Establishment of A Federal Equine Sports Commission Celso Lucas Leite,Jr. Follow this and additional works at: https://digitalcommons.law.villanova.edu/mslj Part of the Animal Law Commons, Entertainment, Arts, and Sports Law Commons, Gaming Law Commons, Legislation Commons, and the State and Local Government Law Commons Recommended Citation Celso L. Leite,Jr., Saving Seabiscuit: An Argument for the Establishment of A Federal Equine Sports Commission, 28 Jeffrey S. Moorad Sports L.J. 135 (2021). Available at: https://digitalcommons.law.villanova.edu/mslj/vol28/iss1/4 This Comment is brought to you for free and open access by Villanova University Charles Widger School of Law Digital Repository. It has been accepted for inclusion in Jeffrey S. Moorad Sports Law Journal by an authorized editor of Villanova University Charles Widger School of Law Digital Repository. \\jciprod01\productn\V\VLS\28-1\VLS104.txt unknown Seq: 1 25-JAN-21 12:07 Leite,Jr.: Saving Seabiscuit: An Argument for the Establishment of A Federal SAVING SEABISCUIT: AN ARGUMENT FOR THE ESTABLISHMENT OF A FEDERAL EQUINE SPORTS COMMISSION I. DEATH ON THE TRACK In January 2020, three horses died in three days at the Santa Anita racetrack in Arcadia, California.1 Racing officials euthanized the horses following the accidents at the track, prompting fierce criticism from animal rights groups.2 These incidents added to a death toll of five horses in January 2020 and followed a cascade of fifty-six deaths -

BCRP Brochure 2021 Class
Boston Combined Residency Program This brochure describes the residency program as we assume it will -19 exist will in be JulyThe 2021, Pediatric by which time Residency authorities Training Program predict a vaccine to COVID of available. If thatBoston is not the Children’s case and the Hospital pandemic is still active, the program Harvard Medical School will be very similar but many of the and educational conferences and other group activities Bostonwill be virtual Medical instead Center Boston University School of Medicine of in-person, as they are today. August 2020 edi,on CLASS OF 2021.. BOSTON COMBINED RESIDENCY PROGRAM Boston Medical Center Boston Children’s Hospital CONTENTS History…………........................... 3 Rotation # descriptions.................. 47# Global health fellowships............ 84# BCRP…........................................ 3# Night call................................... 53# Global health grants………….… 84 # Boston Children’s Hospital........... 3# Longitudinal ambulatory.............. 54# Diversity and Inclusion................. 84# Boston Medical Center................. 8# Electives………………………….. 55# Salaries and benefits.................... 87# People……................................... 11 Individualized curriculum............ 56# Child care................................... 88# Program director biosketches...... 11# Academic development block.. 56# O$ce of fellowship training....... 88# Residency program leadership..... 12# Education.................................... 57# Cost of living.............................. -

Celebrating 25 Years of Trooper Camaraderie
Volume 23, Issue 1 Winter 2014 Celebrating 25 years of trooper camaraderie AAST serves, connects troopers for quarter century Twenty-five years ago, a small group Today AAST can do more than merely mail of Florida state troopers had the vision letters to its members to notify them of needs to create an association that would unite in the trooper family. state troopers across the country and When AAST learns that a trooper has an assist them by providing valuable benefits extreme need – a job-related injury, a long- and services. term illness, loss from a natural disaster, Thus was born the American Association an ill child – AAST has the capability of of State Troopers. e-mailing its members with the quick click Thousands of state troopers have been of a button and calling them to action. Tens first-hand recipients of AAST benefits: of thousands of dollars have been sent in scholarships for their children, insurance, from concerned troopers to help their fel- donations from AAST’s Brotherhood Assis- low troopers in need. The thin blue line tance Fund, and donations sent from their knows no state boundaries. fellow state troopers around the country. In November 2010, 2-year-old Wyatt Bai- ley, son of Tpr. Jason It is humbling, to say the least, to be Bailey of the Idaho State Police was diagnosed a recipient of such an outpouring with lymphoid nodular hyperplasia, a serious of support and brotherhood. digestive disorder. Not Tpr. John Ollquist, after Hurricane Sandy struck his home only did AAST send a Brotherhood Assistance AAST’s most highly touted benefit donation, but troopers around the country since its inception in 1989 has been its sent a staggering $12,647 to help little Wyatt. -

