Pacific Population Health Profile
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Regional Overview
Air, land and water in the Wellington region – state and trends Regional overview This summary highlights the key findings from State of the Environment monitoring we carry out of natural resources across the Wellington region. It is drawn from eight technical reports which give the full picture of the health of the Wellington region’s air, land, fresh waters and coast. The reports, published every five years, are based on environmental monitoring and investigations over the past five to ten years (and longer for some resources). The findings are informing the current review of Greater Wellington’s regional plans – the ‘rule books’ for ensuring our region’s natural resources are sustainably managed. These plans are now more than ten years old and we are developing a new integrated plan. Community input to the review is critical – you can find out how to have a say on the back page. How do we measure the health of the region’s air, land and water resources? Regional councils have a legal responsibility under section 35 of the Resource Management Act 1991 to monitor the state of the environment – this essentially means tracking the quality and quantity of the region’s natural resources over time. Greater Wellington does this through long-term monitoring programmes across the region focusing on: ● Air quality at 6 locations ● Soil quality (118 sites under a range of different land uses) and stability ● Rainfall (at 50 sites) and river flows/levels (at 45 sites) ● Groundwater levels (at 146 sites) and quality (at 71 sites) ● Water quality at popular river and beach recreation spots (100 sites) ● River/stream water quality and ecosystem health (at 55 sites) ● The health of selected estuaries and our two harbours Measuring river flow We also carry out short-term investigations where our routine monitoring identifies gaps or potential problems, such as poor air or water quality. -
Foton International
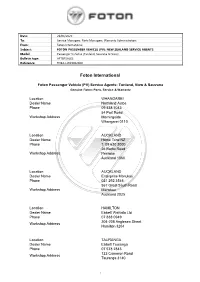
Date: 23/06/2020 To: Service Managers, Parts Managers, Warranty Administrators From: Foton International Subject: FOTON PASSENGER VEHICLE (PV): NEW ZEALAND SERVICE AGENTS Model: Passenger Vehicles (Tunland, Sauvana & View) Bulletin type: AFTERSALES Reference: FDBA-LW23062020 Foton International Foton Passenger Vehicle (PV) Service Agents: Tunland, View & Sauvana Genuine Foton: Parts, Service & Warranty Location WHANGAREI Dealer Name Northland Autos Phone 09 438 7043 54 Port Road Workshop Address Morningside Whangarei 0110 Location AUCKLAND Dealer Name Home Tune NZ Phone T: 09 630 3000 26 Botha Road Workshop Address Penrose Auckland 1060 Location AUCKLAND Dealer Name Enterprise Manukau Phone 021 292 3546 567 Great South Road Workshop Address Manukau Auckland 2025 Location HAMILTON Dealer Name Ebbett Waikato Ltd Phone 07 838 0949 204-208 Anglesea Street Workshop Address Hamilton 3204 Location TAURANGA Dealer Name Ebbett Tauranga Phone 07 578 2843 123 Cameron Road Workshop Address Tauranga 3140 1 Location ROTORUA Dealer Name Grant Johnstone Motors Phone 07 349 2221 24-26 Fairy Springs Road Workshop Address Fairy Springs Rotorua 2104 Location TAUPO Dealer Name Central Motor Hub Phone 022 046 5269 79 Miro Street Workshop Address Tauhara Taupo 3330 Location GISBORNE Dealer Name Enterprise Motors Phone 06 867 8368 323 Gladstone Rd Workshop Address Gisborne 4010 Location HASTINGS Dealer Name The Car Company Phone 06 870 9951 909 Karamu Road North Workshop Address Hastings 4122 Location NEW PLYMOUTH Dealer Name Ross Graham Motors Ltd Phone 06 -

Porirua Harbour Intertidal Fine Scale Monitoring 2008/9
Wriggle coastalmanagement Porirua Harbour Intertidal Fine Scale Monitoring 2008/09 Prepared for Greater Wellington Regional Council June 2009 Porirua Harbour Intertidal Fine Scale Monitoring 2008/09 Prepared for Greater Wellington Regional Council By Barry Robertson and Leigh Stevens Cover Photo: Upper Pauatahanui Arm of Porirua Harbour from mouth of Pautahanui Stream. Wriggle Limited, PO Box 1622, Nelson 7040, Ph 0275 417 935, 021 417 936, www.wriggle.co.nz Wriggle coastalmanagement iii Contents Porirua Harbour 2009 - Executive Summary . vii 1. Introduction . 1 2. Methods . 4 3. Results and Discussion . 8 4. Conclusions . 15 5. Monitoring ���������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������� 15 6. Management ������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������ 15 8. References ���������������������������������������������������������������������������������������������������������������������������������������������������������������������������������������� 16 Appendix 1. Details on Analytical Methods �������������������������������������������������������������������������������������������������������������������������������� 17 Appendix 2. 2009 Detailed Results . 17 Appendix 3. Infauna Characteristics . 23 List of Figures Figure 1. Location of sedimentation and fine scale monitoring -