GOP Leaders Seek to Bar Floor Fight
ion SEESTpHYBEMW FINAL Sunny and warm today, Red Bank, Freehold clear tonight. Tomorrow mostly sunny and very warm. long Branch EDITION Monmouth County's Outstanding Home Newspaper PAGES VOL.SS' NO.4O RED BANK, N.J. MONDAY, AUGUST 21,1972 TEN CENTS IUIIHIIIII iiiiiiirniiinrniiniiiiiiiiiiiiiiiiiiiMiiuuiiiiuiniuiuuiiiuiniiiiiiuuiiiuiriiiiiiiiiiiiiiiiiiuiiininiiiiiiiiiiiiiiiitiiiiniiiiiniiiiiiiiiitiiiiiiuniiuiniiiiinniiu State Weighs Easing Records* Secrecy By HENRY GOTTLIEB for the first time by State statute should be changed in with tbe state Health Depart- One of the state regulations He said the review would Kugler has invited the state Kugler would not comment ud Atty. Gen. George F. Kugler some fashion," Kugler said. ment's refusal to release re- to be scrutinized is an execu- take "a couple of months." Investigation Commission to on the Sherwin investigation, TOMTOOLEN Jr. in an interview with mem- Kugler said the review was ports about food estab- tive order promulgated in 1963 The interview was one of investigate the cover-up alle- but he defended bis office's AP-Record Strike Force bers of an Associated Press- sparked by a landmark state lishments with poor sanitary that allows heads of state the few Kugler has granted gations and had asked the reputation as a force against Record of Hackensack strike Supreme Court decision fore-' conditions. agencies to decide what docu- since New Jersey Secretary of. state Supreme Court to ap- crime. He said the federal TRENTON - A massive re- force investigating secrecy in ing the Public Utilities Com- Kugler said the public ments are public and what State Paul J. Sherwin was in- point a special prosecutor to government's crime fighting view is under way that may state government. -

Baby Parade Renewal Draws 50,000 Watergate Seen Damaging to Both
Baby Parade Renewal Draws 50,000 uSEESTORYPAGE t.14 ^MMAtkU 3 The Weather Hazy, hot and humid today FINAL and tomorrow, highs in low to mid-90s. Fair and warm EDITION tonight,' F^REGISTER llonmouth County's Outstanding Homo Newspaper 24 PACES VOL.96 NO.lt TEN CKNTS RED UANk-MIUDI.KTOWN, N.J. SUNDAY, AUGUST 27,1973 iiimiinimi niiiitiiMiiiiniHiiiii IIIIUIIIIIIIIinilllllllllllMUHIHIIIIIIIIIMIinillHU IIIMUIIIIIIIIIIIUIIIIIIIIIIIIIIUIIIIIIII Watergate Seen Damaging to Both Parties By JIM ADAMS assessment that Watergate State Sen. Robert E. Bauman. going to vote against me to all politicians are crooks. .It Republican leader, GOP Con- they're making a big mis- a Republican without being scandal will have negative ef- Hauman, a conservative, get back at President Nixon seems to me this is just part ference Chairman John B. An- take." with that crowd." Parris stressed to every WASHINGTON (AP)— fects on both parties. narrowly defeated a con- or the bad things that have of the whole rotten system. derson of Illinois, says Water- Bauman, Peyser and Parris Three Republican politicians But they are inclined to be- servative Democratic oppo- been done," Bauman said be- But it's nothing new. They gate will severely damage Re- group he talked to that he arc pinning their hopes of not plans to introduce a bill in out among the voters last lieve that it will hurt Republi- nent last week to fill an unex- fore last week's election. talk about Watergate: what publicans. being scarred by either Wa- week have come up with the Bauman's district has sent Congress to repeal wage-price cans more. -

Prospective Students See Academia In
The WALRUS The time has come, the Walrus said, to talk of many things: Of shoes and ships and sealing wax, of cabbages and kings. - Lewis Carroll Vol LXVII, No. 3 St. Sebastian’s School December 2013 New Yearbook: Beauty to Behold By JACKSON McKEIGUE ‘17 my AP Stats guys, cause they gave me Fachetti placed on his page the quote by The release of the yearbook is a hard time last year.” Mr. Morelli also Neutral Milk Hotel, “How strange it is a highlight of every year. Whether it is explains the significance of being chosen to be anything at all.” Other mention- over the commotion of the past seniors by the senior class and what it means to able quotations, include Joe Cough- returning, or the laughs everyone gets out him specifically. He began to talk about lin’s chosen excerpt by Jimmy Tatro, of last years pictures, it is always a fun winning the money at the raffle and how “Someone once told me it’s a marathon, time getting the yearbook. Last year’s great of a feeling it was, but he compared not a sprint. I sprint marathons, simple as installment was one of the best books this his honor of being chosen to the money that.” Another quotation that was pointed school has seen in a long time, according and said, “The money goes away, very out by many students, as they relate it to to a number of different, veteran faculty. quickly, but something like that means one of the all time greatest movies this After the 2012 book was released it was a lot coming from kids you taught, and world has come to know, Forrest Gump.