Activity of Birds in the Western Hutt Hills, New Zealand
Notornis, 2000, Vol. 47: 13-35 0029-4470 0 The Ornithological Society of New Zealand, Inc. 2000 Activity of birds in the Western Hutt Hills, New Zealand JOHN A. GIBB 3 Wairere Road, Lower Hun, New Zealand j.gibb@ c1ea~net.n~ Abstract This paper describes the activity of garden, bush and riverine birds in the Western Hutt hills, 1981-92. The area is 15 km north of Wellington, 7 !an north of the Hutt River estuary, and 15 !an south of Pauatahanui Inlet, Porirua Harbour, on the southwest coast of the North Island. Observation is based on 35 years' residence and >12 500 10-min counts conducted between 1981 and 1992. Species first seen each day are distinguished from those first heard. Whenever possible the birds' food was recorded. The western hills have fewer native passerines than similar habitat on the eastern hills. Several species increased or decreased during the study. Some apparent decline was attributed to the author's hearing loss. Wind reduced bird detection. Nectar of New Zealand flax (Phormium spp.) was eaten by silvereyes (Zosterops lateralis),tui (Prosthemaderanovaeseelandiae) and starlings (Sturnus vulgaris) at different times. In the study area there were about 0.9 cats (Felis catus) per household, a potential predator on birds. Gibb, J.A. 2000. Bird activity in the Western Hutt Hills, Wellington, New Zealand. Notornis 47(1): 13-35. Keywords bird activity; detection; counts; garden; forest; river; food; voice; house cats INTRODUCTION hills (41°12'S, 174'55'E), is 150 m. a.s.l., 15 krn north I began this study because I was curious how birds used of Wellington, 7 km north of the Hutt River estuary, and the habitat between Lower Hutt city and bush along the 15 krn south of Pauatahanui at the head of Porirua Harbour Western Hutt hills. -

Caring Deception : Community Art in the Suburbs of Aotearoa
Copyright is owned by the Author of the thesis. Permission is given for a copy to be downloaded by an individual for the purpose of research and private study only. The thesis may not be reproduced elsewhere without the permission of the Author. Caring Deception: Community art in the suburbs of Aotearoa (New Zealand) A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy in Fine Arts at Massey University, Wellington, New Zealand. By Tim Barlow 2016 2 Abstract In Aotearoa (New Zealand), community art practice has a disadvantaged status and a poorly documented national history. This thesis reinvigorates the theory and practice of community art and cultural democracy using adaptable and context-specific analyses of the ways that aesthetics and ethics can usefully co-exist in practices of social change. The community art projects in this thesis were based in four suburbs lying on the economic and spatial fringes of Aotearoa. Over 4 years, I generated a comparative and iterative methodology challenging major binaries of the field, including: ameliorative vs. disruptive; coloniser vs. colonised; instrumental vs. instrumentalised; and long term vs. short term. This thesis asserts that these binaries create a series of impasses that drive the practice towards two new artistic categories, which I define as caring deception and the facade. All the projects I undertook were situated in contested space, where artists working with communities overlapped with local and national governments aiming for CBD and suburban re-vitalisation, creative city style initiatives, community development, grassroots creative projects, and curated public-art festivals. -

Infill Housing: Intensification and the District Plan
Intensification and the District Plan Issues and Options for Facilitating and Managing Intensive Residential Development in Wellington City Final Report December 2007 Project name: Intensification and the District Plan – Issues and Options for Wellington City Document 1574 reference: Date of this December 2007 version: Status of report: Final Report prepared David Mead – Director by: Report reviewed Andrew Macleod – Senior Consultant by: Hill Young Cooper Ltd Hill Young Cooper Ltd Level 4, 128 Broadway Level 3, AMP Chambers PO Box 99847 187 Featherston Street Newmarket PO Box 8092, The Terrace Auckland 1149 Wellington 6143 p: 09 529 2684 p: 04 473 5310 f: 09 520 4685 f: 04 473 5307 e: [email protected] e: [email protected] Table of Contents 1 INTRODUCTION .............................................................................................................1 1.1 The Purpose of the Project ............................................................................................... 1 1.2 Background to the Project ................................................................................................ 2 1.3 Methodology ................................................................................................................. 2 1.3.1 Structure of the Report .................................................................................................... 3 2 THE WELLINGTON CONTEXT - AREAS OF CHANGE ................................................4 2.1 Possible areas of redevelopment ...................................................................................... -

Kapiti Coast District Council and Other Councils, Including Population Forecasts
Housing and Business Development Capacity Assessment Kāpiti Coast District Council November 2019 Housing and Business Land Capacity Assessment 229 230 Housing and Business Land Capacity Assessment Contents Executive Summary 232 5.0 Infrastructure 270 Background 233 5.1 Three Waters 270 Residential demand 233 5.2 Local Road Network 271 Residential capacity 233 5.3 State Highway Network 272 Business demand 234 5.4 Public Transport 272 Business capacity 234 5.5 Open Space 273 Infrastructure capacity 234 5.6 Education 273 1.0 Introduction 237 6.0 Relationship between Housing and Business Land 274 2.0 Existing Policy Context 238 7.0 Monitoring 275 2.1 Kāpiti Coast District Plan 238 7.1 Historic Development Activity 275 2.2 Development Management Strategy 2007 238 7.2 Market Indicators 278 2.3 Infrastructure Strategy 2018-2048 238 7.3 Price Efficiency Indicators 285 2.4 Roads of National Significance and Town Centres Transformation 239 8.0 Conclusion 293 3.0 Residential Demand and Capacity 240 9.0 Next Actions 294 3.1 Historic urban growth and settlement 240 3.2 Current growth and settlement trends 240 3.3 Future Housing Demand 241 3.4 Housing Development Capacity 248 3.5 Housing Feasibility, Realisation and Sufficiency 251 4.0 Business Demand and Capacity 258 4.1 Business Development Context 258 4.2 Current Economic and Business Drivers 259 4.3 Future Business Demand 260 4.4 Business Development Capacity 264 4.5 Business Feasibility, Realisation and Sufficiency 266 Housing and Business Land Capacity Assessment 231 Executive Summary This report presents the results from the Wellington Region Housing and Business Development Capacity Assessment (HBA) for the Kāpiti Coast District Council. -
Secondary Schools of New Zealand
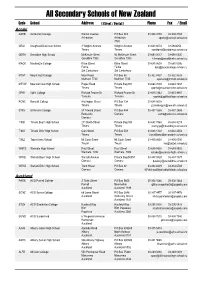
All Secondary Schools of New Zealand Code School Address ( Street / Postal ) Phone Fax / Email Aoraki ASHB Ashburton College Walnut Avenue PO Box 204 03-308 4193 03-308 2104 Ashburton Ashburton [email protected] 7740 CRAI Craighead Diocesan School 3 Wrights Avenue Wrights Avenue 03-688 6074 03 6842250 Timaru Timaru [email protected] GERA Geraldine High School McKenzie Street 93 McKenzie Street 03-693 0017 03-693 0020 Geraldine 7930 Geraldine 7930 [email protected] MACK Mackenzie College Kirke Street Kirke Street 03-685 8603 03 685 8296 Fairlie Fairlie [email protected] Sth Canterbury Sth Canterbury MTHT Mount Hutt College Main Road PO Box 58 03-302 8437 03-302 8328 Methven 7730 Methven 7745 [email protected] MTVW Mountainview High School Pages Road Private Bag 907 03-684 7039 03-684 7037 Timaru Timaru [email protected] OPHI Opihi College Richard Pearse Dr Richard Pearse Dr 03-615 7442 03-615 9987 Temuka Temuka [email protected] RONC Roncalli College Wellington Street PO Box 138 03-688 6003 Timaru Timaru [email protected] STKV St Kevin's College 57 Taward Street PO Box 444 03-437 1665 03-437 2469 Redcastle Oamaru [email protected] Oamaru TIMB Timaru Boys' High School 211 North Street Private Bag 903 03-687 7560 03-688 8219 Timaru Timaru [email protected] TIMG Timaru Girls' High School Cain Street PO Box 558 03-688 1122 03-688 4254 Timaru Timaru [email protected] TWIZ Twizel Area School Mt Cook Street Mt Cook Street -

PUBLIC AGENDA V.2 Held on Wednesday 3 March Location: Hutt Hospital, Level 1, Clock Tower Building, Auditorium Room Zoom: 876 5068 1844 Time: 9.30Am MEETING
3 March PUBLIC Concurrent Board Meeting - Agenda PUBLIC AGENDA v.2 Held on Wednesday 3 March Location: Hutt Hospital, Level 1, Clock Tower Building, Auditorium Room Zoom: 876 5068 1844 Time: 9.30am MEETING Item Action Presenter Min Time Pg 1 PROCEDURAL BUSINESS 1.1 Karakia All members 1.2 Apologies ACCEPT Chair Public Participation 1.3 VERBAL Public - Nil Continuous Disclosure 1.4 1.4.1 Combined Board Interest Register ACCEPT Chair 1.4.2 Combined ELT Interest Register 15 9:30am 1.5 Minutes of Previous Concurrent Meeting ACCEPT Chair Matters Arising from Previous Concurrent 1.6 NOTE Chair Meetings 1.7 Chair’s Report and Correspondence NOTE Chair 1.8 Chief Executive’s Report NOTE Chief Executive Board Work Plan 2021 1.9 DISCUSS Chair 20 9:45am 1.9.1 Detailed Work Plan 2 DHB Performance and Accountability 2.1 HVDHB October 2020 Financial and NOTE Chief Financial Officer 10 10.05am Operational Performance Report Director Provider Services 2.1.1 Report 2.2 CCDHB October 2020 Financial and NOTE Chief Financial Officer Operational Performance Report Director Provider Services 2.2.1 Report 3 Updates 3.1 HSC Update and Items for Approval NOTE Chair of HSC 20 10.15am 4 OTHER 4.1 General Business NOTE Chair 5 10.35am 4.2 Resolution to Exclude the Public ACCEPT Chair 11:00 am - MORNING TEA – 15 min DATE OF NEXT FULL BOARD MEETING: 7 April 2021, Zoom: 876 5068 1844, Location: Wellington Regional Hospital, Level 11 Boardroom Grace Neil Block Hutt Valley and Capital & Coast District Health Boards Page 1 December 2020 1 3 March PUBLIC Concurrent Board -

PLIMMERTON FARM SUBMISSION | K BEAMSLEY Page 1
PLIMMERTON FARM – PLAN CHANGE PROPOSAL Supporting Documentation View from Submitters Property Karla and Trevor Beamsley 24 Motuhara Road Plimmerton PLIMMERTON FARM SUBMISSION | K BEAMSLEY Page 1 1. INTRODUCTION The village of Plimmerton is a northern suburb of Porirua, and is surrounded to the North and East by farmland. It represents the edge of existing residential dwellings. Generally existing homes are stand-alone dwellings on lots greater than 500m² in size. Most residents within Plimmerton and Camborne either commute into Wellington city or work from home. The demand for housing in this area is from professional couples or families looking for 3 – 4 bedroom family homes on a section with space for kids to run around in, not medium or high density three-storey buildings and apartments, this is reflected in the TPG report to PCC (Dec 2019). Medium density style townhouses, or apartments would be totally out of character of the surrounding residential areas, and would present a stark contrast to the remaining rural areas which bound the site. The Plimmerton Farm site is not located close to areas of high employment, nor is it close to local amenities like the main shopping areas of Porirua. The site is also not located within an area currently supported by existing infrastructure. Much of the infrastructure in the area is aging, and requires repair or upgrade to support existing demands. Therefore, the idea that Plimmerton Farm would provide homes in a location close to employment, amenities and infrastructure1 is simply incorrect in terms of a 10-year time frame. Areas where this would be true include the currently developing areas of Aotea, Whitby, Kenepuru, and Porirua East. -
2015 Sunday Festival Report and Survey Results
2015 Sunday Festival Report and Survey Results CONTENTS 1.0 INTRODUCTION ..................................................................................................................... 3 2.0 BACKGROUND ....................................................................................................................... 3 3.0 PURPOSE ................................................................................................................................ 3 4.0 FESTIVAL PROFILE .................................................................................................................. 4 5.0 SURVEY METHODOLOGY ..................................................................................................... 11 6.0 FINDINGS ............................................................................................................................. 12 Who came to Te Rā? ...................................................................................................... 12 Where did people at Te Rā festival come from? ............................................................ 13 How did people hear about Te Rā? ................................................................................ 14 What the Te Rā festival means for those who came...................................................... 14 What did people think of Te Rā 2015? ........................................................................... 16 Entertainment, hauora and mātauranga tents and the youth zone .............................. 17 Stalls food -

Employment Analysis Report
Employment Analysis October 2020 Wellington Regional Growth Framework | 0 Introduction Ka ora te wai If the water is healthy Purpose of this report More detailed work, than has been undertaken in the Ka ora te whenua the land will be nourished The purpose of this report is to summarise existing Framework, will need to be undertaken to Ka ora te whenua If the land is nourished research and data to assist with regional spatial understand in more detail: Ka ora te tangata the people will be provided planning. No new analysis has been undertaken. This 1. How many jobs do we expect in each for report should be read as an input into other work, geographical area as of 2050? and not as a final conclusion on the spatial direction 2. What change is that from the current situation? for the Framework or as policy for any of the partner Mo te iti - mo te rahi For the little - for the large 3. What type of jobs are they? organisations. 4. What do we need to do to make this change? 1 As outlined in the Foundation Report for the This report builds upon the Foundation Report to Wellington Regional Growth Framework (the 2 provide background information to assist in analysing Framework), employment in the region is employment patterns and information and concentrated in central Wellington and a significant determine what changes may/could occur with number of commuters travel into central Wellington regards to employment and the Framework. from other parts of the region for employment. A key direction during development of the Regional employment is dominated by knowledge- Framework with regards to employment has been to based sector employment.